Beyond Trial and Error: Advanced Strategies for Optimizing Model Refinement of Low-Accuracy Targets
This article provides a comprehensive guide for researchers and drug development professionals on refining computational and biological models with initially low accuracy.
Beyond Trial and Error: Advanced Strategies for Optimizing Model Refinement of Low-Accuracy Targets
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on refining computational and biological models with initially low accuracy. It explores the foundational challenges, presents cutting-edge methodological workflows like genetic algorithms and machine learning-based refinement, offers troubleshooting strategies to overcome common pitfalls, and details robust validation frameworks. By integrating insights from recent advances in fields ranging from genomics to quantitative systems pharmacology, this resource aims to equip scientists with the tools to enhance predictive accuracy, generate testable hypotheses, and accelerate the translation of models into reliable biomedical insights.
The Low-Accuracy Challenge: Diagnosing the Root Causes in Biological Models
In both drug discovery and systems biology, the selection and validation of biological targets are foundational to success. However, these fields are persistently plagued by the challenge of low-accuracy targets, leading to high failure rates and inefficient resource allocation. In clinical drug development, a staggering 90% of drug candidates fail after entering clinical trials [1]. The primary reasons for these failures are a lack of clinical efficacy (40-50%) and unmanageable toxicity (30%) [1]. Similarly, in systems biology modelling, a systematic analysis revealed that approximately 49% of published mathematical models are not directly reproducible due to incorrect or missing information in the manuscript [2]. This article explores the root causes of these low-accuracy targets and provides a technical troubleshooting guide for researchers seeking to overcome these critical challenges.
Quantitative Data on Failure Rates
The tables below summarize key quantitative data on failure rates and reasons across drug discovery and computational modeling.
Table 1: Reasons for Clinical Drug Development Failures (2010-2017 Data)
| Reason for Failure | Percentage of Failures |
|---|---|
| Lack of Clinical Efficacy | 40% - 50% |
| Unmanageable Toxicity | 30% |
| Poor Drug-Like Properties | 10% - 15% |
| Lack of Commercial Needs / Poor Strategic Planning | 10% |
Table 2: Reproducibility Analysis of 455 Published Mathematical Models
| Reproducibility Status | Number of Models | Percentage of Total |
|---|---|---|
| Directly Reproducible | 233 | 51% |
| Reproduced with Manual Corrections | 40 | 9% |
| Reproduced with Author Support | 13 | 3% |
| Non-reproducible | 169 | 37% |
Table 3: Genetic Evidence Support and Clinical Trial Outcomes
| Trial Outcome Category | Association with Genetic Evidence (Odds Ratio) |
|---|---|
| All Stopped Trials | Depleted (OR = 0.73) |
| Stopped for Negative Outcomes (e.g., Lack of Efficacy) | Significantly Depleted (OR = 0.61) |
| Stopped for Safety Reasons | Associated with highly constrained target genes and broad tissue expression |
| Stopped for Operational Reasons (e.g., COVID-19) | No significant association |
Troubleshooting Guide: FAQs on Low-Accuracy Targets
FAQ 1: Why do our drug candidates repeatedly fail in clinical trials due to lack of efficacy, despite promising preclinical data?
Issue: This is the most common failure, accounting for 40-50% of clinical trial stoppages [1]. A primary cause is often inadequate target validation and poor target engagement [3].
Troubleshooting Steps:
- Strengthen Genetic Evidence: Retrospective analyses show that clinical trials are less likely to stop for lack of efficacy when there is strong human genetic evidence supporting the link between the drug target and the disease. Trials halted for negative outcomes show a significant depletion of such genetic support (Odds Ratio = 0.61) [4]. Before target selection, consult genetic databases (e.g., Open Targets Platform) to assess this evidence.
- Implement STR and STAR Profiling: Move beyond the traditional focus on Structure-Activity Relationship (SAR). Integrate Structure-Tissue Exposure/Selectivity Relationship (STR) and the comprehensive Structure–Tissue Exposure/Selectivity–Activity Relationship (STAR) [1]. A drug may be potent but fail if it does not reach the target tissue in sufficient concentration (a Class II drug), while another with adequate potency but high tissue selectivity (Class III) might be overlooked but succeed [1].
- Verify Target Engagement in Physiologically Relevant Conditions: Use advanced techniques like the Cellular Thermal Shift Assay (CETSA) to confirm that your drug candidate actually binds to and engages the intended target in intact cells or tissues, preserving physiological conditions [3]. This helps move beyond artificial, purified protein assays.
FAQ 2: How can we reduce late-stage failures due to unmanageable toxicity?
Issue: Toxicity accounts for 30% of clinical failures and can stem from both on-target and off-target effects [1] [4].
Troubleshooting Steps:
- Analyze Target Gene Properties: Trials stopped for safety reasons are associated with drug targets that are highly constrained in human populations (indicating intolerance to functional genetic variation) and that are broadly expressed across tissues [4]. Prioritize targets with more selective expression profiles.
- Employ Forward vs. Reverse Chemical Genetics:
- Reverse Chemical Genetics: Start with a purified protein target, screen for binders/inhibitors, and then characterize the phenotype in cells/animals. This risks selecting compounds that are optimized for an artificial system [5].
- Forward Chemical Genetics: Start with a phenotypic screen in a disease-relevant cell or animal model to find compounds that produce the desired effect, then work to identify the protein target(s). This "pre-validates" the target in a physiological context but requires effective target deconvolution [5].
- Investigate Polypharmacology: Use unbiased affinity purification and proteomic profiling methods to identify off-target protein interactions that could contribute to toxicity [5]. Understanding a compound's full interaction profile is crucial for optimizing selectivity.
FAQ 3: Why are our computational models and predictions, such as for synthetic lethality, often inaccurate and not reproducible?
Issue: Computational models in systems biology often fail to accurately predict biological outcomes, such as synthetic lethal gene pairs, with one study showing accuracy between only 25-43% [6]. Furthermore, nearly half of all published models are not reproducible [2].
Troubleshooting Steps:
- Systematically Address Reproducibility: Follow an 8-point reproducibility scorecard for model creation and reporting [2]. The most common reasons for non-reproducible models are missing parameter values, missing initial conditions, and inconsistencies in model structure (e.g., errors in equations) [2].
- Automate Model Refinement: For network-based dynamic models (e.g., Boolean models), leverage tools like boolmore, a genetic algorithm-based workflow that automatically refines models to better agree with a corpus of perturbation-observation experimental data [7]. This can streamline the laborious manual process of trial-and-error refinement.
- Identify and Rectify Common Failure Modes: When a model prediction fails, systematically check for:
Issue: The drug discovery process is prolonged and costly, with the preclinical phase alone taking 3-6 years [8].
Troubleshooting Steps:
- Centralize Data Management: Implement centralized data management software (e.g., a LIMS or ELN) to break down data silos, reduce manual entry errors, and provide a unified view of research activities, enabling real-time informed decisions [8].
- Optimize Experimental Design: Use customizable templates for standardized experimental protocols to ensure consistency and data integrity. Identify Critical Process Parameters (CPPs) and Quality Attributes (CQAs) early to strengthen protocols [8].
- Enhance Collaboration: Utilize platforms that offer real-time notifications, simultaneous document editing, and robust project tracking to keep cross-functional teams (chemistry, biology, pharmacology) aligned and to identify bottlenecks early [8].
Experimental Protocols for Key Validation Experiments
Protocol 1: Assessing Target Engagement Using CETSA
Purpose: To quantitatively measure the engagement of a drug molecule with its protein target in intact cells under physiological conditions [3].
Methodology:
- Cell Treatment: Incubate intact cells with the drug candidate or a vehicle control.
- Heat Challenge: Subject the cell aliquots to a range of elevated temperatures. When a drug binds to a target protein, it often stabilizes the protein, increasing its thermal stability.
- Cell Lysis and Protein Solubilization: Lyse the heated cells and separate the soluble (non-denatured) protein from the insoluble (aggregated) protein.
- Target Protein Quantification: Detect and quantify the amount of soluble target protein remaining in each sample using a specific detection method, such as immunoblotting or a target-specific assay.
- Data Analysis: The difference in thermal stability of the target protein between drug-treated and untreated samples is a direct indicator of target engagement.
Protocol 2: Automated Model Refinement with Boolmore
Purpose: To streamline and automate the refinement of a Boolean network model to improve its agreement with experimental data [7].
Methodology:
- Inputs:
- Starting Model: The initial Boolean model to be refined.
- Biological Mechanisms: Known biological constraints expressed as logical relations (e.g., "A is necessary for B").
- Perturbation-Observation Pairs: A curated compilation of experimental results, each describing the state of a node under a specific perturbation context.
- Genetic Algorithm Workflow:
- Mutation: The tool generates a population of new models by mutating the Boolean functions of the starting model, while preserving user-defined biological constraints and the structure of the starting interaction graph.
- Prediction: For each model, it calculates the long-term behaviors (minimal trap spaces) under each experimental setting.
- Fitness Scoring: It computes a fitness score for each model by quantifying its agreement with the compendium of experimental results.
- Selection: The models with the top fitness scores are retained for the next iteration.
- Output: A refined Boolean model with higher accuracy and new, testable predictions [7].
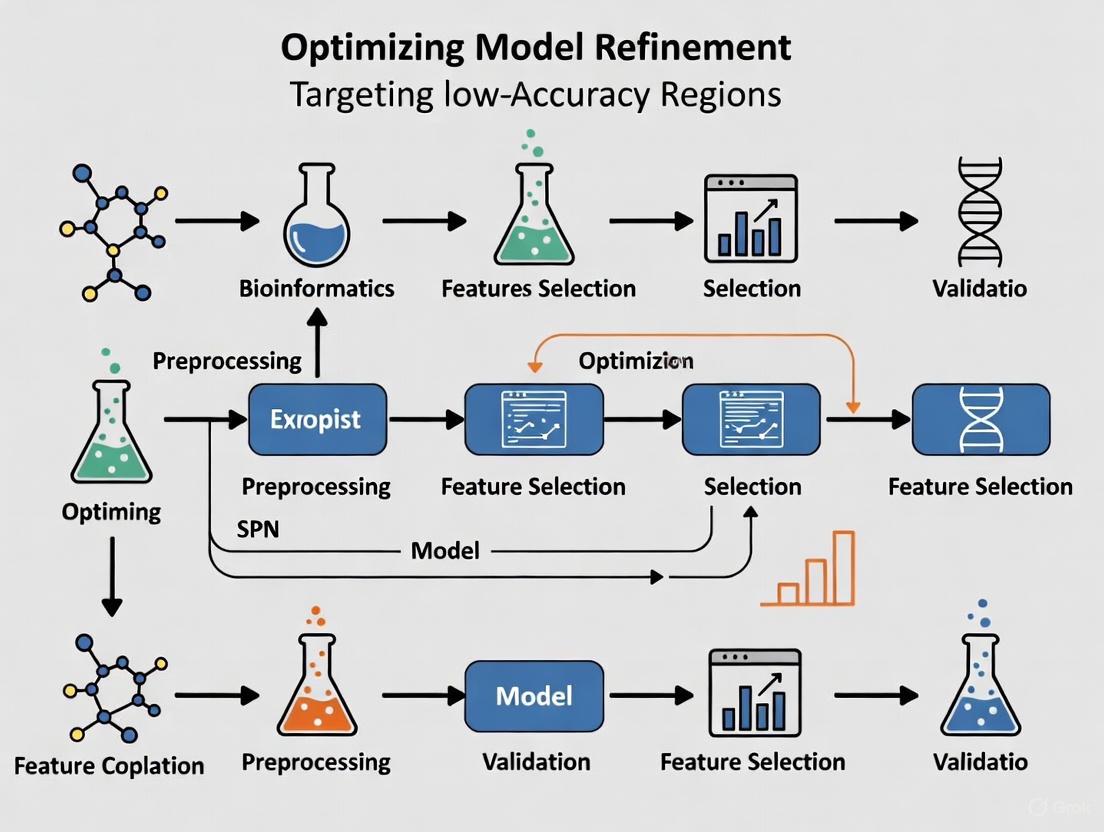
Visual Workflows and Signaling Pathways
Diagram 1: STAR-driven Drug Optimization Workflow
Diagram 2: Forward vs. Reverse Chemical Genetics
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Tools and Reagents
| Tool / Reagent | Function / Application |
|---|---|
| CETSA (Cellular Thermal Shift Assay) | A label-free method for measuring target engagement of small molecules with their protein targets directly in intact cells and tissues under physiological conditions [3]. |
| Boolmore | A genetic algorithm-based tool that automates the refinement of Boolean network models to improve agreement with experimental perturbation-observation data [7]. |
| Open Targets Platform | An integrative platform that combines public domain data to associate drug targets with diseases and prioritize targets based on genetic, genomic, and chemical evidence [4]. |
| BioModels Database | A public repository of curated, annotated, and peer-reviewed computational models, used for model sharing, validation, and reproducibility checking [2]. |
| LIMS & ELN Software | Centralized data management systems (Laboratory Information Management System and Electronic Lab Notebook) that streamline experimental tracking, inventory management, and collaboration [8]. |
| Affinity Purification Reagents | Chemical tools (e.g., immobilized beads, photoaffinity labels, cross-linkers) for the biochemical purification and identification of small-molecule protein targets and off-targets [5]. |
FAQs on Data Quality and Model Refinement
How can I identify which data points are most harmful to my model's accuracy?
You can use data valuation frameworks to identify harmful data points. The Data Shapley method provides a principled framework to quantify the value of each training datum to the predictor performance, uniquely satisfying several natural properties of equitable data valuation [9]. It effectively identifies helpful or harmful data points for a learning algorithm, with low Shapley value data effectively capturing outliers and corruptions [9]. Influence functions offer another approach, tracing a model's prediction through the learning algorithm back to its training data, thereby identifying training points most responsible for a given prediction [9]. For practical implementation, ActiveClean supports progressive and iterative cleaning in statistical modeling while preserving convergence guarantees, prioritizing cleaning those records likely to affect the results [9].
What should I do when my experimental results don't match expected outcomes?
Follow a systematic troubleshooting protocol. First, repeat the experiment unless cost or time prohibitive, as you might have made a simple mistake [10]. Second, consider whether the experiment actually failed - consult literature to determine if there's another plausible reason for unexpected results [10]. Third, ensure you have appropriate controls - both positive and negative controls can help confirm the validity of your results [10]. Fourth, check all equipment and materials - reagents can be sensitive to improper storage, and vendors can send bad batches [10]. Finally, start changing variables systematically, isolating and testing only one variable at a time while documenting everything meticulously [10].
How do I address mechanistic uncertainty in biological research?
Mechanistic uncertainty presents special challenges, particularly when causal inference cannot be made and unmeasured confounding may explain observed associations [11]. In such cases, consider that relationships may not be causal, or mechanisms may be indirect rather than direct [11]. For example, in ultraprocessed food research, it's unclear whether associations with health outcomes stem from macronutrient profiles, specific processing techniques, or displacement of health-promoting dietary patterns [11]. The Bayesian synthesis (BSyn) method provides one solution, offering credible intervals for mechanistic models that typically produce only point estimates [12]. This approach is particularly valuable when environmental conditions change and empirical models may be of limited usefulness [12].
Troubleshooting Guides
Guide 1: Diagnosing Data Quality Issues
Problem: Model performance is inconsistent or deteriorating despite apparent proper training procedures.
Diagnostic Steps:
- Run data attribution analysis: Use influence functions or Shapley values to identify problematic training points [9].
- Implement Confident Learning: Apply techniques to estimate uncertainty in dataset labels and characterize label errors [9].
- Check for data drift: Monitor whether incoming data maintains the same statistical properties as training data.
- Validate data preprocessing: Ensure consistency in normalization, handling of missing values, and feature engineering across training and deployment.
Solutions:
- Use ActiveClean for interactive data cleaning while preserving statistical modeling convergence guarantees [9].
- Apply Beta Shapley as a unified and noise-reduced data valuation framework to prioritize the most impactful data repairs [9].
- Establish automated data validation pipelines to detect anomalies before model retraining.
Guide 2: Addressing Mechanistic Uncertainty in Drug Development
Problem: Biological mechanisms underlying observed effects remain unclear, creating challenges for model refinement and validation.
Diagnostic Steps:
- Identify knowledge gaps: Map known mechanisms versus hypothesized pathways and their supporting evidence.
- Assess causal evidence: Distinguish between correlational relationships and established causal mechanisms.
- Evaluate alternative explanations: Systematically consider competing hypotheses that might explain observed results.
- Quantify uncertainty: Use Bayesian methods to provide credible intervals around mechanistic predictions [12].
Solutions:
- Implement Bayesian synthesis to quantify uncertainty in mechanistic models [12].
- Design targeted experiments to test specific mechanistic hypotheses rather than just outcome measures.
- Use model comparison frameworks to evaluate competing mechanistic explanations against experimental data.
- Apply sensitivity analysis to determine which uncertain parameters most affect model predictions.
Guide 3: Systematic Experimental Troubleshooting
Problem: Experiments produce unexpected results, high variance, or consistent failure despite proper protocols.
Diagnostic Steps:
- Apply the Pipettes and Problem Solving framework: This approach involves presenting unexpected experimental outcomes and systematically proposing new experiments to identify the source of problems [13].
- Categorize the problem type: Determine if it involves known outcomes returning atypical results (Type 1) or developing new assays/methods where the "right" outcome isn't known in advance (Type 2) [13].
- Consensus-driven hypothesis generation: Work collaboratively to reach consensus on proposed diagnostic experiments [13].
- Propose limited, sequential experiments: Typically limit to 2-3 proposed experiments before identifying the source of the problem [13].
Solutions:
- For Type 1 problems (atypical results with known expectations): Focus on fundamentals like appropriate controls, instrument calibration, and technique verification [13].
- For Type 2 problems (unknown right outcomes): Emphasize hypothesis development, proper controls, and new analytical techniques [13].
- Include seemingly mundane sources of error such as contamination, miscalibration, instrument malfunctions, and software bugs in your troubleshooting considerations [13].
- Document all troubleshooting steps meticulously for future reference and knowledge transfer [10].
Quantitative Error Analysis Framework
Table 1: Data Error Quantification Methods Comparison
| Method | Key Principle | Advantages | Limitations | Best Use Cases |
|---|---|---|---|---|
| Data Shapley [9] | Equitable data valuation based on cooperative game theory | Satisfies unique fairness properties; identifies both helpful/harmful points | Computationally expensive for large datasets | Critical applications requiring fair data valuation; error analysis |
| Influence Functions [9] | Traces predictions back to training data using gradient information | Explains individual predictions; no model retraining needed | Theoretical guarantees break down on non-convex/non-differentiable models | Model debugging; understanding prediction behavior |
| Confident Learning [9] | Characterizes label errors using probabilistic thresholds | Directly estimates joint distribution between noisy and clean labels | Requires per-class probability estimates | Learning with noisy labels; dataset curation |
| Beta Shapley [9] | Generalizes Data Shapley by relaxing efficiency axiom | Noise-reduced valuation; more stable estimates | Recent method with less extensive validation | Noisy data environments; robust data valuation |
| ActiveClean [9] | Interactive cleaning with progressive validation | Preserves convergence guarantees; prioritizes impactful cleaning | Limited to convex loss models (linear regression, SVMs) | Iterative data cleaning; budget-constrained cleaning |
Table 2: Troubleshooting Protocol for Common Experimental Issues
| Problem Type | Example Scenario | Diagnostic Experiments | Common Solutions |
|---|---|---|---|
| High Variance Results [13] | MTT assay with very high error bars and unexpected values | Check negative controls; verify technique (e.g., aspiration method); test with known compounds | Improve technical consistency; adjust protocol steps; verify equipment calibration |
| Unexpected Negative Results [10] | Dim fluorescence in immunohistochemistry | Repeat experiment; check reagent storage and compatibility; test positive controls | Adjust antibody concentrations; verify reagent quality; optimize visualization settings |
| Mechanistic Uncertainty [11] | Observed associations without clear causal mechanisms | Design controlled experiments to test specific pathways; assess confounding factors | Bayesian synthesis methods; consider multiple mechanistic hypotheses; targeted validation |
| Systematic Measurement Error [14] | Consistent bias across all measurements | Calibration verification; instrument cross-checking; reference standard testing | Equipment recalibration; protocol adjustment; measurement technique refinement |
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Error Reduction
| Reagent/Category | Function | Error Mitigation Role | Quality Control Considerations |
|---|---|---|---|
| Positive Controls [10] | Verify experimental system functionality | Identifies protocol failures versus true negative results | Should produce consistent, known response; validate regularly |
| Negative Controls [10] | Detect background signals and contamination | Distinguishes specific signals from non-specific binding | Should produce minimal/zero signal when properly implemented |
| Reference Standards | Calibrate instruments and measurements | Reduces systematic error in quantitative assays | Traceable to certified references; proper storage conditions |
| Validated Antibodies [10] | Specific detection of target molecules | Minimizes off-target binding and false positives | Verify host species, clonality, applications; check lot-to-lot consistency |
| Compatible Detection Systems [10] | Generate measurable signals from binding events | Ensures adequate signal-to-noise ratio | Confirm primary-secondary antibody compatibility; optimize concentrations |
Methodological Workflows
Data Error Identification Protocol
Data Error Identification and Mitigation Workflow
Systematic Experimental Troubleshooting
Systematic Experimental Troubleshooting Protocol
Mechanistic Uncertainty Resolution
Mechanistic Uncertainty Resolution Framework
Frequently Asked Questions (FAQs) on Model Refinement
Q1: What is the primary challenge of manual model refinement in systems biology? Manual model refinement is a significant bottleneck because it relies on a slow, labor-intensive process of trial and error, constrained by domain knowledge. For instance, refining a Boolean model of ABA-induced stomatal closure in Arabidopsis thaliana took over two years of manual effort across multiple publications [7].
Q2: What is automated model refinement and how does it address this challenge?
Automated model refinement uses computational workflows, such as genetic algorithms, to systematically adjust a model's parameters to better agree with experimental data. Tools like boolmore can streamline this process, achieving accuracy gains that surpass years of manual revision by automatically exploring a space of biologically plausible models [7].
Q3: My model gets stuck in a local optimum during refinement. What can I do? Advanced optimization pipelines like DANTE address this by incorporating mechanisms such as local backpropagation. This technique updates visitation data in a way that creates a gradient to help the algorithm escape local optima, preventing it from repeatedly visiting the same suboptimal solutions [15].
Q4: How can I ensure my refined model generalizes well and doesn't overfit the training data?
Benchmarking is crucial. Studies with boolmore showed that refined models improved their accuracy on a validation set from 47% to 95% on average, demonstrating that proper algorithmic refinement enhances predictive power without overfitting [7]. Using a hold-out validation set is a standard practice to test generalizability.
Q5: What kind of data is needed for automated refinement with a tool like boolmore?
The primary input is a compilation of curated perturbation-observation pairs. These are individual experimental results that describe the state of a biological node under specific conditions, such as a knockout or stimulus. This is common data in traditional functional biology, making the method suitable even without high-throughput datasets [7].
Quantitative Data on Refinement Performance
The table below summarizes key performance metrics from the boolmore case study, demonstrating its effectiveness against manual methods [7].
| Metric | Starting Model (Manual) | Refined Model (boolmore) | Notes |
|---|---|---|---|
| Training Set Accuracy (Average) | 49% | 99% | Accuracy on the set of experimental data used for refinement. |
| Validation Set Accuracy (Average) | 47% | 95% | Accuracy on a held-out set of experiments, demonstrating improved generalizability. |
| Time to Achieve Refinement | ~2 years (manual revisions) | Automated workflow | The manual process spanned publications from 2006 to 2018-2020. |
| Key Improvement in ABA Stomatal Closure | Baseline | Surpassed manual accuracy gain | The refined model agreed significantly better with a compendium of published results. |
Experimental Protocol: TheboolmoreWorkflow
The following is a detailed methodology for refining a Boolean model using the boolmore genetic algorithm-based workflow [7].
Input Preparation:
- Starting Model: Provide the initial Boolean model, including its interaction graph and regulatory functions.
- Biological Constraints: Define known biological mechanisms as logical relations (e.g., "A is necessary for B").
- Experimental Compendium: Curate a set of perturbation-observation pairs, categorizing observations (e.g., OFF, ON, "Some").
Model Mutation:
- The algorithm generates new candidate models ("offspring") by mutating the regulatory functions of the starting model.
- Mutations are constrained to preserve the original interaction graph's structure and signs, and to respect the user-provided biological constraints. Regulations can be deleted and later recovered.
Prediction Generation:
- For each candidate model, calculate its long-term behaviors (minimal trap spaces) under each experimental setting defined in the perturbation-observation pairs.
- Determine the predicted state (ON, OFF, or oscillating) for each node.
Fitness Scoring:
- Compute a fitness score for each model by quantifying its agreement with the experimental compendium.
- Scoring is hierarchical; to score well on a double perturbation experiment, the model must also agree with the constituent single perturbations.
Selection and Iteration:
- Retain the models with the top fitness scores, with a preference for models with fewer added edges.
- Repeat the steps of mutation, prediction, and selection for multiple generations to evolve an optimized model.
Workflow and Signaling Pathway Diagrams
Automated Model Refinement Workflow
Simplified ABA Stomatal Closure Signaling Pathway
Research Reagent Solutions
The table below lists key computational and biological tools used in automated model refinement, as featured in the case study and related research [7] [15].
| Item Name | Type | Function in Refinement |
|---|---|---|
boolmore Tool |
Software Workflow | A genetic algorithm-based tool that refines Boolean models to better fit perturbation-observation data [7]. |
| Perturbation-Observation Pairs | Curated Data | A compiled set of experiments that serve as the ground truth for scoring and training model candidates [7]. |
| Deep Active Optimization (DANTE) | Optimization Pipeline | An AI pipeline that uses a deep neural surrogate and tree search to find optimal solutions in high-dimensional problems with limited data [15]. |
| Minimal Trap Space Calculator | Computational Method | Used to determine the long-term behavior (e.g., ON/OFF states) of a Boolean model under specific conditions for prediction [7]. |
Frequently Asked Questions (FAQs) on Dose Optimization
1. What is Project Optimus and why was it initiated? Project Optimus is an initiative launched by the U.S. Food and Drug Administration's (FDA) Oncology Center of Excellence in 2021. Its mission is to reform the dose-finding and dose selection paradigm in oncology drug development. It was initiated due to a growing recognition that conventional methods for determining the best dose of a new agent are inadequate. These older methods often identify unnecessarily high doses for modern targeted therapies and immunotherapies, leading to increased toxicity without added benefit for patients [16] [17].
2. What are the main limitations of conventional dose-finding methods like the 3+3 design? Conventional methods, such as the 3+3 design, have several critical flaws:
- Ignores Efficacy: They select a dose based primarily on short-term toxicity (Maximum Tolerated Dose, or MTD) and ignore whether the drug is actually effective at treating cancer [16] [17].
- Poorly Suited for Modern Therapies: They were designed for cytotoxic chemotherapies and rely on the assumption that both toxicity and efficacy always increase with dose. This is often not true for targeted therapies, where efficacy may plateau while toxicity continues to rise [16].
- Short-Term Focus: They evaluate toxicity over very short periods (e.g., one to two cycles), which does not reflect the reality of patients staying on modern therapies for months or years, leading to issues with cumulative or late-onset toxicities [16].
- High Failure Rate: Studies show that nearly 50% of patients on late-stage trials for targeted therapies require dose reductions, and the FDA has required additional studies to re-evaluate the dosing for over 50% of recently approved cancer drugs [17].
3. What are model-informed approaches in dose optimization? Model-informed approaches use mathematical and statistical models to integrate and analyze all available data to support dose selection. Key approaches include [18]:
- Exposure-Response Modeling: Determines the relationship between drug exposure in the body and its safety and efficacy outcomes.
- Population Pharmacokinetic (PK) Modeling: Describes how drug concentrations vary in different patients and can be used to select dosing regimens that achieve target exposure levels.
- Quantitative Systems Pharmacology (QSP): Incorporates biological mechanisms to understand and predict a drug's effects with limited clinical data. These models can predict outcomes for doses not directly tested and help identify an optimized dose with a better benefit-risk profile [18].
4. What are adaptive or seamless trial designs? Traditional drug development has separate trials for distinct stages (Phase 1, 2, and 3). Adaptive or seamless designs combine these various phases into a single trial [17] [19]. For example, an adaptive Phase 2/3 design might test multiple doses in Stage 1, then select the most promising dose to continue into Stage 2 for confirmatory testing. This allows for more rapid enrollment, faster decision-making, and the accumulation of more long-term safety and efficacy data to better inform dosing decisions [17].
Troubleshooting Guide: Common Scenarios in Dose Optimization
Scenario 1: High Rates of Dose Modification in Late-Stage Trials
Problem: A high percentage of patients in a registrational trial require dose reductions, interruptions, or discontinuations due to intolerable side effects [17].
| Investigation Step | Action | Goal |
|---|---|---|
| Analyze Data | Review incidence of dosage modifications, long-term toxicity data, and patient-reported outcomes from early trials [18]. | Identify the specific toxicities causing modifications and their relationship to drug exposure. |
| Model Exposure-Response | Perform exposure-response (ER) modeling to link drug exposure (e.g., trough concentration) to the probability of key adverse events [18]. | Quantify the benefit-risk trade-off for different dosing regimens. |
| Evaluate Lower Doses | Use the ER model to simulate the potential safety profile of lower doses or alternative schedules (e.g., reduced frequency). | Determine if a lower dose maintains efficacy while significantly improving tolerability. |
| Consider Randomized Evaluation | If feasible, initiate a randomized trial comparing the original high dose with the optimized lower dose to confirm the improved benefit-risk profile [16]. | Generate high-quality evidence for dose selection as encouraged by Project Optimus [16]. |
Scenario 2: Efficacy Plateau with Increasing Dose
Problem: Early clinical data suggests that the anti-cancer response (e.g., tumor shrinkage) reaches a maximum at a certain dose level, but toxicity continues to increase at higher doses [16].
| Investigation Step | Action | Goal |
|---|---|---|
| Identify Efficacy Plateau | Analyze dose-response data for efficacy endpoints (e.g., Overall Response Rate) and safety endpoints (e.g., Grade 3+ adverse events) [18]. | Visually confirm the plateau effect and identify the dose where it begins. |
| Integrate Pharmacodynamic Data | Incorporate data on target engagement or pharmacodynamic biomarkers. For example, assess if the dose at which target saturation occurs aligns with the efficacy plateau [17]. | Understand the biological basis for the plateau and identify a biologically optimal dose. |
| Apply Clinical Utility Index (CUI) | Use a CUI framework to quantitatively combine efficacy and safety data into a single score for each dose level [17]. | Objectively compare doses and select the one that offers the best overall value. |
| Select Optimized Dose | Choose the dose that provides near-maximal efficacy with a significantly improved safety profile compared to the MTD. | Avoid the "false economy" of selecting an overly toxic dose that provides no additional patient benefit [16]. |
Experimental Protocols for Key Dose Optimization Analyses
Protocol 1: Exposure-Response Analysis for Safety
Objective: To characterize the relationship between drug exposure and the probability of a dose-limiting toxicity to inform dose selection.
Materials:
- Research Reagent Solutions:
- Patient PK/PD Data: Collected plasma concentration-time data from your First-in-Human trial.
- Safety Data: Graded adverse event data, standardized using CTCAE criteria.
- Population PK Model: A model describing the typical population pharmacokinetics of your drug and sources of variability.
- Software: Non-linear mixed-effects modeling software (e.g., NONMEM, Monolix, R).
Methodology:
- Data Preparation: Merge individual patient exposure metrics (e.g., predicted trough concentration or area under the curve from the population PK model) with the corresponding safety event data (e.g., occurrence of a severe adverse event over a defined period) [18].
- Model Development: Use logistic regression or time-to-event modeling to relate the exposure metric to the probability (or hazard) of the safety event.
- Model structure:
Logit(P(Event)) = β0 + β1 * Exposure - Where P(Event) is the probability of the adverse event, and β1 represents the steepness of the exposure-response relationship [18].
- Model structure:
- Model Validation: Evaluate the model's goodness-of-fit using diagnostic plots and visual predictive checks to ensure it adequately describes the observed data.
- Simulation: Use the validated model to simulate the probability of the adverse event across a range of potential doses and dosing regimens [18].
- Decision-Making: Compare the simulated safety profiles to identify doses with an acceptable risk level.
Protocol 2: Clinical Utility Index (CUI) for Dose Selection
Objective: To integrate multiple efficacy and safety endpoints into a single quantitative value to rank and compare different dose levels.
Materials:
- Research Reagent Solutions:
- Efficacy & Safety Data: Key efficacy (e.g., ORR, PFS) and safety (e.g., rate of specific AEs, dose intensity) metrics for each dose level.
- Stakeholder Input: Pre-defined weights reflecting the relative importance of each endpoint (e.g., from clinicians, patients, regulators).
- Computational Tool: Spreadsheet software or statistical software (e.g., R, Python).
Methodology:
- Define Endpoints and Weights: Select the critical efficacy and safety endpoints to include in the index. Assign a weight to each endpoint based on stakeholder input, ensuring the sum of all weights is 1 [17].
- Normalize Endpoint Values: Rescale the raw data for each endpoint to a common scale (e.g., 0 to 1, where 1 is most desirable). For efficacy, higher values are better; for safety (toxicity), lower values are better, so normalization may need to be inverted.
- Calculate CUI: For each dose level, calculate the CUI using a linear additive model:
CUI_Dose = [Weight_E1 * Normalized_E1] + [Weight_E2 * Normalized_E2] + ... + [Weight_S1 * (1 - Normalized_S1)] + ...- Where E represents efficacy endpoints and S represents safety endpoints [17].
- Rank and Select: Rank the dose levels based on their CUI scores. The dose with the highest CUI represents the best balance of efficacy and safety according to the pre-defined criteria.
Research Reagent Solutions for Dose Optimization
| Item | Function in Dose Optimization |
|---|---|
| Population PK Modeling | Describes the typical drug concentration-time profile in a population and identifies sources of variability (e.g., due to organ function, drug interactions) to support fixed vs. weight-based dosing and dose adjustments [18]. |
| Exposure-Response Modeling | Correlates drug exposure metrics with changes in clinical endpoints (safety or efficacy) to predict the outcomes of untested dosing regimens and understand the therapeutic index [18]. |
| Clinical Utility Index (CUI) | Provides a quantitative and collaborative framework to integrate multiple data types (efficacy, safety, PK) to determine the dose with the best overall benefit-risk profile [17]. |
| Backfill/Expansion Cohorts | Enrolls additional patients at specific dose levels of interest within an early-stage trial to strengthen the understanding of that dose's benefit-risk ratio [17]. |
| Adaptive Seamless Trial Design | Combines traditionally distinct trial phases (e.g., Phase 2 and 3) into one continuous study, allowing for dose selection based on early data and more efficient confirmation of the chosen dose [17] [19]. |
Workflow Diagrams for Dose Optimization Strategies
Diagram 1: Model-Informed Dose Optimization Workflow
Diagram 2: Troubleshooting High Toxicity with Exposure-Response
In the landscape of modern drug development, 'Fit-for-Purpose' (FFP) models represent a paradigm shift in how computational and quantitative approaches are integrated into regulatory decision-making. The U.S. Food and Drug Administration (FDA) defines the FFP initiative as a pathway for regulatory acceptance of dynamic tools for use in drug development programs [20]. These models are not one-size-fits-all solutions; rather, they are specifically developed and tailored to answer precise questions of interest (QOI) within a defined context of use (COU) at specific stages of the drug development lifecycle [21].
The imperative for FFP models stems from the need to improve drug development efficiency and success rates. Evidence demonstrates that a well-implemented FFP approach can significantly shorten development cycle timelines, reduce discovery and trial costs, and provide better quantitative risk estimates amidst development uncertainties [21]. As drug modalities become more complex and therapeutic targets more challenging, the strategic application of FFP models provides a structured, data-driven framework for evaluating safety and efficacy throughout the entire drug development process, from early discovery to post-market surveillance.
The Scientific Framework for FFP Model Development
Core Principles and Regulatory Alignment
FFP model development operates under several core principles that ensure regulatory alignment and scientific rigor. A model is considered FFP when it successfully defines the COU, ensures data quality, and undergoes proper verification, calibration, validation, and interpretation [21]. Conversely, a model fails to be FFP when it lacks a clearly defined COU, utilizes poor quality data, or suffers from unjustified oversimplification or unnecessary complexity.
The International Council for Harmonisation (ICH) has expanded its guidance to include MIDD, specifically the M15 general guidance, promoting global harmonization in model application [21]. This standardization improves consistency among global sponsors applying FFP models in drug development and regulatory interactions, potentially streamlining processes worldwide. Regulatory agencies emphasize that FFP tools must be "reusable" or "dynamic" in nature, capable of adapting to multiple disease areas or development scenarios, as demonstrated by successful applications in dose-finding and patient drop-out modeling across various therapeutic areas [21].
Structured Troubleshooting for Model Optimization
When FFP models underperform, particularly with low-accuracy targets, researchers require systematic troubleshooting methodologies. Adapted from proven laboratory troubleshooting frameworks [22], the following workflow provides a structured approach to diagnosing and resolving model deficiencies:
Figure 1. Systematic troubleshooting workflow for optimizing low-accuracy FFP models.
This troubleshooting methodology emphasizes iterative refinement and validation, ensuring that model optimizations directly address root causes of inaccuracy while maintaining regulatory compliance.
Technical Support Center: FFP Model Troubleshooting Guides
Frequently Asked Questions (FAQs) on FFP Model Refinement
Q: What are the primary causes of low accuracy in target localization and quantification for FFP models, and how can they be diagnosed?
Low accuracy in target localization often stems from multiple factors, including uncertainties in model structure, inaccurate parameter estimations, and challenges in model construction that account for both mobility and localization constraints [23] [24]. Diagnosis should begin with residual error analysis to identify systematic biases, followed by parameter identifiability assessment using profile likelihood or Markov chain Monte Carlo (MCMC) sampling. For long-distance target localization issues specifically, researchers have implemented pruning operations and silhouette coefficient calculations based on multiple target relative coordinates to efficiently identify clusters near true relative coordinates [24].
Q: How can we improve coordinate fusion accuracy in multi-target FFP models?
Advanced clustering algorithms can significantly enhance coordinate fusion accuracy. Research demonstrates that improved hierarchical density-based spatial clustering of applications with noise (HDBSCAN) algorithms effectively fuse relative coordinates of multiple targets [23] [24]. The implementation involves introducing a pruning operation and silhouette coefficient calculation based on multiple target relative coordinates, which efficiently identifies clusters near the true relative coordinates of targets, thereby improving coordinate fusion effectiveness [24]. This approach has maintained relative localization error within 4% and absolute localization error within 6% for static targets at distances ranging from 100 to 500 meters in robotics applications, with similar principles applying to pharmacological target localization [24].
Q: What optimization algorithms show the most promise for refining path planning in adaptive FFP models?
Double deep Q-networks (DDQN) with reward strategies based on coordinate fusion error have demonstrated significant improvements in positioning accuracy for long-distance targets [23] [24]. Successful implementation involves developing an experience replay buffer that includes state information such as grid centers and estimated target coordinates, constructing behavior and target networks, and designing appropriate loss functions [24]. For drug development applications, this translates to creating virtual population simulations that adaptively explore parameter spaces, with reward functions aligned with precision metrics rather than mere convergence.
Q: How does the FDA's FFP initiative impact model selection and validation requirements?
The FDA's FFP initiative provides a pathway for regulatory acceptance of dynamic tools that may not have formal qualification [20]. A drug development tool (DDT) is deemed FFP based on the acceptance of the proposed tool following thorough evaluation of submitted information. This evaluation publicly determines the FFP designation to facilitate greater utilization of these tools in drug development programs [20]. The practical implication is that researchers must clearly document the COU, QOI, and model validation strategies that demonstrate fitness for their specific purpose, as exemplified by approved FFP tools in Alzheimer's disease and dose-finding applications [20].
Q: What are the consequences of using non-FFP models in regulatory submissions?
Non-FFP models risk regulatory rejection due to undefined COU, poor data quality, inadequate model verification, or unjustified incorporation of complexities [21]. Specifically, oversimplification that eliminates critical biological processes, or conversely, unnecessary complexity that cannot be supported by available data, renders models unsuitable for regulatory decision-making. Additionally, machine learning models trained on specific clinical scenarios may not be FFP for predicting different clinical settings, leading to extrapolation errors and regulatory concerns [21].
Advanced Optimization Methodologies for Low-Accuracy Targets
Enhanced Sensing and Positioning Algorithms
Robotics research provides transferable methodologies for improving target localization accuracy in pharmacological models. One advanced approach involves dividing the movement area into hexagonal grids and introducing constraints on stopping position selection and non-redundant locations [24]. Based on image parallelism principles, researchers have developed methods for calculating the relative position of targets using sensing information from two positions, significantly improving long-distance localization precision [23]. These techniques can be adapted to improve the accuracy of physiological compartment identification in PBPK models and target engagement quantification in QSP models.
Integrated Residual Attention Units for Feature Extraction
For complex remote sensing image change detection, researchers have developed Integrated Residual Attention Units (IRAU) that optimize detection accuracy through ResNet variants, Split and Concat (SPC) modules, and channel attention mechanisms [25]. These units extract semantic information from feature maps at various scales, enriching and refining the feature information to be detected. In one application, this approach improved accuracy from 0.54 to 0.97 after training convergence, with repeated detection accuracy ranging from 95.82% to 99.68% [25]. Similar architectures can enhance feature detection in pharmacological models dealing with noisy or complex biological data.
Depth-wise Separable Convolution for Real-time Processing
Depth-wise Separable Convolution (DSC) modules significantly optimize processing efficiency while maintaining accuracy [25]. When combined with attention mechanisms, these modules reduce computational complexity and latency, crucial for real-time applications and large-scale simulations. In benchmark tests, removing DSC modules increased latency by 117ms while decreasing accuracy by 1.91% [25]. For large virtual population simulations in drug development, implementing similar efficient processing architectures can enable more extensive sampling and faster iteration cycles.
Quantitative Performance Data for FFP Model Optimization
Table 1. Comparative performance metrics of optimization algorithms for target localization
| Algorithm | Relative Localization Error | Absolute Localization Error | Optimal Path Identification | Application Context |
|---|---|---|---|---|
| LTLO [24] | <4% | <6% | Yes | Long-distance static targets (100-500m) |
| Traditional Monocular Visual Localization (TMVL) [24] | >4% | >6% | Limited | Short-distance dynamic targets |
| Monocular Global Geolocation (MGG) [24] | Higher than LTLO | Higher than LTLO | Partial | Intermediate distance with GPS |
| Long-range Binocular Vision Target Geolocation (LRBVTG) [24] | Higher than LTLO | Higher than LTLO | No | Specific distance ranges |
Table 2. Accuracy optimization results with advanced architectural components
| Model Component | Performance Improvement | Training Impact | Latency Effect | Implementation Complexity |
|---|---|---|---|---|
| Integrated Residual Attention Unit (IRAU) [25] | Accuracy increased from 0.54 to 0.97 | Faster convergence | Moderate increase | High (requires specialized architecture) |
| Depth-wise Separable Convolution (DSC) [25] | 1.91% accuracy improvement | Standard convergence | 117ms reduction | Medium (modification of existing layers) |
| Improved HDBSCAN Algorithm [24] | Relative error <4%, Absolute error <6% | Requires coordinate fusion training | Minimal increase | Medium (clustering implementation) |
| Double Deep Q-Network (DDQN) [24] | Optimal path identification | Requires extensive training | Initial high computational load | High (reinforcement learning setup) |
Experimental Protocols for Key Methodologies
Protocol 1: Implementing Improved HDBSCAN for Coordinate Fusion
Purpose: To enhance coordinate fusion accuracy in multi-target FFP models using an improved HDBSCAN algorithm.
Materials and Reagents:
- Multi-dimensional parameter estimation data
- Computational environment (Python/R/MATLAB)
- HDBSCAN library with custom modifications
- Validation dataset with known ground truth
Procedure:
- Data Preparation: Compile relative coordinates from multiple target estimations into a feature matrix.
- Pruning Operation: Implement silhouette coefficient-based pruning to eliminate outlier coordinates that fall outside acceptable confidence intervals.
- Cluster Identification: Apply modified HDBSCAN algorithm with constraints tailored to the specific target topology.
- Coordinate Fusion: Calculate weighted centroids of identified clusters, giving higher weights to coordinates with lower estimated variance.
- Validation: Compare fused coordinates against ground truth using standardized error metrics.
Validation Metrics: Relative localization error (<4% target), absolute localization error (<6% target), and cluster stability across multiple iterations [24].
Protocol 2: DDQN with Experience Replay for Path Optimization
Purpose: To implement a reinforcement learning approach for optimizing model exploration strategies in parameter space.
Materials and Reagents:
- State definition of model parameters and targets
- Reward function framework
- DDQN implementation framework (e.g., TensorFlow, PyTorch)
- Experience replay buffer infrastructure
Procedure:
- State Representation: Define state information including current parameter estimates, target coordinates, and uncertainty metrics.
- Reward Function Design: Create a reward strategy based on coordinate fusion error reduction rather than absolute accuracy.
- Network Architecture: Construct separate behavior and target networks with identical architecture but different update frequencies.
- Experience Replay: Implement prioritized experience replay that stores state transitions and associated rewards.
- Training Cycle: Iterate through action selection, reward calculation, experience storage, and model updates until convergence.
Validation Metrics: Path efficiency improvement, reduction in target localization error, and training stability [24].
Research Reagent Solutions for FFP Model Development
Table 3. Essential computational tools for FFP model optimization
| Tool Category | Specific Examples | Function in FFP Development | Regulatory Considerations |
|---|---|---|---|
| Physiologically Based Pharmacokinetic (PBPK) Platforms [21] | GastroPlus, Simcyp Simulator | Mechanistic modeling of drug disposition incorporating physiology and product quality | FDA FFP designation available for specific COUs |
| Quantitative Systems Pharmacology (QSP) Frameworks [21] | DILIsym, ITCsym | Integrative modeling combining systems biology with pharmacology for mechanism-based predictions | Requires comprehensive validation and biological plausibility documentation |
| Population PK/PD Tools [21] | NONMEM, Monolix, R/nlme | Explain variability in drug exposure and response among individuals in a population | Well-established regulatory precedent with standardized submission requirements |
| AI/ML Platforms [21] | TensorFlow, PyTorch, Scikit-learn | Analyze large-scale biological and clinical datasets for pattern recognition and prediction | Emerging regulatory framework with emphasis on reproducibility and validation |
| First-in-Human (FIH) Dose Algorithm Tools [21] | Allometric scaling, QSP-guided prediction | Determine starting dose and escalation scheme based on preclinical data | High regulatory scrutiny requiring robust safety margins and justification |
The strategic development and refinement of 'Fit-for-Purpose' models represents a critical advancement in model-informed drug development. By applying systematic troubleshooting methodologies, leveraging advanced optimization algorithms from complementary fields, and maintaining alignment with regulatory expectations through the FDA's FFP initiative, researchers can significantly enhance model accuracy and reliability for challenging targets. The integration of approaches such as improved HDBSCAN clustering, DDQN path optimization, and architectural improvements like IRAU and DSC modules provides a robust toolkit for addressing the persistent challenge of low-accuracy targets in pharmacological modeling. As the field evolves, continued emphasis on methodological rigor, comprehensive validation, and regulatory communication will ensure that FFP models fulfill their potential to accelerate therapeutic development and improve patient outcomes.
From Data to Discovery: Modern Methodologies for Effective Model Refinement
What is boolmore and what is its primary function? boolmore is an open-source, genetic algorithm (GA)-based workflow designed to automate the refinement of Boolean models of biological networks. Its primary function is to adjust the Boolean functions of an existing model to improve its agreement with a corpus of curated experimental data, formatted as perturbation-observation pairs. This process, which traditionally requires manual trial-and-error, is streamlined by boolmore, which efficiently searches the space of biologically plausible models to find versions with higher accuracy [7] [26].
What are the core biological concepts behind the models boolmore refines? boolmore works on Boolean models, which are a type of discrete dynamic model used to represent biological systems like signal transduction networks. In these models [7]:
- Nodes represent biological components (e.g., proteins).
- Edges represent causal interactions between them (e.g., activation or inhibition).
- Node States are either 0 (OFF/inactive) or 1 (ON/active).
- Regulatory Functions are Boolean rules (using AND, OR, NOT) that determine a node's state based on its regulators.
- Long-term behavior is analyzed through minimal trap spaces (or quasi-attractors), which represent the stable patterns of activity the system can settle into.
Essential Research Reagents and Tools
The following table details the key "research reagents" – the core inputs, software, and knowledge required – to run a boolmore experiment successfully.
Table 1: Research Reagent Solutions for boolmore Experiments
| Item Name | Type | Function / Purpose |
|---|---|---|
| Starting Boolean Model | Input Model | The initial network (interaction graph and Boolean rules) to be refined. Serves as the baseline and constrains the search space [7]. |
| Perturbation-Observation Pairs | Input Data | A curated compendium of experimental results. Each pair describes the observed state of a node under a specific perturbation context (e.g., a knockout) [7]. |
| Biological Mechanism Constraints | Input Knowledge | Logical relations (e.g., "A is necessary for B") provided by the researcher to ensure evolved models remain biologically plausible [7]. |
| CoLoMoTo Software Suite | Software Environment | An integrated Docker container or Conda environment that provides access to over 20 complementary tools for Boolean model analysis, ensuring reproducibility [27]. |
| GINsim | Software Tool | Used within the CoLoMoTo suite to visualize and edit the network structure and logical rules of the Boolean model [27]. |
| bioLQM & BNS | Software Tools | Tools within the CoLoMoTo suite used for attractor analysis, which is crucial for generating model predictions to compare against experimental data [27]. |
boolmore Workflow and Experimental Protocol
The boolmore refinement process follows a structured, iterative workflow. The diagram below illustrates the key stages from initial setup to final model analysis.
Detailed Step-by-Step Experimental Protocol
Input Preparation
- Obtain your Starting Boolean Model in a supported format (e.g., SBML-qual). The model's interaction graph should be biologically reasonable, though it may be missing some edges [7].
- Curate your Perturbation-Observation Pairs from experimental literature. Categorize observations (e.g., OFF, ON, "Some" activity) and organize perturbations hierarchically (e.g., single then double knockouts) for accurate scoring [7].
- Define Biological Constraints as logical statements to limit the algorithm's search to functionally plausible models [7].
Algorithm Execution and Configuration
- Initialize the genetic algorithm. boolmore will create the first generation of models by applying mutation and crossover operators to the starting model's Boolean functions, while respecting your constraints and the interaction graph [7].
- For each new model (offspring), boolmore performs fitness scoring. It calculates the model's minimal trap spaces under each perturbation setting and compares the predictions to your experimental pairs. The score reflects the degree of agreement [7].
- The models with the top fitness scores are selected to produce the next generation. This cycle repeats for a predefined number of generations or until convergence [7].
Output and Validation
- The primary output is one or more Refined Boolean Models with higher accuracy against the training data.
- Crucially, these models should be validated against a hold-out validation set of experimental data not used during refinement to ensure the model has not overfitted and possesses predictive power [7].
- Analyze the refined model's structure and dynamics to generate new, testable predictions for experimental validation [7].
Performance Benchmarking and Data
In-silico benchmarks on a suite of 40 biological models demonstrated boolmore's effectiveness. The table below summarizes the quantitative performance gains.
Table 2: boolmore Benchmark Performance on 40 Biological Models
| Model Set | Starting Model Average Accuracy | Refined Model Average Accuracy | Performance Gain |
|---|---|---|---|
| Training Set (80% of data) | 49% | 99% | +50 percentage points |
| Validation Set (20% of data) | 47% | 95% | +48 percentage points |
This data shows that boolmore can dramatically improve model accuracy without overfitting, as evidenced by the high performance on the unseen validation data [7].
Integration with Analysis Workflows
boolmore operates within a broader ecosystem of model analysis tools. The diagram below shows how it fits into a reproducible workflow using the CoLoMoTo software suite.
Frequently Asked Questions (FAQs)
My refined model has high accuracy on the training data but performs poorly on new perturbations. What went wrong? This is a classic sign of overfitting. Your model may have become overly specialized to the specific experiments in your training set.
- Solution: Ensure you are using a hold-out validation set (data not used for refinement) to monitor performance during the process. Increase the stringency of your biological constraints to limit the algorithm's search to a more plausible model space. You may also need to adjust GA parameters like population size or mutation rate to encourage broader exploration [7].
The algorithm isn't converging on a high-fitness model. How can I improve the search?
- Solution: First, verify the quality and consistency of your perturbation-observation pairs. Inconsistent data can confuse the fitness function. Second, review your biological constraints; they might be too restrictive. Consider allowing the algorithm to add interactions from a user-provided pool of potential edges if the starting network is incomplete. Finally, you can tune GA parameters like mutation probability or the number of models per generation [7].
How do I handle experimental observations that are not simply ON or OFF?
- Solution: boolmore supports an intermediate category, labeled "Some", to represent observations of an intermediate level of activation. You can incorporate these into your data compilation. The scoring function can be configured to handle this category appropriately, giving partial credit for predictions that match this intermediate state [7].
Can I use boolmore for lead optimization in drug discovery?
- Answer: While boolmore itself refines network models, the genetic algorithm approach is directly applicable to drug design. Tools like AutoGrow4 use a very similar GA workflow for de novo drug design and lead optimization. They start with seed molecules and use crossover and mutation operators to evolve new compounds with better predicted binding affinity to a protein target [28]. The core concepts of using a GA to optimize a complex model against a fitness score are directly transferable.
Technical Support Center: FAQs & Troubleshooting Guides
Frequently Asked Questions (FAQs)
FAQ 1: Why is my decision tree model for genomic variant analysis encountering memory errors?
The most likely cause is that the analysis includes genes with an unusually high number of variants or particularly long genes, which demand significant memory during aggregation steps. Examples of such problematic genes include RYR2 (ENSG00000198626) and SCN5A (ENSG00000183873) [29].
To resolve this, increase the memory allocation in your workflow configuration files. The following table summarizes the recommended changes for the quick_merge.wdl file [29]:
Table: Recommended Memory Adjustments in quick_merge.wdl
| Task | Parameter | Default | Change to |
|---|---|---|---|
split |
memory |
1 GB | 2 GB |
first_round_merge |
memory |
20 GB | 32 GB |
second_round_merge |
memory |
10 GB | 48 GB |
Similarly, adjustments are needed in the annotation.wdl file [29]:
Table: Recommended Memory Adjustments in annotation.wdl
| Task | Parameter | Default | Change to |
|---|---|---|---|
fill_tags_query |
memory allocation |
2 GB | 5 GB |
annotate |
memory allocation |
1 GB | 5 GB |
sum_and_annotate |
memory allocation |
5 GB | 10 GB |
FAQ 2: What could cause a high number of haploid calls (ACHemivariant > 0) for a gene located on an autosome?
For autosomal variants, the majority of samples will have diploid genotypes (e.g., 0/1). However, some samples may exhibit haploid (hemizygous-like) calls (e.g., 1) for specific variants [29].
This typically indicates that the variant call is located within a known deletion on the homologous chromosome for that sample. These haploid calls are not produced during aggregation but are already present in the input single-sample gVCFs [29].
Worked Example: In a single-sample gVCF, you might observe a haploid ALT call for a variant (e.g., chr1:2118756 A>T with genotype '1'). This occurs because a heterozygous deletion (e.g., chr1:2118754 TGA>T with genotype '0/1') is located upstream, spanning the position of the A>T SNP. The SNP is therefore called as haploid because it resides within the deletion on one chromosome [29].
FAQ 3: Why do my variant classifications conflict with public databases like ClinVar, and how can I resolve this?
Conflicting interpretations of pathogenicity (COIs) are a common challenge. A 2024 study found that 5.7% of variants in ClinVar have conflicting interpretations, and 78% of clinically relevant genes harbor such variants [30]. Discrepancies often arise from several factors [31]:
- Differences in classification methods: Use of different guidelines (e.g., ACMG/AMP vs. Sherloc) or gene-specific modifications.
- Differences in application of methods: Subjectivity in applying evidence categories (e.g., PS3/BS3 for functional data or BS1 for population frequency).
- Differences in evidence: Inconsistent access to the latest medical literature or internal clinical data.
- Differences in interpreter opinions: Subjective judgment, especially for variants associated with rare diseases.
Resolution Strategy: Collaboration and evidence-sharing between clinical laboratories and researchers can resolve a significant portion of these discrepancies. Ensuring all parties use the same classification guidelines, data sources, and versions is a critical first step [31].
FAQ 4: What are the key performance metrics for optimized decision tree models in pattern recognition, and how do they compare to other models?
Optimized decision tree models, such as those combining Random Forest and Gradient Boosting, can achieve high accuracy. The following table compares the performance of an optimized decision tree with other common algorithms from a 2025 study on pattern recognition [32]:
Table: Algorithm Performance Comparison for Pattern Recognition
| Algorithm | Accuracy (%) | Model Size (MB) | Memory Usage (MB) |
|---|---|---|---|
| Optimized Decision Tree | 94.9 | 50 | 300 |
| Support Vector Machine (SVM) | 87.0 | 45 | Not Specified |
| Convolutional Neural Network (CNN) | 92.0 | 200 | 800 |
| XGBoost | 94.6 | Not Specified | Not Specified |
| LightGBM | 94.7 | 48 | Not Specified |
| CatBoost | 94.5 | Not Specified | Not Specified |
Troubleshooting Guide: Data Quality and Model Performance
Problem: The model's predictions are inaccurate or nonsensical, potentially due to underlying data issues.
This is a classic "Garbage In, Garbage Out" (GIGO) scenario. In bioinformatics, the quality of input data directly dictates the quality of the analytical results. Up to 30% of published research may contain errors traceable to data quality issues at the collection or processing stage [33].
Solution: Implement a multi-layered data quality control strategy.
Table: Common Data Pitfalls and Prevention Strategies
| Pitfall | Description | Prevention Strategy |
|---|---|---|
| Sample Mislabeling | Incorrect tracking of samples during collection, processing, or analysis. | Implement rigorous sample tracking systems (e.g., barcode labeling) and regular identity verification using genetic markers [33]. |
| Technical Artifacts | Non-biological signals from sequencing (e.g., PCR duplicates, adapter contamination). | Use tools like Picard and Trimmomatic to identify and remove artifacts before analysis [33]. |
| Batch Effects | Systematic differences between sample groups processed at different times or locations. | Employ careful experimental design and statistical methods for batch effect correction [33]. |
| Contamination | Presence of foreign genetic material (e.g., cross-sample, bacterial). | Process negative controls alongside experimental samples to identify contamination sources [33]. |
Detailed Methodology for Data Validation:
- Standardized Protocols (SOPs): Develop and adhere to detailed, validated SOPs for every data handling step, from tissue sampling to sequencing, following standards from organizations like the Global Alliance for Genomics and Health (GA4GH) [33].
- Quality Control Metrics: Establish thresholds for key metrics. For next-generation sequencing, use tools like FastQC to monitor base call quality scores (Phred scores), read length distributions, and GC content [33].
- Data Validation: Ensure data makes biological sense by checking for expected patterns (e.g., gene expression profiles matching known tissue types). Employ cross-validation using alternative methods (e.g., confirming a variant from WGS with targeted PCR) [33].
- Version Control and Reproducibility: Use systems like Git to track changes to datasets and analysis workflows. Utilize workflow managers like Nextflow or Snakemake to ensure all processing steps are documented and reproducible [33].
Experimental Protocol: Building an Optimized Decision Tree Model for Variant Analysis
This protocol details the methodology for creating a high-accuracy decision tree model, adapted from a 2025 study on pattern recognition [32].
1. Data Collection and Preprocessing
- Data Source: Collect genomic data from high-precision sources. This may include key parameters such as allele counts, read depth, and functional prediction scores.
- Data Preprocessing: Perform data cleaning steps, including denoising and standardization, to ensure data quality and consistency. Handle missing data and normalize features as necessary [32].
2. Model Training with Adaptive Hyperparameter Tuning
- Algorithm Selection: Combine the advantages of ensemble methods like Random Forest (RF) and Gradient Boosting Tree (GBT). RF enhances stability by integrating multiple trees, while GBT finely adjusts predictions through sequential optimization [32].
- Adaptive Feature Selection: The algorithm should adaptively select the most informative features (genomic annotations) to improve recognition of different variant classes and reduce overfitting [32].
- Hyperparameter Optimization: Use grid search to identify the optimal set of hyperparameters. Perform this within a cross-validation framework to ensure robust model selection and avoid overfitting [32].
3. Model Performance Evaluation
- Compare the optimized decision tree against commonly used benchmark algorithms such as Support Vector Machine (SVM) and Convolutional Neural Network (CNN) [32].
- Evaluate models based on key metrics: Accuracy, Precision, Recall, F1-Score, and Computational Efficiency (latency and memory usage) [34] [32].
Workflow Visualization: Decision Tree Model for Variant Analysis
The following diagram illustrates the logical workflow and data flow for a machine learning-enhanced genomic variant analysis pipeline.
Table: Key Resources for Genomic Variant Analysis with Machine Learning
| Item Name | Function / Purpose |
|---|---|
| ACMG/AMP Guidelines | The gold-standard framework for the clinical interpretation of sequence variants, providing criteria for classifying variants as Pathogenic, VUS, or Benign [30] [31]. |
| ClinVar Database | A public archive of reports detailing the relationships between human variations and phenotypes, with supporting evidence. Essential for benchmarking and identifying interpretation conflicts [30]. |
| Ensembl VEP (Variant Effect Predictor) | A tool that determines the effect of your variants (e.g., amino acid change, consequence type) on genes, transcripts, and protein sequence, as well as regulatory regions [30]. |
| gnomAD (Genome Aggregation Database) | A resource that aggregates and harmonizes exome and genome sequencing data from a wide variety of large-scale sequencing projects. Critical for assessing variant allele frequency [30]. |
| Scikit-learn (sklearn) | A core Python library for machine learning. It provides efficient tools for building and evaluating decision tree models, including Random Forest and Gradient Boosting classifiers [35]. |
| FastQC | A quality control tool for high throughput sequence data. It provides a modular set of analyses to quickly assess whether your raw genomic data is of high quality [33]. |
| Genome Analysis Toolkit (GATK) | A structured software library for variant discovery in high-throughput sequencing data. It provides best-practice workflows for variant calling and quality assessment [33]. |
| Python with Matplotlib | A fundamental plotting library for Python. Used for visualizing decision tree structures, feature importance, and other key model metrics to aid in interpretation [35]. |
Frequently Asked Questions (FAQs)
Q1: What are perturbation-observation pairs, and why are they fundamental for model refinement in biological systems?
Perturbation-observation pairs are a core data type in functional biology where a specific component of a biological system is perturbed (e.g., knocked out or stimulated), and the state of another component is observed [7]. In modeling, they are used to constrain and validate dynamic models. Unlike high-throughput data, these pairs are often piecewise and uneven, making them unsuitable for standard inference algorithms [7]. They are crucial for refining models because they provide direct, causal insights into the system's logic, allowing you to test and improve a model's predictive accuracy against known experimental outcomes.
Q2: My model fits the training perturbation data perfectly but fails to predict new experimental outcomes. What might be causing this overfitting?
Overfitting often occurs when a model becomes too complex and starts to memorize the training data rather than learning the underlying biological rules. To address this:
- Constrained Search Space: Limit the algorithm's search space to only biologically plausible models by incorporating existing mechanistic knowledge as logical constraints (e.g., "A is necessary for B") [7].
- Validation Set: Always hold back a portion of your experimental data (e.g., 20%) to use as a validation set. A refined model should show improved accuracy on both the training and this unseen validation set [7].
- Function Complexity: If using a tool like
boolmore, you can lock certain Boolean functions from mutating if they are already well-supported by evidence, preventing unnecessary complexity [7].
Q3: How can I refine a model when my data spans multiple time scales (e.g., fast signaling and slow gene expression)?
Integrating multi-scale data is challenging because a single model may not capture the full spectrum of dynamics. A proposed framework addresses this by:
- Data-Driven Decomposition: Using algorithms like Computational Singular Perturbation (CSP) to partition your dataset into subsets where the dynamics are similar and occur on a comparable time scale [36].
- Local Model Identification: Applying system identification methods, like Sparse Identification of Nonlinear Dynamics (SINDy), to each subset to identify the appropriate reduced model for that specific dynamical regime [36].
- Jacobian Estimation: Employing Neural Networks to estimate the Jacobian matrix from observational data, which is required for time-scale decomposition methods like CSP when explicit equations are unavailable [36].
Q4: What should I do if my model's predictions and the experimental observation are in conflict for a specific perturbation?
A systematic troubleshooting protocol is essential [10]:
- Repeat the Experiment: If cost and time permit, repeat the experiment to rule out simple human error.
- Verify Biological Plausibility: Revisit the scientific literature. The unexpected result could be a true biological phenomenon (e.g., the protein is not expressed in that tissue) rather than a model error [10].
- Check Controls: Ensure you have appropriate positive and negative controls. If a positive control also fails, the issue likely lies with the protocol or reagents, not the model [10].
- Audit Equipment and Reagents: Check for improper storage or expired reagents. Visually inspect solutions for precipitates or cloudiness [10].
- Change Variables Systematically: If the experimental protocol is suspect, generate a list of variables (e.g., concentration, incubation time) and test them one at a time, starting with the easiest to change [10].
Q5: What is the advantage of using a genetic algorithm for model refinement compared to manual curation?
Genetic algorithms (GAs) streamline and automate the labor-intensive, trial-and-error process of manual model refinement [7]. A GA-based workflow like boolmore can systematically explore a vast space of possible model configurations (Boolean functions) that are consistent with biological constraints. It efficiently identifies high-fitness models that agree with a large compendium of perturbation-observation pairs, a process that would be prohibitively slow for a human. This can lead to significant accuracy gains in a fraction of the time, as demonstrated by a refinement that surpassed the improvements achieved over two years of manual revision [7].
Experimental Protocols
Protocol: Refining Boolean Models with Perturbation-Observation Pairs
This protocol uses the boolmore workflow to refine a starting Boolean model against a corpus of experimental data [7].
I. Input Preparation
- Starting Model: Prepare a baseline Boolean model (interaction graph and Boolean functions). This graph is considered biologically plausible but may have inaccuracies.
- Biological Mechanisms: Formalize known biological constraints as logical relations (e.g., "A is necessary for B," "C inhibits D").
- Perturbation-Observation Pairs: Curate experimental results into a structured list. Categorize each observation as:
- OFF: The node is inactive/not expressed.
- ON: The node is active/expressed.
- Some: An intermediate level of activation [7].
II. Genetic Algorithm Execution
- Mutation: The algorithm generates new candidate models by mutating the Boolean functions of the starting model. The mutation is constrained to preserve the input biological knowledge and the signs of the edges in the interaction graph.
- Crossover: Create new models by randomly combining regulatory functions from two high-performing parent models.
- Prediction: For each candidate model, calculate its long-term behavior (minimal trap spaces) under each experimental perturbation setting.
- Fitness Scoring: Quantify the model's agreement with all perturbation-observation pairs. Scoring is hierarchical, meaning a model must agree with single-perturbation data to get credit for double-perturbation results.
- Selection: The models with the highest fitness scores are retained for the next iteration, with a preference for models that use fewer added edges.
III. Output and Validation
- Refined Models: Select the top-performing models from the algorithm.
- Testable Predictions: Analyze the refined models to generate new, experimentally testable hypotheses about the system.
- Validation: Test the refined model's predictions against a held-out validation set of experimental data not used in the training process.
Protocol: Handling Multi-Scale Data for Continuous Model Identification
This protocol is for identifying governing equations from multi-scale observational data using a hybrid CSP-SINDy framework [36].
I. Data Collection and Preprocessing
- Collect time-series data for the system of interest. The data should capture dynamics across multiple time scales.
- Preprocess the data to handle noise and missing points if necessary.
II. Time-Scale Decomposition with CSP
- Jacobian Estimation: Use Neural Ordinary Differential Equations (NODE) and Neural Networks to estimate the Jacobian matrix of the system directly from the observational data [36].
- Regime Identification: Apply the Computational Singular Perturbation (CSP) algorithm to the data and the estimated Jacobian. CSP will decompose the tangent space and identify time scales, allowing you to partition the dataset into subsets where the dynamics are similar [36].
III. Local Model Identification with SINDy
- Library Construction: For each data subset identified by CSP, create a library of candidate basis functions (e.g., polynomials, trigonometric functions) that could describe the dynamics.
- Sparse Regression: Apply the SINDy algorithm to each data subset. SINDy performs sparse regression to identify a minimal set of functions from the library that best capture the dynamics in that specific regime [36].
- Model Validation: Validate the identified reduced models by comparing their simulations to the original data within each subset and against any held-out validation data.
Workflow and Signaling Pathway Diagrams
boolmore Refinement Workflow
Multi-Scale Data Integration
Research Reagent Solutions
The following table details key computational tools and their functions for model refinement.
| Tool/Reagent | Primary Function | Key Feature / Application Context |
|---|---|---|
| boolmore [7] | Refines Boolean models using a genetic algorithm. | Optimizes model agreement with perturbation-observation pairs; constrains search to biologically plausible models. |
| SINDy [36] | Identifies governing equations from time-series data. | Uses sparse regression to find parsimonious (simple) models; good for interpretable, equation-based modeling. |
| Computational Singular Perturbation (CSP) [36] | Decomposes multi-scale dynamics. | Partitions datasets into regimes of similar dynamics; essential for identifying reduced models in complex systems. |
| Neural ODEs [36] | Learns continuous-time dynamics from data. | Estimates the vector field (and Jacobian) of a system; useful when explicit equations are unknown. |
| RefineLab [37] | Refines QA datasets under a token budget. | Applies selective edits to improve dataset quality (coverage, difficulty); useful for preparing validation data. |
| Flat-Bottom Restraints [38] | Used in MD simulation for protein refinement. | Allows conformational sampling away from the initial model while preventing excessive unfolding. |
Quantitative Systems Pharmacology (QSP) and PBPK Models for Dosage Optimization
► FAQ: Core Concepts and Applications
What is the fundamental difference between a QSP and a PBPK model?
While both are mechanistic modeling approaches used in drug development, their primary focus differs. PBPK (Physiologically Based Pharmacokinetic) models primarily describe what the body does to the drug—the Absorption, Distribution, Metabolism, and Excretion (ADME) processes based on physiological parameters and drug properties [39] [40]. QSP (Quantitative Systems Pharmacology) models have a broader scope, integrating systems biology with pharmacology to also describe what the drug does to the body. They combine mechanistic models of disease pathophysiology with pharmacokinetics and pharmacodynamics to predict a drug's systems-level efficacy and safety [41] [42].
When should I consider a QSP approach over traditional PK/PD modeling for dose optimization?
A QSP approach is particularly valuable when:
- Your question cannot be solved by standard Pharmacokinetic/Pharmacodynamic (PKPD) methods, such as understanding the mechanistic basis for a biomarker response or explaining an observed lack of efficacy [43].
- You need to integrate high-dimensional data (e.g., -omics) and account for complex, non-linear biological pathways and network interactions [41].
- The goal is to extrapolate outside clinically studied scenarios, for instance, for personalized dosing in rare diseases or predicting long-term outcomes from short-term data [44] [40].
How can these models inform dosing for novel therapeutic modalities like gene therapies?
QSP and PBPK are critical for dose selection in data-sparse areas like gene therapy. For example:
- AAV Gene Therapy: PBPK models can describe AAV vector biodistribution and transduction, while QSP models integrate this with transgene expression and pharmacodynamic effects to predict durable responses from a single dose [44] [39].
- CRISPR/Cas9 (LNP-delivered): A mechanistic QSP model was developed for NTLA-2001, capturing the lipid nanoparticle (LNP) pharmacokinetics and the subsequent knockdown of the target protein (transthyretin) to support first-in-human dose predictions [44].
- mRNA Therapeutics: Multiscale QSP frameworks can link intracellular processes (mRNA internalization, endosomal escape, antigen translation) with tissue-level immune dynamics to optimize dosing regimens [44].
► FAQ: Model Development and Best Practices
What are the key considerations for choosing the right level of granularity in a QSP model?
Selecting the appropriate model complexity is a critical step. The granularity should be gauged based on the following criteria [43]:
- Need: The model's complexity should be justified by a question that simpler models cannot answer.
- Prior Knowledge: The availability of quantitative biological, physiological, and pharmacological data to inform and calibrate the model.
- Pharmacology: The use of multiple pharmacological interventions (e.g., different compounds) to "probe" the system and validate the model structure.
- Translation: The ability to translate findings from preclinical species to humans by accounting for interspecies physiological differences.
- Collaboration: Long-term integration with experimental labs is essential to close the loop between model predictions, new experiments, and model refinement.
My model has many parameters but limited data. How can I address parameter identifiability and uncertainty?
Parameter estimation for complex QSP and PBPK models is a recognized challenge. A robust approach involves [43] [45]:
- Using Multiple Algorithms: Do not rely on a single method. Employ a combination of algorithms (e.g., quasi-Newton, Nelder-Mead, genetic algorithms, particle swarm optimization) and compare the results.
- Testing Different Conditions: Conduct multiple rounds of parameter estimation under different initial values to see if the solution converges to the same point.
- Assessing Practical Identifiability: Use techniques like profile likelihood or Markov Chain Monte Carlo (MCMC) approaches to explore the distribution of parameters and identify those that are poorly constrained by the available data.
- Model Reduction: Apply variable lumping or other reduction techniques to simplify the model to a more manageable form without sacrificing its predictive power for the key questions.
► TROUBLESHOOTING GUIDES
Problem: Model Results Are Not Reproducible or Reusable
Potential Causes and Solutions:
- Cause 1: Inadequate model documentation. The purpose, scope, and underlying assumptions of the model are not clearly stated [46].
- Solution: Adopt a minimum set of documentation standards. Clearly declare the scientific question the model addresses, all model assumptions, and the contexts for which it is (and is not) suitable.
- Cause 2: Model code or files are missing, poorly annotated, or do not match the publication.
- Solution: Use standardized markup languages (SBML, CellML) and share the fully annotated model code. Ensure the provided code can reproduce the results presented in the publication [46].
- Cause 3: Parameter values, including units and uncertainty, are omitted or scattered.
- Solution: Provide a complete and consolidated list of all parameter values, their units, and their sources (e.g., experimental data, literature, estimation) [46].
Problem: High Predictive Uncertainty in Dose Projections
Potential Causes and Solutions:
- Cause 1: The model was not properly qualified for its Context of Use (COU).
- Solution: Implement a credibility assessment framework. Demonstrate the model's predictive capability within a specific COU by showing it can recapitulate a dataset not used for model calibration [40].
- Cause 2: Key physiological or system-specific parameters are missing for your target population.
- Cause 3: The model is over-extrapolating beyond its validated scope.
- Solution: Clearly define the boundaries of the model. Avoid using a model developed for one disease or patient population to make predictions for another without proper validation and, if needed, model refinement [46].
► THE SCIENTIST'S TOOLKIT
The following tools and concepts are fundamental for conducting rigorous QSP and PBPK research.
| Tool / Resource | Function / Description |
|---|---|
| Standardized Markup Languages (SBML, CellML, PharmML) | Encodes models in a standardized, interoperable format, promoting reproducibility and reuse across different software platforms [46]. |
| Model Repositories (BioModels, CellML, DDMore) | Public databases to find, share, and access previously published models, facilitating model reuse and community validation [46]. |
| Parameter Estimation Algorithms (e.g., Cluster Gauss-Newton, Genetic Algorithm) | Software algorithms used to estimate model parameters by minimizing the difference between model simulations and observed data [45]. |
| Sensitivity Analysis | A mathematical technique used to identify which model parameters have the greatest influence on the model outputs, guiding data collection efforts [43]. |
| Qualified PBPK Platform (e.g., GastroPlus, PK-Sim, Simcyp) | A software environment that has undergone validation and qualification for specific Contexts of Use, ensuring trust in its predictive capabilities [40]. |
| Virtual Population (Virtual Twin) Generation | A method to create a large cohort of in silico patients with realistic physiological variability, used to simulate clinical trials and personalize therapies [44] [47]. |
► EXPERIMENTAL PROTOCOLS & WORKFLOWS
Protocol 1: Workflow for Developing and Qualifying a QSP Model for Dose Optimization
This protocol outlines a step-by-step methodology for building a credible QSP model to support dosage selection.
1. Define Question and Context of Use (COU):
- Precisely state the drug development question the model will answer (e.g., "Predict the optimal starting dose for a novel AAV gene therapy in pediatric patients").
- Define the COU, which specifies the model's purpose, the populations, and the interventions it will simulate [40].
2. Assemble Prior Knowledge and Data:
- Gather all available quantitative data on the system: pathway kinetics, receptor densities, physiological rates, and disease mechanisms [43].
- Collect drug-specific data: PK, target binding affinity, and in vitro efficacy data.
- Identify and document all knowledge gaps and underlying assumptions [46].
3. Model Building and Granularity Selection:
- Develop the mathematical structure (e.g., ordinary differential equations) representing the biological system and drug action.
- Choose the model granularity based on the predefined "Need" and available "Prior Knowledge" [43]. The diagram below illustrates a generalized QSP model refinement workflow that balances these factors.
4. Parameter Estimation and Calibration:
- Use parameter estimation algorithms to fit model parameters to the assembled data.
- Critically assess parameter identifiability using methods like profile likelihood to understand uncertainty [43] [45].
5. Model Validation and Qualification:
- Test the model's predictive power against a dataset not used for calibration (e.g., a different clinical study or competing drug data).
- If the model can reproduce these external data, it is considered qualified for its specific COU [40].
A Decision Framework for Selecting a Parameter Estimation Algorithm
Given that the performance of estimation algorithms depends on model structure, using a systematic approach to select an algorithm is crucial. The table below summarizes the performance characteristics of common methods based on a published assessment [45].
| Algorithm | Typical Performance & Characteristics | Best Suited For |
|---|---|---|
| Quasi-Newton Method | Converges quickly if starting near solution; performance highly sensitive to initial values. | Models with good initial parameter estimates and a relatively smooth objective function. |
| Nelder-Mead Method | A direct search method; can be effective for problems with noisy objective functions. | Models where derivative information is difficult or expensive to compute. |
| Genetic Algorithm (GA) | A global search method; less sensitive to initial values but computationally intensive. | Complex models with many parameters and potential local minima. |
| Particle Swarm Optimization (PSO) | Another global optimization method; often effective for high-dimensional problems. | Similar use cases to GA; performance can vary, so testing both is recommended. |
| Cluster Gauss-Newton Method (CGNM) | Designed for problems where parameters are not uniquely identifiable; can find multiple solutions. | Models with high parameter correlation or non-identifiability issues. |
General Recommendation: To obtain credible results, conduct multiple rounds of estimation using different algorithms and initial values [45].
Technical Support Center: Frequently Asked Questions (FAQs)
FAQ 1: What is the primary function of a Genome Variant Refinement Pipeline (GVRP)? A Genome Variant Refinement Pipeline (GVRP) is a computational tool designed to process and refine Variant Call Format (VCF) files. Its core function is to separate analysis code from the pipeline infrastructure, allowing researchers to either reenact specific results from a paper or use the pipeline directly for refining variants in their own VCF files, including functionalities for input, output, and optional deletion of variants [48].
FAQ 2: Our pipeline's accuracy is below target for our low-accuracy targets research. What are the most common root causes? Suboptimal model accuracy in bioinformatics pipelines often stems from foundational data quality issues rather than complex algorithmic failures. The most frequent culprits include [49]:
- Poor Data Quality: Missing values, inconsistent data formats, and outliers in your input data can severely confuse the model during training.
- Suboptimal Feature Engineering: The presence of irrelevant or redundant features introduces noise, while a lack of meaningful, domain-specific engineered features can prevent the model from learning critical patterns.
- Incorrect Model Selection: Using an algorithm unsuited to the specific problem type (e.g., using a model designed for germline variants on somatic data) limits potential accuracy.
FAQ 3: What are the critical pre-processing steps to ensure variant calling accuracy? Adequate pre-processing of sequencing data is crucial for accurate variant calling. The recommended steps include [50] [51]:
- Read Alignment: Aligning raw sequencing reads (FASTQ) to a reference genome using tools like BWA-MEM.
- Duplicate Marking: Identifying and marking PCR duplicate reads using tools like Picard or Sambamba to prevent them from skewing variant counts.
- Quality Control (QC): Performing routine QC on the resulting BAM files to verify sequencing coverage, check for sample contamination, and confirm expected sample relationships in family or tumor-normal studies.
FAQ 4: How can I benchmark my refined variant calls to ensure they are reliable? To evaluate the accuracy of your variant calls, you should use publicly available benchmark datasets where the "true" variants are known. The most widely used resource is the Genome in a Bottle (GIAB) consortium dataset, which provides a set of "ground truth" small variant calls for specific human samples. These resources also define "high-confidence" regions of the human genome where variant calls can be reliably benchmarked [50].
Troubleshooting Guide: Common Scenarios and Solutions
Problem: High False Positive Variant Calls
- Symptoms: An unusually high number of variant calls, many of which are likely artifacts.
- Possible Causes: Inadequate alignment, failure to mark PCR duplicates, or sequencing artifacts from low-quality samples (e.g., FFPE-derived DNA) [51].
- Solutions:
- Verify Pre-processing: Ensure your pipeline includes duplicate marking and consider local realignment around indels, though the latter may offer marginal improvements for high computational cost [50].
- Check Sample Quality: For clinical samples like FFPE tissue, use repair enzymes to address formalin-induced DNA damage, which can be mistaken for low-frequency mutations [51].
- Apply Rigorous Filtering: Use the GVRP's functionality to delete false variants from the VCF file based on quality scores and other metrics [48].
Problem: Low Sensitivity in Detecting Structural Variants (SVs)
- Symptoms: The pipeline misses large deletions, duplications, or other structural variants.
- Possible Causes: Using a variant caller designed only for single nucleotide variants (SNVs) and small indels. Short-read sequencing technology may also be unable to span large, complex variations [51].
- Solutions:
- Use Specialized Callers: Employ variant callers specifically designed for structural variants, such as DELLY, Lumpy, or Manta [50].
- Consider Sequencing Strategy: For projects where SVs are a priority, consider using long-read sequencing technologies, which are more effective for detecting large variants [51].
- Combine Multiple Tools: Since no single tool is optimal for all variant types, consider consolidating variant call sets from multiple specialized tools to improve sensitivity [51].
Problem: Inconsistent Results When Re-running the Pipeline
- Symptoms: The pipeline produces different variant calls when executed multiple times with the same input data.
- Possible Causes: This can be due to random elements in the model or issues with the training data, such as overfitting, where the model has memorized the training examples rather than learning generalizable patterns [49].
- Solutions:
- Prevent Overfitting: Implement techniques like regularization (L1/L2) and use cross-validation to ensure your model's performance is robust and not dependent on a specific data split [49].
- Ensure Data Consistency: Check that your input data is consistently formatted and that all pre-processing steps are reproducible.
Experimental Protocols for Pipeline Optimization
Protocol 1: Optimizing Data Pre-processing for Variant Calling
Objective: To enhance the quality of input data (BAM files) for improved variant calling accuracy, a critical step in refining low-accuracy targets.
Methodology:
- Read Alignment: Align raw FASTQ files to a reference genome (e.g., GRCh38) using the BWA-MEM aligner [50].
- Duplicate Marking: Process the resulting BAM file with Picard Tools to identify and mark duplicate reads, which are then excluded from variant calling [50].
- Quality Control: Use BEDTools and QualiMap to evaluate key sequencing metrics, including the average depth of coverage and the percentage of the target region covered at a minimum depth (e.g., 20x) [50].
- Sample Verification: For family or paired samples, use the KING algorithm to confirm expected genetic relationships and VerifyBamID to check for sample contamination [50].
Protocol 2: A Multi-Tool Approach for Comprehensive Variant Calling
Objective: To maximize the sensitivity and specificity for detecting different variant classes (SNVs, Indels, SVs) by integrating multiple best-in-class variant callers.
Methodology:
- Germline SNVs/Indels: Call variants using
GATK HaplotypeCallerorFreeBayeson your pre-processed BAM file [50]. - Somatic Mutations: For tumor-normal pairs, use a somatic-specific caller like
MuTect2,Strelka2, orVarScan2[50]. - Structural Variants: Call SVs using a dedicated tool such as
DELLYorManta[50]. - Data Integration: Combine the variant call sets from the different tools. The GVRP can then be applied to refine this consolidated VCF file, filtering out false positives and organizing the data [48] [51].
Workflow and Signaling Pathway Visualizations
Genome Variant Refinement Pipeline (GVRP) Workflow
The following diagram illustrates the logical flow and key stages of a typical Genome Variant Refinement Pipeline, integrating best practices for data pre-processing and variant refinement [50] [48].
Variant Caller Selection Logic
This diagram outlines the decision-making process for selecting the appropriate variant calling tool based on the research question and variant type, which is crucial for optimizing model refinement [50] [51].
The following table details key software tools and reference materials essential for building and optimizing a Genome Variant Refinement Pipeline [50] [48] [51].
Table 1: Key Resources for a Genome Variant Refinement Pipeline
| Item Name | Type | Primary Function in GVRP | Usage Notes |
|---|---|---|---|
| BWA-MEM | Software | Read alignment of sequencing reads to a reference genome. | Preferred aligner for most clinical sequencing studies; balances speed and accuracy [50]. |
| Picard Tools | Software | Identifies and marks PCR duplicate reads in BAM files. | Prevents duplicates from skewing variant allele frequencies [50]. |
| GATK HaplotypeCaller | Software | Calls germline SNPs and indels via local re-assembly of haplotypes. | A best-practice tool for germline variant discovery [50]. |
| MuTect2 / Strelka2 | Software | Calls somatic SNVs and indels from tumor-normal sample pairs. | Specifically designed to handle tumor heterogeneity and low variant allele fractions [50]. |
| DELLY | Software | Calls structural variants (SVs) such as deletions, duplications, and translocations. | Used for detecting larger, more complex variants that SNV callers miss [50]. |
| Genome in a Bottle (GIAB) | Reference | Provides benchmark variant calls for a set of human genomes. | Used to validate and benchmark pipeline performance against a "ground truth" [50]. |
| Python 3.11 | Software | Core programming language for running the GVRP. | Required environment; all necessary libraries are listed in requirements.txt [48]. |
| DeepVariant | Software | A deep learning-based variant caller that can generate the initial VCF files for GVRP refinement. | Cited as the source of VCF files for the GVRP [48]. |
Table 2: Comparison of Sequencing Strategies for Variant Detection [50]
| Strategy | Target Space | Average Read Depth | SNV/Indel Detection | CNV Detection | SV Detection | Low VAF Detection |
|---|---|---|---|---|---|---|
| Panel | ~ 0.5 Mbp | 500–1000x | ++ | + | – | ++ |
| Exome | ~ 50 Mbp | 100–150x | ++ | + | – | + |
| Genome | ~ 3200 Mbp | 30–60x | ++ | ++ | + | + |
Performance is indicated as good (+), outstanding (++), or poor/absent (–). VAF: Variant Allele Frequency.
Table 3: Recommended Software Tools for Different Variant Types [50]
| Variant Class | Analysis Type | Recommended Tools |
|---|---|---|
| SNVs/Indels | Inherited | FreeBayes, GATK HaplotypeCaller, Platypus |
| SNVs/Indels | Somatic | MuSE, MuTect2, SomaticSniper, Strelka2, VarDict, VarScan2 |
| Copy Number Variants (CNVs) | Both | cn.MOPS, CONTRA, ExomeDepth, XHMM |
| Structural Variants (SVs) | Both | DELLY, Lumpy, Manta, Pindel |
Navigating Pitfalls: Strategies for Robust and Biologically Plausible Refinement
Troubleshooting Guides
Guide 1: Diagnosing and Resolving Model Underfitting
Problem: Your model shows poor performance on both training and validation data, indicating it has failed to capture the underlying patterns in the dataset. This is a common challenge when optimizing models for low-accuracy targets, where initial performance is often weak.
Diagnosis Checklist:
- Confirm high error rates on both training and validation sets.
- Check if the model is too simple for the problem's complexity (e.g., using linear regression for a highly non-linear problem).
- Verify if feature engineering is adequate or if key predictive features are missing.
- Determine if the model was trained for a sufficient number of epochs or with overly aggressive regularization.
Solution Protocol: A systematic approach to increasing model learning capacity.
- Step 1: Increase Model Complexity. Transition to a more powerful algorithm (e.g., from logistic regression to a tree-based model like Random Forest or Gradient Boosting) [52]. For neural networks, add more layers or more neurons per layer [53] [52].
- Step 2: Enhance Feature Space. Perform feature engineering to create more informative input features [52] [54]. Use domain knowledge to derive new variables that may be more relevant to the low-accuracy target.
- Step 3: Reduce Regularization. Weaken constraints like L1/L2 regularization penalties that may be preventing the model from learning effectively [53] [54].
- Step 4: Increase Training Duration. Train the model for more epochs, ensuring you monitor a validation set to avoid triggering overfitting later in the process [53].
Guide 2: Diagnosing and Resolving Model Overfitting
Problem: Your model performs exceptionally well on the training data but generalizes poorly to new, unseen validation or test data. This is a critical risk when refining models for low-accuracy targets, as it can create a false impression of success.
Diagnosis Checklist:
- Confirm a large performance gap between high training accuracy and low validation accuracy.
- Check if the model is excessively complex relative to the amount of available training data.
- Verify if the training dataset is too small or lacks diversity.
- Determine if the model was trained for too many epochs without validation checks.
Solution Protocol: A multi-faceted strategy to improve model generalization.
- Step 1: Implement Regularization. Apply L1 (Lasso) or L2 (Ridge) regularization to penalize model complexity and encourage simpler, more robust models [53] [52] [55].
- Step 2: Use Data Augmentation. Artificially expand your training set by creating modified versions of your existing data [52] [55]. In drug development, this could involve adding noise or using generative AI to create high-quality synthetic data [52].
- Step 3: Apply Early Stopping. Halt the training process as soon as performance on a validation set stops improving [53] [52] [55].
- Step 4: Introduce Dropout. For neural networks, randomly disable a percentage of neurons during training to prevent over-reliance on any single node [53] [55].
- Step 5: Gather More Data. If possible, increase the size and quality of the training dataset, providing a better representation of the true underlying distribution [53] [52].
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between overfitting and underfitting? A1: Overfitting occurs when a model is too complex and memorizes the training data, including its noise and random fluctuations. It performs well on training data but poorly on new, unseen data [53] [56]. Underfitting is the opposite: the model is too simple to capture the underlying pattern in the data, resulting in poor performance on both training and new data [53] [56].
Q2: How can I quickly tell if my model is overfitting during an experiment? A2: The most telling sign is a large and growing gap between training accuracy (very high) and validation accuracy (significantly lower) [53] [52]. Monitoring learning curves that plot both metrics over time will clearly show this divergence.
Q3: My dataset is small and cannot be easily expanded. What is the most effective technique to prevent overfitting? A3: For small datasets, a combination of techniques is most effective. Data augmentation is a primary strategy to artificially expand your dataset [55]. Additionally, employ robust k-fold cross-validation to get a reliable performance estimate [52] [55], and apply regularization (L1/L2) and dropout to explicitly constrain model complexity [53] [55].
Q4: In the context of drug development, what does a "Fit-for-Purpose" model mean? A4: A "Fit-for-Purpose" (FFP) model in Model-Informed Drug Development (MIDD) is one that is closely aligned with the specific Question of Interest (QOI) and Context of Use (COU) at a given development stage [21]. It means the model's complexity and methodology are justified by its intended application, avoiding both oversimplification that leads to underfitting and unjustified complexity that leads to overfitting [21].
Q5: Is some degree of overfitting always unacceptable? A5: While significant overfitting is detrimental as it indicates poor generalization, a very small degree might be acceptable in some non-critical applications [53]. However, for rigorous research and high-stakes fields like drug development, significant overfitting should always be mitigated to ensure model reliability and regulatory acceptance [21].
Table 1: Techniques to Mitigate Underfitting
| Technique | Description | Typical Use Case |
|---|---|---|
| Increase Model Complexity | Transition to more powerful algorithms (e.g., from linear models to neural networks) or add more layers/neurons. | The model is too simple for the problem's complexity [52] [54]. |
| Feature Engineering | Create new, more informative input features from raw data based on domain knowledge. | The current feature set is insufficient to capture the underlying patterns [52]. |
| Reduce Regularization | Weaken or remove constraints (like L1/L2 penalties) that are preventing the model from learning. | Overly aggressive regularization has constrained the model [53] [54]. |
| Increase Training Epochs | Allow the model more time to learn from the data by extending the training duration. | The model has not converged and needs more learning iterations [53]. |
Table 2: Techniques to Mitigate Overfitting
| Technique | Description | Typical Use Case |
|---|---|---|
| Regularization (L1/L2) | Adds a penalty to the loss function for large weights, discouraging model complexity. | A general-purpose method to prevent complex models from memorizing data [53] [55] [57]. |
| Data Augmentation | Artificially expands the training set by creating modified copies of existing data. | The available training dataset is limited in size [52] [55]. |
| Early Stopping | Halts training when validation performance stops improving. | Preventing the model from continuing to train and over-optimize on the training data [53] [52] [55]. |
| Dropout | Randomly disables neurons during training in neural networks. | Prevents the network from becoming over-reliant on any single neuron [53] [55]. |
| Cross-Validation | Assesses model performance on different data splits to ensure generalizability. | Provides a more reliable estimate of how the model will perform on unseen data [52] [55]. |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Computational Tools for Model Refinement
| Tool / Reagent | Function / Purpose |
|---|---|
| L1/L2 Regularization | Penalizes model complexity to prevent overfitting and encourage simpler, more generalizable models [53] [55]. |
| K-Fold Cross-Validation | A resampling procedure used to evaluate a model on a limited data sample, providing a robust estimate of generalizability [52] [55]. |
| SHAP/LIME | Post-hoc explanation methods that help interpret complex model predictions, crucial for validating models in regulated environments [58] [52]. |
| Data Augmentation Pipelines | Tools to systematically generate new training examples from existing data, mitigating overfitting caused by small datasets [52] [55]. |
| Hyperparameter Tuning Suites (e.g., Optuna) | Software to automate the search for optimal model settings, systematically balancing complexity and performance [52]. |
| Physiologically Based Pharmacokinetic (PBPK) Models | A mechanistic "Fit-for-Purpose" modeling tool in drug development used to predict pharmacokinetics and inform clinical trials [21] [59]. |
In research focused on optimizing model refinement for low-accuracy targets, a central problem is navigating the vast space of potential biological mechanisms. Relying solely on output accuracy can lead to models that learn spurious correlations or biologically implausible pathways, ultimately failing to generalize. The goal is to constrain this search space to mechanisms that are not only effective but also faithful to known biology, thereby preserving biological fidelity. This technical support center provides guidelines and solutions for integrating these constraints into your research workflow.
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: What are the most common causes of biologically implausible model behavior?
- Cause: Over-reliance on Output Metrics. Optimizing a model solely for prediction accuracy on a low-accuracy target can cause it to exploit statistical noise in the training data, a phenomenon known as overfitting [60].
- Troubleshooting: Implement techniques like regularization and pruning during training to prevent overfitting and force the model to learn more generalizable, and potentially more plausible, features [60].
- Cause: Inadequate Task Specification. The prompt or training objective may be too vague, failing to articulate the desired level of biological granularity or the specific relationships to be extracted [61].
- Troubleshooting: Engage in an iterative refinement process to create a comprehensive "error ontology." This systematic framework helps classify discrepancies and forces a precise definition of what constitutes a correct, biologically plausible output [61].
FAQ 2: How can I validate that my model's internal mechanisms are biologically plausible?
- Solution: Employ mechanistic interpretation tools, such as attribution graphs, to reverse-engineer the model's internal decision-making process [62]. These tools allow you to trace the computational steps the model uses to arrive at an output. You can then perform intervention experiments, such as inhibiting specific internal features, to test if the model's behavior changes in a way consistent with your biological hypothesis [62].
FAQ 3: My model performs well on training data but poorly on new, real-world data. How can I improve its generalization?
- Solution: This is a classic sign of overfitting. Ensure your training set has sufficient volume, balance, and variety to adequately represent the different scenarios the model will encounter [60]. Furthermore, techniques like fine-tuning a pre-trained model on your specific dataset can help it adapt its existing knowledge to the new task more effectively than training from scratch, often leading to more robust performance [60].
Experimental Protocols for Ensuring Biological Fidelity
Protocol 1: Iterative Refinement and Error Ontology Development
This methodology, adapted from successful clinical AI workflows, is essential for precisely defining biologically correct outputs and refining your model accordingly [61].
- Initial Pipeline Setup: Develop an initial model and a flexible prompt template that defines the desired structured output.
- Gold-Standard Annotation: Manually create a set of "gold-standard" annotations for a small, diverse development set of data points (e.g., 152 reports or samples).
- Iterative Testing and Error Classification: Run your model on the development set and compare its outputs to the gold standard. Classify every discrepancy using a developing error ontology. Key categories include [61]:
- Report Complexities: Challenges posed by inherently ambiguous or complex data.
- Specification Issues: Ambiguity in the desired scope or granularity of the information to be extracted.
- Normalization Difficulties: Challenges in standardizing terms and handling free-text entries.
- Pipeline Refinement: Use the insights from the error ontology to refine your model, prompts, or output schema. This may involve adding explicit instructions for handling edge cases or clarifying ontological priorities.
- Final Validation: Repeat steps 3 and 4 for multiple cycles (e.g., 6 cycles) until the major error rate is minimized. The final error ontology then serves as a guide for ongoing evaluation.
Protocol 2: Circuit Tracing and Mechanistic Validation
This protocol uses model interpretability tools to directly inspect and validate the internal mechanisms of a large language model, as pioneered by AI transparency research [62].
- Model Selection: Choose a model for analysis (e.g., a model like Claude 3.5 Haiku was used in the original study [62]).
- Generate Attribution Graphs: For a given input prompt, use a circuit tracing methodology to generate an attribution graph. This graph is a representation of the model's internal computational steps, where nodes represent features (interpretable concepts) and edges represent causal interactions between them [62].
- Identify Key Subcircuits: Analyze the graph to identify groups of features (supernodes) that work together to perform a specific function, such as "Identify Candidate Diagnoses" or "Plan Rhyming Words" [62].
- Hypothesis Testing via Intervention: Formulate a hypothesis about the role of a specific subcircuit. Then, perform an intervention experiment in the original model, such as inhibiting the activation of that feature group.
- Measure Causal Impact: Observe the effect of this intervention on the model's downstream features and final output. If the effect aligns with the hypothesis generated from the attribution graph, you gain confidence that the graph has captured a real, causal mechanism within the model [62].
The workflow for this mechanistic analysis is outlined in the following diagram:
Quantitative Data and Research Reagent Solutions
Table 1: Error Ontology Refinement Metrics
The following data, based on a clinical study, demonstrates the impact of iterative refinement on model error rates. The initial error rate was reduced to less than 1% after six refinement cycles [61].
| Iteration Cycle | Major Error Rate | Primary Error Contexts Identified |
|---|---|---|
| Initial Pipeline | High (Base Rate) | Specification Issues, Normalization Difficulties |
| Cycle 3 | Significantly Reduced | Report Complexities, Ontological Nuances |
| Cycle 6 (Final) | 0.99% (14/1413 entities) | Minor normalization issues (e.g., "diffusely" vs. "diffuse") |
Research Reagent Solutions
This table lists key computational tools and their functions for implementing the described protocols.
| Tool / Solution | Function in Research | Key Rationale |
|---|---|---|
| Attribution Graphs [62] | Mechanistic interpretation and visualization of model internals. | Moves beyond the "black box" by revealing the model's computational graph and intermediate reasoning steps. |
| Error Ontology [61] | Systematic framework for classifying model discrepancies. | Provides a structured method to move from "what" information to extract to "why" an output is incorrect, guiding refinement. |
| COM-B Model / TDF [63] | Framework for analyzing implementation mechanisms in behavioral studies. | Offers a granular understanding of Capability, Opportunity, and Motivation as mediators for behavior change, useful for modeling complex biological behaviors. |
| Fine-Tuning [60] | Adapting a pre-trained model to a specific, narrow task. | Leverages existing knowledge, saving computational resources and often improving performance compared to training from scratch. |
| Pruning [60] | Removing unnecessary parameters from a neural network. | Reduces model size and complexity, which can help eliminate redundant and potentially implausible pathways. |
Table 2: Impact of a Multifaceted Implementation Strategy on Key Mediators
This data, from a study on implementing complex guidelines, shows how a multifaceted strategy can enhance key drivers of behavior, which can be analogized to training a model for reliable performance. The effect on fidelity was partially mediated by these TDF domains [63].
| Theoretical Domains Framework (TDF) Mediator | Component | Proportion of Effect Mediated (at 12 Months) |
|---|---|---|
| Skills | Capability | 41% |
| Behavioral Regulation | Capability | 35% |
| Goals | Motivation | 34% |
| Environmental Context & Resources | Opportunity | Data Not Specified |
| Social Influences | Opportunity | Data Not Specified |
FAQs and Troubleshooting Guides
FAQ: My model has achieved 95% accuracy, but upon inspection, it fails to predict any instances of the minority class. What is happening?
This is a classic symptom of the Accuracy Paradox [64] [65]. On a severely imbalanced dataset (e.g., where 95% of examples belong to one class), a model can achieve high accuracy by simply always predicting the majority class, thereby learning nothing about the minority class. In such cases, accuracy becomes a misleading metric [65].
Troubleshooting Guide:
- Audit Your Metrics: Immediately stop using accuracy. Switch to metrics that are more informative for imbalanced classes, such as:
- Confusion Matrix: Provides a breakdown of correct and incorrect predictions for each class [65].
- Precision and Recall: Precision measures exactness, while recall measures completeness for the minority class [64] [65].
- F1-Score: The harmonic mean of precision and recall, providing a single balanced metric [64] [65].
- Cohen's Kappa: Measures agreement between predictions and actual values, normalized for class imbalance [65].
- Resample Your Training Data: Apply the resampling techniques detailed in the sections below to rebalance your training set [66] [64].
FAQ: When should I use oversampling versus undersampling?
The choice often depends on the size of your dataset [65].
- Consider Undersampling when you have a very large amount of data (tens or hundreds of thousands of instances). Removing examples from the majority class can speed up training and reduce the resource footprint, but it risks discarding potentially useful information [66] [64] [65].
- Consider Oversampling when your total dataset is smaller. Generating new examples for the minority class can help the model learn its characteristics without losing any original data, though it may increase the risk of overfitting if not done carefully [64] [65].
FAQ: How can I determine the right balance ratio when resampling?
There is no universal optimal ratio. The common starting point is to resample to a perfect 1:1 balance [64]. However, the ideal ratio should be treated as a hyperparameter. It is recommended to experiment with different ratios (e.g., 1:1, 1.5:1, 2:1) and evaluate the performance on a held-out validation set using metrics like F1-score to find the best balance for your specific problem [66].
The following tables provide a structured overview of core strategies for handling class imbalance.
Table 1: Comparison of Key Resampling Techniques
| Technique | Type | Brief Description | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Random Undersampling [64] | Undersampling | Randomly removes examples from the majority class. | Simple, fast, reduces dataset size and training time. | Can discard potentially useful information, leading to a loss of model performance. |
| Random Oversampling [64] | Oversampling | Randomly duplicates examples from the minority class. | Simple, fast, retains all original information. | Can cause overfitting as the model sees exact copies of minority samples. |
| SMOTE (Synthetic Minority Oversampling Technique) [64] [67] | Oversampling | Creates synthetic minority examples by interpolating between existing ones. | Reduces risk of overfitting compared to random oversampling, helps the model generalize better. | Can generate noisy samples if the minority class decision boundary is highly non-linear. |
| Tomek Links [64] [67] | Undersampling (Data Cleaning) | Removes majority class examples that are closest neighbors to minority class examples. | Cleans the decision boundary, can be combined with other techniques (e.g., SMOTE). | Primarily a cleaning method; often insufficient to fully balance a dataset on its own. |
Table 2: Evaluation Metrics for Imbalanced Classification
| Metric | Formula / Principle | Interpretation and Use Case |
|---|---|---|
| Precision [64] [65] | ( \text{Precision} = \frac{TP}{TP + FP} ) | Answers: "When the model predicts the positive class, how often is it correct?" Use when the cost of False Positives (FP) is high (e.g., spam detection). |
| Recall (Sensitivity) [64] [65] | ( \text{Recall} = \frac{TP}{TP + FN} ) | Answers: "Of all the actual positive instances, how many did the model find?" Use when the cost of False Negatives (FN) is high (e.g., fraud detection, disease screening). |
| F1-Score [64] [65] | ( \text{F1} = 2 \times \frac{\text{Precision} \times \text{Recall}}{\text{Precision} + \Recall} ) | The harmonic mean of Precision and Recall. Provides a single score to balance the two concerns. |
| Cohen's Kappa [65] | Measures agreement between raters, corrected for chance. | A score that accounts for the possibility of correct predictions by luck due to class imbalance. More reliable than accuracy. |
Experimental Protocols for Model Refinement
This section provides detailed methodologies for implementing key strategies to improve model performance on imbalanced data.
Protocol 1: Implementing Downsampling and Upweighting
This two-step technique separates the goal of learning the features of each class from learning the true class distribution, leading to a better-performing and more calibrated model [66].
- Downsample the Majority Class: Artificially create a more balanced training set by randomly selecting a subset of the majority class examples. The downsampling factor is a hyperparameter; a factor of 25 could transform a 99:1 imbalance to an 80:20 ratio [66].
- Upweight the Downsampled Class: To correct the bias introduced by the artificial balance, apply a weight to the loss function for every majority class example. The weight is typically the same as the downsampling factor (e.g., a factor of 25). This means a misclassification of a majority class example is treated as 25 times more costly, teaching the model the true prevalence of the classes [66].
Protocol 2: Synthetic Sample Generation with SMOTE
This protocol is used to generate synthetic samples for the minority class to avoid the overfitting associated with simple duplication [64].
- Identification: For each example ( \mathbf{x}_i ) in the minority class, identify its ( k )-nearest neighbors (typically k=5) belonging to the same class.
- Synthesis: For each of these examples ( \mathbf{x}i ), select one of its ( k ) nearest neighbors, ( \mathbf{x}{zi} ), at random.
- Interpolation: Generate a new synthetic example ( \mathbf{x}{\text{new}} ) by interpolating between ( \mathbf{x}i ) and ( \mathbf{x}{zi} ): ( \mathbf{x}{\text{new}} = \mathbf{x}i + \lambda (\mathbf{x}{zi} - \mathbf{x}_i) ) where ( \lambda ) is a random number between 0 and 1. This creates a new point along the line segment connecting the two original examples in the feature space.
Protocol 3: Algorithm Spot-Checking and Penalized Learning
- Algorithm Spot-Checking: Do not rely on a single algorithm. It is crucial to test a variety of models, as they handle imbalance differently. Decision tree-based algorithms (e.g., C4.5, C5.0, CART, Random Forest) often perform well because their splitting rules can force both classes to be addressed [65].
- Penalized Models: Many algorithms can be used in a penalized mode, where an additional cost is imposed on the model for misclassifying the minority class during training. This biases the model to pay more attention to the minority class. This can be implemented by:
- Using built-in class weight parameters (e.g.,
class_weight='balanced'in scikit-learn). - Wrapping algorithms in a cost-sensitive classifier that applies a custom penalty matrix [65].
- Using built-in class weight parameters (e.g.,
Workflow Visualization
The following diagrams illustrate the logical relationships and workflows for the strategies discussed.
The Scientist's Toolkit: Essential Research Reagents and Solutions
This table details key software tools and libraries essential for implementing the strategies outlined in this guide.
Table 3: Key Research Reagent Solutions for Imbalanced Data
| Item Name | Type | Function/Brief Explanation |
|---|---|---|
| imbalanced-learn (imblearn) [64] [67] | Python Library | A scikit-learn-contrib library providing a wide array of resampling techniques, including SMOTE, ADASYN, RandomUnderSampler, and Tomek Links. It is the standard tool for data-level balancing in Python. |
| Cost-Sensitive Classifier [65] | Algorithm Wrapper | A meta-classifier (e.g., as implemented in Weka) that can wrap any standard classifier and apply a custom cost matrix, making the underlying algorithm penalize mistakes on the minority class more heavily. |
| XGBoost / Random Forest [64] [65] | Algorithm | Tree-based ensemble algorithms that often perform well on imbalanced data due to their hierarchical splitting structure. They also typically have built-in parameters to adjust class weights for cost-sensitive learning. |
| scikit-learn [64] [67] | Python Library | Provides the foundation for model building and, crucially, offers a comprehensive suite of evaluation metrics (precision, recall, F1, ROC-AUC) that are essential for properly assessing model performance on imbalanced data. |
In drug development and AI model refinement, the Fit-for-Purpose (FFP) framework ensures that the tools and methodologies selected are perfectly aligned with the specific questions of interest and the context of use at each development stage. This strategic alignment is crucial for optimizing model refinement, especially when working with low-accuracy targets where resource allocation and methodological precision are paramount. The core principle of FFP is that a model or method must be appropriate for the specific decision it aims to support, avoiding both oversimplification and unnecessary complexity [21].
For researchers focusing on low-accuracy targets, this framework provides a structured approach to selecting optimization techniques, experimental designs, and validation methods that maximize the probability of success while efficiently utilizing limited resources. By systematically applying FFP principles, scientists can navigate the complex trade-offs between model accuracy, computational efficiency, and biological relevance throughout the drug development pipeline.
Frequently Asked Questions
What does "Fit-for-Purpose" mean in practical terms for my research? A Fit-for-Purpose approach means that the models, tools, and study designs you select must be directly aligned with your specific research question and context of use [21]. For low-accuracy target research, this involves choosing optimization techniques that address your specific accuracy limitations rather than applying generic solutions. For example, if your model suffers from high false positive rates in early detection, your FFP approach would prioritize techniques that specifically enhance specificity rather than overall accuracy.
How do I determine if a model is truly Fit-for-Purpose? Evaluate your model against these key criteria [21]:
- Clearly defined Context of Use (COU) and Questions of Interest (QOI)
- Appropriate for the specific development stage (discovery, preclinical, clinical)
- Properly validated for your specific low-accuracy target scenario
- Capable of generating reliable evidence for decision-making
- Balanced in complexity - neither oversimplified nor unnecessarily complex
What are common pitfalls when applying FFP to low-accuracy targets? Researchers often encounter these challenges [21]:
- Oversimplification: Using models that cannot capture the complexity of low-accuracy targets
- Insufficient data quality or quantity: Applying sophisticated methods to inadequate datasets
- Scope creep: Expanding the model's purpose beyond its original design
- Validation gaps: Failing to properly verify model performance for the specific context of use
Which optimization techniques are most suitable for improving low-accuracy models? For low-accuracy targets, these techniques have proven effective [60] [7]:
- Hyperparameter optimization (Grid search, Random search, Bayesian optimization)
- Model pruning to remove unnecessary parameters
- Quantization methods to reduce computational complexity
- Genetic algorithm-based refinement for systematic model improvement
- Transfer learning to leverage knowledge from related domains
Troubleshooting Common Experimental Issues
Poor Model Performance Despite Extensive Training
Problem: Your model consistently shows low accuracy even after extensive training cycles and parameter adjustments.
Solution: Implement a systematic optimization workflow:
Apply automated model refinement using genetic algorithms that adjust model functions to enhance agreement with experimental data [7]. The boolmore workflow has demonstrated improvement from 49% to 99% accuracy in benchmark studies.
Utilize hyperparameter optimization techniques including Bayesian optimization to find optimal learning rates, batch sizes, and architectural parameters [60].
Implement quantization methods to maintain performance while reducing model size by 75% or more, which can paradoxically improve effective accuracy for specific tasks [60].
Experimental Protocol:
- Start with a baseline model and define evaluation metrics specific to your low-accuracy target
- Apply genetic algorithm-based refinement with mutation and crossover operations
- Score model fitness by comparing predictions to perturbation-observation pairs
- Retain top-performing models while preferring simpler solutions
- Validate on held-out data to ensure improvements generalize
High Computational Costs Limiting Experimentation
Problem: Model refinement and optimization processes require excessive computational resources, limiting the scope of experiments.
Solution: Deploy efficiency-focused optimization strategies:
Apply parameter-efficient fine-tuning (PEFT) methods like QLoRA, which enables model adaptation using significantly reduced resources [68].
Implement post-training quantization to create GPU-optimized (GPTQ) and CPU-optimized (GGUF) model versions [68]. Benchmark tests show GGUF formats can achieve 18× faster inference with over 90% reduced RAM consumption.
Use model pruning strategies to remove unnecessary connections and parameters without significantly affecting performance [60].
Performance Comparison of Optimization Techniques:
| Technique | Accuracy Impact | Memory Reduction | Speed Improvement | Best Use Cases |
|---|---|---|---|---|
| QLoRA Fine-tuning | Maintains >99% of original | Up to 75% | Similar to baseline | Domain adaptation |
| 4-bit GPTQ Quantization | <1% loss typical | 41% VRAM reduction | May slow inference on older GPUs | GPU deployment |
| GGUF Quantization | Minimal loss | >90% RAM reduction | 18× faster inference | CPU deployment |
| Model Pruning | Maintains performance | Significant | Improved | All model types |
| Genetic Algorithm Refinement | 49% to 99% improvement | Varies | Slower training | Low-accuracy targets |
Difficulty Translating Model Improvements to Biological Relevance
Problem: Model metrics improve during optimization, but the changes don't translate to meaningful biological insights or practical applications.
Solution: Implement biological constraint integration:
Incorporate domain knowledge as logical constraints during model refinement to maintain biological plausibility [7]. The boolmore workflow demonstrates how biological mechanisms can be expressed as logical relations that limit search space to meaningful solutions.
Utilize causal modeling approaches that formulate reasoning as selection mechanisms, where high-level logical concepts act as operators constraining observed inputs [69].
Apply reflective representation learning that incorporates estimated latent variables as feedback, facilitating learning of dense dependencies among biological representations [69].
Experimental Protocol for Biologically Relevant Optimization:
- Define biological constraints and logical relationships as formal rules
- Implement reflective representation learning to capture complex dependencies
- Use dependency self-refinement to ensure solutions satisfy biological constraints
- Apply periodic intermediate alignment to maintain biological relevance during training
- Validate against perturbation-observation pairs with biological significance
Experimental Protocols for Key Methodologies
Genetic Algorithm-Based Model Refinement
This protocol is adapted from the boolmore workflow for automated model refinement [7]:
Materials and Reagents:
- Baseline model with defined interaction graph
- Curated perturbation-observation pairs
- Biological constraint definitions
- Computational environment supporting genetic algorithms
Procedure:
- Input Preparation:
- Define starting model architecture and parameters
- Formalize biological mechanisms as logical relations
- Categorize experimental results into OFF, ON, and intermediate activation states
Model Mutation:
- Apply stochastic mutation to model functions while preserving biological constraints
- Generate crossover models by combining elements from parent models
- Maintain consistency with starting interaction graph unless edge addition is permitted
Fitness Evaluation:
- Calculate minimal trap spaces for each model under different settings
- Identify nodes that are ON, OFF, or oscillate
- Compute fitness scores by quantifying agreement with perturbation-observation data
Selection and Iteration:
- Retain models with top fitness scores
- Prefer models with fewer added edges to maintain simplicity
- Iterate through mutation-evaluation-selection cycles until convergence
Validation:
- Test refined models on held-out validation data
- Ensure improvements generalize beyond training set
- Verify biological plausibility of refined models
Parameter-Efficient Fine-Tuning with Quantization
This protocol enables significant model optimization with reduced computational requirements [68]:
Materials and Reagents:
- Pretrained base model (e.g., Llama 3.2 1B parameters)
- Domain-specific dataset (synthetic or real)
- QLoRA implementation framework
- Quantization tools (GPTQ, GGUF converters)
Procedure:
- QLoRA Fine-tuning:
- Quantize base model to 4-bit precision using NormalFloat4 (NF4) data type
- Inject trainable low-rank adapters while freezing base model weights
- Train with paged optimizers to handle memory spikes
- Use lower learning rate to preserve pretrained knowledge
Domain Specialization:
- Curate or generate task-specific data matching target domain
- Apply metaprompting for synthetic data generation if real data is limited
- Focus training on domain-specific objectives rather than general capabilities
Post-Training Quantization:
- For GPU deployment: Apply GPTQ for inference optimization
- For CPU deployment: Convert to GGUF format with appropriate quantization levels
- Validate quantized model performance against full-precision version
Performance Benchmarking:
- Measure accuracy on domain-specific tasks
- Quantify memory usage and inference speed
- Compare to larger general-purpose models (e.g., GPT-4) for baseline comparison
Research Reagent Solutions
| Reagent/Tool | Function | Application Context |
|---|---|---|
| Boolmore | Genetic algorithm-based model refinement | Automated optimization of Boolean models for biological networks [7] |
| QLoRA | Parameter-efficient fine-tuning | Adapting large models to specialized domains with limited resources [68] |
| GPTQ Quantization | GPU-optimized model compression | Efficient deployment on GPU infrastructure [68] |
| GGUF Quantization | CPU-optimized model compression | Efficient deployment on CPU-based systems [68] |
| Hyperparameter Optimization Tools (Optuna, Ray Tune) | Automated parameter tuning | Finding optimal model configurations [60] |
| Pruning Algorithms | Model complexity reduction | Removing unnecessary parameters while maintaining performance [60] |
| Quantitative Systems Pharmacology (QSP) Models | Mechanistic modeling of drug effects | Predicting drug behavior in biological systems [21] |
| PBPK Modeling | Physiologically-based pharmacokinetic prediction | Understanding drug absorption, distribution, metabolism, and excretion [21] |
Workflow Visualization
Fit-for-Purpose Model Optimization Workflow
Genetic Algorithm Model Refinement Process
Optimization Technique Selection Guide
Leveraging Expansion Cohorts and Novel Trial Designs for Richer Data Collection
→ Technical Support Center: Troubleshooting Guides and FAQs
Troubleshooting Common Issues in Expansion Cohort Trials
Q1: Our expansion cohort is failing to meet patient enrollment timelines. What are the primary causes and solutions?
Issue Analysis: Chronic under-enrollment is a key symptom of a non-optimized trial design. It often stems from overly narrow eligibility criteria, lack of patient awareness, or poor site selection [70].
Actionable Protocol:
- Utilize Real-World Data (RWD): Use RWD to refine inclusion/exclusion criteria and identify potential clinical trial sites with larger pools of eligible patients [70].
- Broaden Engagement: Partner with patient advocacy groups to raise awareness and build trust within patient communities [70].
- Optimize Site Selection: Conduct rigorous site feasibility assessments, prioritizing sites with proven records of patient recruitment and retention for specific oncology indications [70].
- Review Design: Model your trial's execution in a virtual environment during the design phase to predict and rectify enrollment bottlenecks before the trial begins [71].
Q2: We are encountering unexpected operational complexity and budget overruns in our DEEC trial. How can we improve financial planning?
Issue Analysis: Budget overruns are frequently caused by unanticipated recruitment costs, protocol amendments, and delays that extend the trial timeline [70].
Actionable Protocol:
- Conduct Robust Feasibility Studies: Perform detailed assessments before trial launch to identify potential cost overruns early and refine the budget [70].
- Leverage Predictive Budgeting: Use predictive analytics tools to forecast financial needs more accurately, accounting for patient recruitment and site monitoring costs [70].
- Centralize Design Functions: Establish a centralized trial design capability. A financial justification for this can be built by demonstrating that a 10% savings on the execution phase—through fewer site visits, reduced lab draws, or faster enrollment—will more than pay for the design center's costs [71].
Q3: How can we prevent bias in endpoint assessment in a single-arm trial using a DEEC design?
Issue Analysis: In single-arm trials without a control group, endpoint assessment, particularly for outcomes like tumor response, can be susceptible to bias [72].
Actionable Protocol:
- Implement Independent Review: Utilize an Independent Review Committee (IRC) for endpoint adjudication. This is a critical step to ensure blinded, unbiased assessment of efficacy endpoints [72].
- Define Endpoints Precisely: Use standardized and objectively defined efficacy endpoints in the protocol to minimize interpretation variability.
- Maintain Blinding: Ensure the IRC remains blinded to treatment details and other patient data that could influence their assessment.
Q4: Our trial's patient population does not match the expected commercial population. How can we improve diversity and representativeness?
Issue Analysis: A lack of diversity skews results and limits the generalizability of findings [70].
Actionable Protocol:
- Adopt Inclusive Criteria: Review and broaden inclusion criteria where medically appropriate to encompass a more diverse patient demographic [70].
- Utilize Community-Based Sites: Select trial sites in diverse community settings, not just academic centers, to better represent different populations [70].
- Implement Multilingual Outreach: Provide consent forms and trial information in multiple languages and engage with community leaders to build trust [70].
FAQs on Model Refinement and Trial Optimization
Q1: What is the fundamental difference between a traditional phase I trial and a Dose-Escalation and -Expansion Cohort (DEEC) trial?
- Traditional Phase I: Primarily focuses on safety and determining the maximum tolerated dose (MTD) in a small number of subjects (20-100), often healthy volunteers. It is typically a standalone study [73].
- DEEC Trial: Integrates dose-finding with preliminary efficacy assessment. The dose-escalation phase (using 3+3, Bayesian optimal interval, or continual reassessment methods) finds the recommended Phase II dose. The expansion cohort then directly enrolls additional patients at that dose to further characterize safety, pharmacokinetics, and antitumor activity, potentially serving as the pivotal trial for approval [72] [74].
Q2: What flexible designs can be used for expansion cohorts?
Expansion cohorts can adopt several innovative adaptive designs to efficiently answer multiple questions concurrently [72]:
- Basket Trials: Test the effect of a single drug on a single mutation across multiple cancer types.
- Umbrella Trials: Test multiple targeted drugs on different mutations within a single cancer type.
- Platform Trials: Allow for the flexible addition of new treatment arms or the removal of ineffective ones under a single master protocol.
Q3: How can we justify using a DEEC study as a pivotal trial for regulatory approval?
The use of DEEC studies as pivotal evidence for approval has gained traction, particularly in oncology. From 2012 to 2023, DEECs supported 46 FDA approvals for targeted anticancer drugs [72]. Justification relies on:
- Strong Preliminary Data: The dose-escalation phase must provide a clear and compelling safety and efficacy signal.
- Robust Expansion Data: The expansion cohort must be sufficiently large and well-controlled to provide definitive evidence of efficacy, often using an independent review committee to mitigate bias [72].
- Alignment with Regulatory Guidance: Follow FDA guidance on the use of expansion cohorts in first-in-human trials to expedite oncology drug development [74].
Q4: Our team is resistant to adopting new technologies like AI for trial design. How can we overcome this?
Resistance is common due to training gaps, cost concerns, and general fear of change [70].
- Demonstrate Value: Showcase long-term benefits, such as the ability of AI and RWD to predict enrollment timelines and optimize protocol design, reducing unpleasant surprises [71].
- Provide Vendor Training: Leverage training programs offered by technology vendors to upskill staff [70].
- Implement Gradually: Introduce new tools incrementally to ease the transition and allow for adjustment [70].
→ The Scientist's Toolkit: Essential Materials & Reagents
The table below details key components used in the design and execution of advanced trial designs like DEEC studies.
| Research Reagent / Solution | Function in Experiment |
|---|---|
| Bayesian Optimal Interval (BOIN) Design | A statistical method used in the dose-escalation phase to efficiently determine the Recommended Phase II Dose (RP2D) by calculating the probability of dose-limiting toxicities [72]. |
| Independent Review Committee (IRC) | A group of independent, blinded experts tasked with adjudicating primary efficacy endpoints (e.g., tumor response) to prevent assessment bias, especially in single-arm trials [72]. |
| Real-World Data (RWD) | Data relating to patient health status and/or the delivery of health care collected from routine clinical practice. Used to optimize protocol design, inform eligibility criteria, and identify potential trial sites [70] [71]. |
| Electronic Data Capture (EDC) System | A secure, centralized platform for automated collection and management of clinical trial data. Ensures data integrity, consistency across sites, and compliance with regulatory standards [70]. |
| Simon's Two-Stage Design | An adaptive statistical design often used within expansion cohorts. It allows for an interim analysis to determine if the treatment shows sufficient activity to continue enrollment, preserving resources [72]. |
→ Experimental Workflow & Data Presentation
Workflow Diagram: DEEC Trial Structure
The diagram below illustrates the integrated, multi-cohort structure of a Dose-Escalation and -Expansion Cohort trial.
Table 1: Comparison of Novel Clinical Trial Designs for Targeted Therapies
| Trial Design | Primary Objective | Key Feature | Consideration for Model Refinement |
|---|---|---|---|
| Dose-Escalation and -Expansion Cohort (DEEC) | To efficiently establish a recommended dose and gather pivotal efficacy data in a single trial [72]. | Integrated design where expansion cohorts begin once a safe dose is identified [72]. | Requires independent endpoint review to prevent bias in single-arm studies [72]. |
| Basket Trial | To test the effect of a single drug targeting a specific molecular alteration across multiple cancer types or diseases [72]. | Patient eligibility is based on molecular markers rather than tumor histology. | Allows for refinement of the target population based on response in different "baskets." |
| Umbrella Trial | To test multiple targeted drugs or combinations against different molecular targets within a single cancer type [72]. | Multiple sub-studies are conducted under one master protocol with a common infrastructure. | Efficient for comparing and refining multiple therapeutic strategies simultaneously. |
| Platform Trial | To evaluate multiple interventions in a perpetual setting, allowing arms to be added or dropped based on interim results [72]. | Adaptive and flexible; uses a common control arm and pre-specified decision rules. | Ideal for the continuous refinement of treatment protocols in a dynamic environment. |
Detailed Methodology: Implementing an Independent Review Committee (IRC)
Objective: To ensure unbiased, blinded adjudication of primary efficacy endpoints (e.g., Objective Response Rate) in a single-arm expansion cohort trial.
Protocol:
Charter Development: Draft a detailed IRC charter before the first patient's first scan. This document must define:
- The composition of the IRC (e.g., number of radiologists, oncologists).
- Blinding procedures (IRC members must be blinded to treatment, clinical data, and investigator assessments).
- Response criteria (e.g., RECIST 1.1) and detailed implementation guidelines.
- Procedures for handling discrepant assessments between reviewers.
Image and Data Transfer: Establish a secure, HIPAA-compliant process for transferring all radiographic images and the minimum necessary clinical data (e.g., baseline and on-treatment scans) to the IRC. All potential patient-identifying information must be removed.
Blinded Adjudication: IRC members independently review the images according to the pre-specified criteria in the charter. Their assessments are recorded directly into a dedicated, secure database.
Consensus Process: If independent reviews differ, a pre-defined consensus process is followed. This may involve a third reviewer or a consensus meeting to arrive at a final, binding assessment.
Data Integration: The finalized IRC assessments are integrated with the main clinical trial database for the final analysis. Both the IRC and investigator assessments are often reported in regulatory submissions.
Proving Your Model's Worth: Rigorous Validation and Comparative Analysis
Frequently Asked Questions (FAQs)
1. What is the fundamental difference between in-sample and out-of-sample validation?
Answer: In-sample validation assesses your model's "goodness of fit" using the same dataset it was trained on. It tells you how well the model reproduces the data it has already seen [75]. In contrast, out-of-sample validation tests the model's performance on new, unseen data (a hold-out set). This provides a realistic estimate of the model's predictive performance in real-world scenarios and its ability to generalize [76] [75].
2. Why is my model's in-sample accuracy high, but its out-of-sample performance is poor?
Answer: This is a classic sign of overfitting [77] [75]. Your model has likely become too complex and has learned not only the underlying patterns in the training data but also the noise and random fluctuations. Consequently, it is overly tailored to the training data and fails to generalize to new observations [75]. To mitigate this, you can simplify the model, use regularization techniques, or gather more training data [77].
3. When working with limited data, how can I reliably perform out-of-sample validation?
Answer: When your dataset is small, using a single train-test split might not be reliable due to the reduced sample size for training. In such cases, use resampling techniques like K-Fold Cross-Validation [77]. This method divides your data into K subsets (folds). The model is trained on K-1 folds and validated on the remaining fold. This process is repeated K times, with each fold serving as the validation set once. The final performance is the average across all K trials, providing a robust estimate of out-of-sample performance without severely reducing the training set size [77].
4. For a clinical prediction model, which evaluation metric should I prioritize?
Answer: For clinical applications, the choice of metric is critical and should be guided by the clinical consequence of different error types [78] [79].
- Prioritize Recall (Sensitivity) if missing a positive case (e.g., a patient with a disease) is costlier than a false alarm. This ensures you identify as many true cases as possible [78].
- Prioritize Precision if a false positive diagnosis is very costly (e.g., leading to unnecessary, invasive treatments) [78] [79].
- Often, the F1 Score (the harmonic mean of precision and recall) provides a single, balanced metric when both false positives and false negatives are important [78]. Never rely solely on accuracy, especially with imbalanced datasets, as it can be profoundly misleading (the "Accuracy Paradox") [78].
Troubleshooting Guides
Issue: Model is Overfitting to Training Data
Symptoms:
- High performance metrics (e.g., accuracy, R-squared) on the training data.
- Significantly lower performance on the validation or test data [77] [75].
Diagnostic Steps:
- Compare Metrics: Calculate and compare key performance metrics (e.g., accuracy, precision, recall, log loss) between your training and hold-out test sets. A large gap indicates overfitting.
- Visualize Fit: For regression models, plot the model's predictions against the actual values for both the training and test sets. An overfit model will perfectly follow the training data points but deviate significantly on the test set.
- Learning Curves: Plot learning curves to see if performance on the validation set improves with more training data or if the gap remains.
Solutions:
- Simplify the Model: Reduce model complexity by using fewer parameters, limiting tree depth (for decision trees), or reducing the number of layers/neurons (for neural networks) [77].
- Apply Regularization: Use techniques like L1 (Lasso) or L2 (Ridge) regularization that penalize overly complex models [77].
- Gather More Data: Increasing the size and diversity of your training dataset can help the model learn more generalizable patterns [77].
- Use Cross-Validation: Employ K-Fold cross-validation for hyperparameter tuning to ensure your model choices generalize well [77].
Issue: Model Performance is Poor on All Data (Underfitting)
Symptoms:
- Low performance metrics on both the training data and the validation/test data [77].
Diagnostic Steps:
- Check Baseline: Compare your model's performance to a simple baseline (e.g., predicting the mean or majority class). If your model cannot outperform the baseline, it is likely underfitting.
- Review Features: Evaluate whether your input features are informative and relevant to the problem.
Solutions:
- Increase Model Complexity: Use a more powerful model, add more layers to a neural network, or increase the depth of a decision tree.
- Feature Engineering: Create new, more predictive features from your existing data.
- Reduce Regularization: If you have applied strong regularization, try reducing its strength.
- Train for Longer: For iterative models like neural networks or gradient boosting, increase the number of training epochs or iterations.
Comparative Analysis: In-Sample vs. Out-of-Sample Validation
The table below summarizes the core differences, purposes, and appropriate use cases for each validation type.
| Aspect | In-Sample Validation | Out-of-Sample Validation |
|---|---|---|
| Core Purpose | Assess goodness of fit and model interpretation [75]. | Estimate predictive performance and generalizability [76] [75]. |
| Data Used | The same data used to train (fit) the model [80] [76]. | A separate, unseen hold-out dataset (test set) [80] [75]. |
| Primary Goal | Understand relationships between variables; check model assumptions [75]. | Simulate real-world performance on new data [76]. |
| Key Advantage | Computationally efficient; useful for interpreting model coefficients [75] [81]. | Helps detect overfitting; provides a realistic performance estimate [75] [81]. |
| Key Risk | High risk of overfitting; poor performance on new data [76] [81]. | Reduces sample size for training; can be computationally intensive [75] [81]. |
| Ideal Use Case | Exploratory data analysis, understanding variable relationships/drivers [75]. | Model selection, hyperparameter tuning, and final model evaluation before deployment [76]. |
Experimental Protocols for Robust Validation
Protocol 1: Hold-Out Validation for Model Evaluation
This is the foundational method for out-of-sample testing [77].
- Data Preparation: Preprocess your entire dataset (handle missing values, normalize features, etc.).
- Data Splitting: Randomly split your data into two mutually exclusive sets:
- Training Set (~70-80%): Used to train your model.
- Test (Hold-Out) Set (~20-30%): Locked away and not used during model training or tuning.
- Model Training: Train your model using only the training set.
- Final Evaluation: Use the trained model to make predictions on the hold-out test set. Calculate all performance metrics (e.g., accuracy, precision, recall) on this set. This is your best estimate of real-world performance.
Protocol 2: K-Fold Cross-Validation for Model Development
Use this protocol for reliable model selection and hyperparameter tuning, especially with smaller datasets [77].
- Data Preparation: Preprocess your data.
- Data Splitting: Split the data into K subsets (folds) of approximately equal size. Common values for K are 5 or 10.
- Iterative Training and Validation: For each unique fold
i(wherei= 1 to K):- Use fold
ias the validation set. - Use the remaining K-1 folds as the training set.
- Train the model and evaluate it on the validation set, storing the performance metric.
- Use fold
- Result Aggregation: Calculate the average and standard deviation of the K performance metrics. The average gives a robust estimate of out-of-sample performance.
The following workflow diagram illustrates the K-Fold Cross-Validation process:
The Scientist's Toolkit: Essential Materials for Model Validation
The table below lists key "research reagents" – computational tools and conceptual components – essential for rigorous model validation.
| Tool / Component | Function / Explanation |
|---|---|
| Training Set | The subset of data used to estimate the model's parameters. It is the sample on which the model "learns" [77] [81]. |
| Test (Hold-Out) Set | The reserved subset of data used to provide an unbiased evaluation of the final model fit on the training data. It must not be used during training [77]. |
| K-Fold Cross-Validation | A resampling procedure used to evaluate models on a limited data sample. It provides a more reliable estimate of out-of-sample performance than a single hold-out set [77]. |
| Confusion Matrix | A table that describes the performance of a classification model by breaking down predictions into True/False Positives/Negatives. It is the foundation for many other metrics [78] [79]. |
| ROC-AUC Curve | A plot that shows the trade-off between the True Positive Rate (Sensitivity) and False Positive Rate at various classification thresholds. The Area Under the Curve (AUC) summarizes the model's overall ability to discriminate between classes [78] [79]. |
| Precision & Recall | Metrics that are more informative than accuracy for imbalanced datasets. Precision focuses on the cost of false positives, while Recall focuses on the cost of false negatives [78]. |
| Scikit-learn | A core Python library that provides simple and efficient tools for data mining and analysis, including implementations for model validation, cross-validation, and performance metrics [77]. |
Frequently Asked Questions (FAQs)
Q1: Why is accuracy a misleading metric for my imbalanced drug screening data? Accuracy measures the overall correctness of a model but can be highly deceptive when your dataset is imbalanced, which is common in drug discovery where there are far more inactive compounds than active ones [82]. A model that simply predicts "inactive" for all compounds would achieve a high accuracy score yet would fail completely to identify any active candidates [83] [84]. In such scenarios, metrics like Precision and Recall provide a more meaningful performance assessment.
Q2: How do I choose between optimizing for Precision or Recall? The choice depends on the cost of different types of errors in your specific experiment [84].
- Optimize for Precision when false positives are costly. For example, in the early stages of virtual screening, high Precision ensures that the compounds flagged as "active" are very likely to be true hits, preventing wasted resources on validating incorrect leads [83] [82].
- Optimize for Recall when false negatives are costly. In safety-critical applications, such as predicting drug toxicity or adverse reactions, a false negative (missing a toxic compound) is much riskier than a false positive. High Recall ensures you capture as many true risky compounds as possible [84] [82].
Q3: What does the F1-Score represent, and when should I use it? The F1-Score is the harmonic mean of Precision and Recall [83] [84]. It provides a single metric that balances the trade-off between the two [85]. Use the F1-Score when you need a balanced measure and there is no clear preference for prioritizing Precision over Recall or vice versa. It is especially useful for comparing models on imbalanced datasets where accuracy is not informative [83] [86].
Q4: My model's Precision calculation returned "NaN." What does this mean? A "NaN" (Not a Number) result for Precision occurs when the denominator in the Precision formula is zero, meaning your model did not make any positive predictions (i.e., it predicted zero true positives and zero false positives) [84]. This can happen with a model that never predicts the positive class. While it could theoretically indicate perfect performance in a scenario with no positives, it more often suggests a model that is not functioning as intended for the task.
Q5: Are there domain-specific metrics beyond Precision and Recall for drug discovery? Yes, standard metrics can be limited for complex biopharma data. Domain-specific metrics are often more appropriate [82]:
- Precision-at-K: Measures the model's precision when considering only the top K highest-ranked predictions. This is ideal for prioritizing the most promising drug candidates from a large library [82].
- Rare Event Sensitivity: Focuses specifically on the model's ability to correctly identify low-frequency but critical events, such as rare adverse drug reactions or specific genetic mutations [82].
- Enrichment Factor: A common metric in virtual screening that measures how much a model enriches known active compounds at a given cutoff compared to a random selection [87].
Troubleshooting Guides
Problem: Model has high accuracy but fails to identify any promising drug candidates. This is a classic symptom of evaluating a model with an inappropriate metric on an imbalanced dataset.
Diagnosis:
- Verify the class distribution in your dataset. In drug discovery, inactive compounds typically vastly outnumber active ones [82].
- Check the Confusion Matrix. You will likely see a high number of True Negatives (correctly identified inactives) but very few or zero True Positives (correctly identified actives) [88] [85].
Solution:
- Shift your evaluation metrics. Stop using accuracy as your primary metric.
- Focus on Recall and Precision. Examine the confusion matrix and calculate Precision, Recall, and F1-score [83] [86].
- Consider domain-specific metrics. Use metrics like Precision-at-K to evaluate the model's performance on the top-ranked predictions that matter most for your screening pipeline [82].
Problem: Struggling with the trade-off between Precision and Recall. It is often challenging to improve one without harming the other. This is a fundamental trade-off in machine learning [84].
Diagnosis:
- As you adjust your model's classification threshold, you will observe an inverse relationship between Precision and Recall [84]. A higher threshold typically increases Precision but decreases Recall, and vice versa.
Solution:
- Use the F1-Score. This metric helps you find a model that offers a good balance between Precision and Recall [83] [85].
- Plot a Precision-Recall curve. This visualization allows you to see the trade-off across all possible thresholds and select an optimal operating point for your specific needs.
- Align the trade-off with project goals. Make a strategic decision based on the stage of your research [82]:
- Early-stage screening: Favor Recall to ensure no potential active compound is missed.
- Lead optimization: Favor Precision to ensure resources are dedicated to validating the most promising, high-confidence candidates.
Problem: Need to evaluate a multi-class classification model for tasks like predicting multiple binding affinities. Standard metrics are designed for binary classification (active/inactive) and must be adapted for multiple classes.
Diagnosis: Your model predicts more than two classes or outcomes.
Solution:
- Calculate Precision, Recall, and F1-score for each class individually, treating each one as the "positive" class in turn [83].
- Aggregate the per-class metrics to get an overall score using one of two main methods [83]:
- Macro-average: Computes the metric independently for each class and then takes the average. This treats all classes equally, regardless of their size.
- Weighted-average: Computes the average, weighted by the number of true instances for each class. This is preferable for imbalanced datasets as it accounts for class support.
Metric Selection Workflow
The following diagram outlines a logical workflow to guide researchers in selecting the most appropriate evaluation metric based on their project's goals and data characteristics.
The table below provides a concise definition, formula, and ideal use case for each core metric.
| Metric | Definition | Formula | Ideal Use Case |
|---|---|---|---|
| Accuracy | Overall proportion of correct predictions. | (TP + TN) / (TP + TN + FP + FN) [84] | Balanced datasets; initial, coarse-grained model assessment [84]. |
| Precision | Proportion of positive predictions that are actually correct. | TP / (TP + FP) [83] [84] | When the cost of false positives is high (e.g., virtual screening to avoid wasted resources) [83] [82]. |
| Recall | Proportion of actual positives that were correctly identified. | TP / (TP + FN) [83] [84] | When the cost of false negatives is high (e.g., toxicity prediction where missing a signal is critical) [84] [82]. |
| F1-Score | Harmonic mean of Precision and Recall. | 2 * (Precision * Recall) / (Precision + Recall) [84] | Imbalanced datasets; when a single balanced metric is needed [83] [85]. |
Experimental Protocol: Calculating Metrics with Scikit-learn
This protocol provides a step-by-step methodology for implementing the calculation of these metrics in Python, a common tool in computational research.
1. Objective: To quantitatively evaluate the performance of a binary classification model using accuracy, precision, recall, and F1-score via the scikit-learn library.
2. Research Reagent Solutions (Key Materials/Software)
| Item | Function in Experiment |
|---|---|
| Python (v3.8+) | Programming language providing the computational environment. |
| Scikit-learn library | Provides the functions for metrics calculation and model training [83] [86]. |
| NumPy library | Supports efficient numerical computations and array handling. |
| Synthetic or labeled dataset | Provides the ground truth and feature data for model training and evaluation. |
3. Methodology:
- Step 1: Import Libraries. Import all necessary Python modules.
- Step 2: Prepare Data. Load or generate a dataset and split it into training and testing sets. The example below creates a synthetic dataset for a binary classification problem.
- Step 3: Train a Model. Train a classifier, such as Logistic Regression.
- Step 4: Generate Predictions. Use the trained model to make predictions on the test set.
- Step 5: Calculate and Interpret Metrics. Compute the key evaluation metrics and analyze the results.
Cross-validation (CV) is a fundamental statistical procedure used to evaluate the performance and generalization ability of machine learning models by resampling the available data [89] [90]. For researchers focusing on optimizing model refinement for low-accuracy targets—such as in bioactivity prediction or protein structure refinement—selecting the appropriate cross-validation strategy is critical to obtaining reliable performance estimates that reflect real-world applicability [91] [92]. This technical guide addresses the key challenges and solutions for implementing robust validation frameworks within computational research environments.
The core challenge in model refinement lies in the sampling problem: effectively exploring the conformational or chemical space to reach more accurate states without overfitting to the initial training data [38] [92]. Cross-validation provides a framework to estimate how well refined models will perform on truly unseen data, which is especially important when working with limited experimental data or when extrapolating beyond known chemical spaces [91].
Cross-Validation Methodologies: Technical Specifications
Core Validation Techniques
Table 1: Fundamental Cross-Validation Techniques for Model Refinement
| Technique | Mechanism | Best Use Cases | Advantages | Limitations |
|---|---|---|---|---|
| Hold-Out Validation | Single split into training and test sets (commonly 70-30% or 80-20%) [90] | Initial model prototyping, very large datasets [90] | Computationally efficient, simple to implement [90] | High variance in performance estimates, inefficient data usage [90] |
| K-Fold Cross-Validation | Data divided into k folds; each fold serves as validation once while k-1 folds train the model [93] [94] | General-purpose model selection, hyperparameter tuning with limited data [93] | Reduces variance compared to hold-out, uses all data for evaluation [93] | Computational cost increases with k, standard k-fold may not suit specialized data structures [93] |
| Stratified K-Fold | Preserves class distribution percentages across all folds [95] | Classification with imbalanced datasets | Prevents skewed performance from uneven class representation | Does not account for group structures or temporal dependencies [95] |
| Leave-One-Out (LOOCV) | Leave one sample out for validation, use remaining n-1 samples for training; repeated for all samples [93] [89] | Very small datasets where maximizing training data is critical [90] | Maximizes training data, low bias | Computationally expensive, high variance in error estimates [93] [90] |
| Leave-P-Out | Leaves p samples out for validation [93] [89] | Small to medium datasets requiring robust evaluation | More comprehensive than LOOCV with proper p selection | Computationally intensive with overlapping validation sets [93] |
Domain-Specific and Advanced Techniques
Table 2: Specialized Cross-Validation Methods for Research Applications
| Technique | Domain Application | Splitting Strategy | Research Context |
|---|---|---|---|
| Stratified Group K-Fold [95] | Biomedical data with repeated measurements or multiple samples per patient | Maintains group integrity while preserving class distribution | Prevents information leakage between samples from the same subject or experimental batch |
| Time Series Split [96] | Temporal data, longitudinal studies | Chronological ordering with expanding training window | Maintains temporal causality, prevents future information leakage in forecasting models |
| k-fold n-step Forward (SFCV) [91] | Drug discovery, bioactivity prediction | Sorted by molecular properties (e.g., logP) with sequential training-testing blocks | Mimics real-world scenario of optimizing compounds toward more drug-like properties [91] |
| Nested Cross-Validation [96] | Hyperparameter tuning with unbiased performance estimation | Inner loop for parameter optimization, outer loop for performance assessment | Preforms model selection and evaluation without optimistically biasing performance metrics [96] |
Nested Cross-Validation Workflow for Robust Model Selection
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools for Cross-Validation in Research
| Tool/Category | Function | Implementation Examples |
|---|---|---|
| Model Accuracy Estimation | Predicts local and global model quality to guide refinement | DeepAccNet (protein refinement) [92], ProQ3D, VoroMQA [92] |
| Molecular Featurization | Represents chemical structures as machine-readable features | ECFP4 fingerprints, Morgan fingerprints [91] |
| Structured Data Splitting | Creates domain-appropriate train/test splits | Scaffold splitting (by molecular core) [91], time-series splitting [96] |
| Performance Metrics | Quantifies model improvement after refinement | Discovery yield, novelty error [91], Cβ l-DDT (protein) [92], GDT-TS [92] |
Troubleshooting Guide: Common Cross-Validation Issues
Data Leakage and Preprocessing Problems
Issue: Data leakage during preprocessing causing over-optimistic performance
- Problem Identification: Model performs well during validation but fails in production; performance metrics don't match real-world applicability [93] [95].
- Root Cause: Applying preprocessing steps (e.g., normalization, feature selection) to the entire dataset before splitting, allowing information from the test set to influence training [93] [95].
- Solution:
- Implement a preprocessing pipeline within each cross-validation fold
- Fit preprocessing parameters (e.g., normalization coefficients) on training folds only
- Apply the trained preprocessing to validation folds without refitting
- Use
Pipelineobjects in scikit-learn to automate this process [96]
Issue: Inadequate separation of grouped data
- Problem Identification: Overly optimistic performance when samples within groups are correlated (e.g., multiple measurements from same patient, compounds with similar scaffolds) [95].
- Root Cause: Random splitting without considering group structure places correlated samples in both training and test sets.
- Solution: Implement group-based cross-validation where all samples from a group appear exclusively in either training or test sets [95].
Specialized Data Challenges
Issue: Poor performance on time-series or temporally structured data
- Problem Identification: Models fail to maintain performance when deployed for forecasting.
- Root Cause: Standard random splitting violates temporal dependencies, allowing models to "cheat" by learning from future patterns [96].
- Solution:
Issue: Models fail to generalize to novel chemical spaces in drug discovery
- Problem Identification: Excellent performance on validation compounds but poor prediction for truly novel scaffolds [91].
- Root Cause: Random splitting creates test sets with compounds similar to training data, not reflecting real-world discovery scenarios.
- Solution: Implement step-forward cross-validation sorted by molecular properties (e.g., logP) where training contains less drug-like compounds and testing evaluates more drug-like compounds [91].
Implementation and Computational Challenges
Issue: High variance in model performance estimates
- Problem Identification: Significant performance fluctuations with different random seeds or data splits [90].
- Root Cause: Insufficient model averaging combined with small dataset size amplifies variance.
- Solution:
- Use repeated k-fold cross-validation with multiple random splits
- Increase k value where computationally feasible
- Report performance as mean ± standard deviation across folds
- Consider ensemble methods to reduce variance [95]
Issue: Computational bottlenecks with complex refinement protocols
- Problem Identification: Cross-validation becomes computationally prohibitive with resource-intensive refinement methods (e.g., molecular dynamics, deep learning) [38] [92].
- Root Cause: Multiple refinement iterations across many folds multiplies computational requirements.
- Solution:
- Implement strategic down-sampling for initial experiments
- Use parallel computing to process folds simultaneously
- Employ approximate methods for initial hyperparameter screening
- Consider transfer learning from related tasks to reduce needed folds [92]
Frequently Asked Questions (FAQs)
Q1: How do I choose between k-fold cross-validation and a separate hold-out test set? A: These serve complementary purposes. Use k-fold cross-validation for model selection and hyperparameter tuning within your training data. Always maintain a completely separate hold-out test set for final model evaluation after all tuning is complete. This approach provides the most reliable estimate of real-world performance [93] [96].
Q2: What is the optimal value of k for k-fold cross-validation in protein refinement or bioactivity prediction? A: For typical datasets in computational biology (hundreds to thousands of samples), k=5 or k=10 provide reasonable bias-variance tradeoffs. With very small datasets (<100 samples), consider Leave-One-Out Cross-Validation despite computational cost. For larger datasets, k=5 is often sufficient. The choice should also consider computational constraints of refinement protocols [93] [90].
Q3: How can I validate that my refinement protocol actually improves model accuracy rather than just overfitting? A: Implement novelty error and discovery yield metrics alongside standard performance measures. For protein refinement, assess whether refined models show improved accuracy on regions initially predicted with low confidence. Most importantly, maintain a strict temporal or scaffold-based split where the test set represents truly novel instances not available during training [91].
Q4: What specific cross-validation strategies work best for low-accuracy starting models? A: With low-accuracy starting points (e.g., protein models with GDT-TS <50), consider:
- Increasing k-fold repetitions to account for higher variance
- Implementing ensemble approaches across multiple validation folds
- Using stratified splitting based on model error distributions
- Incorporating accuracy predictions (e.g., DeepAccNet) to guide both refinement and validation prioritization [92]
Q5: How do I handle cross-validation when my dataset has significant class imbalance? A: Use stratified k-fold cross-validation to maintain class proportions in each fold. For severe imbalance (e.g., 95:5 ratio), consider additional techniques such as:
- Oversampling the minority class (but only within training folds to avoid leakage)
- Using precision-recall curves instead of ROC curves for evaluation
- Employing appropriate metrics (F1-score, Matthews correlation coefficient) that account for imbalance [95]
Frequently Asked Questions
What are the primary causes of low accuracy in AI-driven target discovery models? Low accuracy often stems from weak target selection in the initial phases of research, which can account for a high percentage of subsequent failures [97]. This is frequently compounded by poor data quality, irrelevant features, suboptimal model selection for the specific problem, and inadequate hyperparameter tuning [49].
How can I systematically benchmark my target identification model against a gold standard? A robust benchmarking framework like TargetBench 1.0 provides a standardized system for this purpose [97]. You should evaluate your model's performance using metrics like clinical target retrieval rate and the translational potential of novel targets, which includes metrics on structure availability, druggability, and repurposing potential [97].
My model performs well on training data but poorly on validation data. What should I do? This is a classic sign of overfitting [49]. You should implement regularization techniques like L1 or L2 regularization, use dropout in neural networks, or employ ensemble methods like Random Forest which are naturally resistant to overfitting [60] [49]. Additionally, ensure you are using cross-validation for a more reliable performance estimate [49].
What optimization techniques can I use to improve a model's accuracy? Key techniques include hyperparameter optimization through methods like grid search, random search, or more efficient Bayesian optimization [60] [49]. Fine-tuning a pre-trained model on your specific dataset can also save significant resources [60]. For deep learning models, quantization and pruning can enhance efficiency without substantial performance loss [60].
Why is my model not generalizing well despite high computational investment? The issue may be that you are using a general-purpose model. Research indicates that creating disease-specific models, which learn context-dependent patterns unique to each disease area, can result in significantly higher accuracy compared to other models [97].
Troubleshooting Guides
Problem: Model Fails to Retrieve Clinically Relevant Targets
This issue occurs when your model's predictions do not align with known clinical targets or show low potential for translation.
| Troubleshooting Step | Action & Rationale | Key Metrics to Check |
|---|---|---|
| 1. Assess Data Quality & Integration | Integrate multi-modal data (genomics, transcriptomics, proteomics, clinical trial data) [97]. Audit for missing values and inconsistencies that create noise [49]. | Data completeness; Data source diversity. |
| 2. Evaluate Feature Relevance | Use feature selection techniques (e.g., Recursive Feature Elimination) to remove irrelevant or redundant features that confuse the model [49]. | Feature importance scores; Correlation analysis. |
| 3. Benchmark Against Standard | Use TargetBench 1.0 or a similar framework to compare your model's clinical target retrieval rate against established benchmarks (e.g., known LLMs achieving 15-40%) [97]. | Clinical target retrieval rate (aim for >70%). |
| 4. Verify Disease Specificity | Ensure your model is tailored to the specific disease context. A model's decision-making should be nuanced and rely on disease-specific biological patterns [97]. | Model explainability (e.g., SHAP analysis). |
Problem: Novel Targets Lack Translational Potential
Your model nominates novel targets, but they have low druggability, unclear structure, or poor repurposing potential.
| Troubleshooting Step | Action & Rationale | Key Metrics to Check |
|---|---|---|
| 1. Analyze Druggability | Check if predicted novel targets are classified as druggable. A high-performing system should achieve >85% in this metric [97]. | Druggability score (>86%). |
| 2. Check Structure Availability | Confirm that the 3D protein structure is resolved, which is critical for downstream drug design. Target for >95% structure availability [97]. | Structure availability rate (>95%). |
| 3. Assess Repurposing Potential | Evaluate the overlap of novel targets with approved drugs for other diseases. This can significantly de-risk development [97]. | Repurposing potential (>45%). |
| 4. Validate Experimental Readiness | Ensure nominated targets have associated bioassay data and available modulators for laboratory testing [97]. | Number of associated bioassays; Available modulators. |
Benchmarking Data & Performance Standards
The following table summarizes quantitative benchmarking data for AI-driven target identification platforms, providing a standard for comparison.
Table 1. Performance comparison of target identification systems, based on data from Insilico Medicine's landmark paper [97].
| Model / Platform | Clinical Target Retrieval Rate | Novel Target Structure Availability | Novel Target Druggability | Repurposing Potential |
|---|---|---|---|---|
| TargetPro | 71.6% | 95.7% | 86.5% | 46% |
| GPT-4o | 15-40% | 60-91% | 39-70% | Significantly lower |
| Grok3 | 15-40% | 60-91% | 39-70% | Significantly lower |
| DeepSeek-R1 | 15-40% | 60-91% | 39-70% | Significantly lower |
| Open Targets | <20% | 60-91% | 39-70% | Significantly lower |
Experimental Protocols
Protocol 1: Establishing a Benchmarking Framework for Target Identification
This protocol outlines the creation of a standardized benchmarking system like TargetBench 1.0 [97].
- Objective: To create a reproducible system for evaluating and comparing the performance of different target identification models.
- Materials:
- Gold Standard Target Set: A curated list of known clinical-stage targets across multiple disease areas.
- Multi-modal Data: Integrated data from 22 sources, including genomics, transcriptomics, proteomics, and clinical trial records.
- Evaluation Metrics: Defined metrics such as Clinical Target Retrieval Rate, Structure Availability, Druggability, and Repurposing Potential.
- Procedure:
- Compile Gold Standards: Aggregate a comprehensive set of clinically validated targets for oncology, neurological, immune, fibrotic, and metabolic disorders.
- Integrate Data Sources: Build a unified data infrastructure that harmonizes the 22 different multi-modal data types.
- Define Benchmarking Metrics: Establish clear, quantitative metrics for evaluation (see Table 1).
- Execute Model Comparisons: Run the models (e.g., LLMs, specialized AI) against the benchmark and calculate all performance metrics.
- Generate Performance Report: Document the results, highlighting strengths and weaknesses of each model.
Protocol 2: Systematic Hyperparameter Optimization for Model Refinement
This protocol details a method for fine-tuning models to improve accuracy, based on established AI optimization techniques [60] [49].
- Objective: To systematically identify the optimal hyperparameters for a machine learning model to maximize its performance on a given task.
- Materials:
- A trained machine learning model.
- A validation dataset.
- Computational resources (e.g., high-performance computing cluster).
- Optimization tools (e.g., Optuna, Scikit-learn's GridSearchCV).
- Procedure:
- Define Search Space: Identify the hyperparameters to tune (e.g., learning rate, number of layers, batch size) and their potential value ranges.
- Select Optimization Method:
- Grid Search: Exhaustively searches over a specified parameter grid. Best for a small number of parameters.
- Random Search: Randomly samples from the parameter space. More efficient for higher dimensions.
- Bayesian Optimization: Uses a probabilistic model to guide the search towards promising parameters. The most efficient method for complex, resource-intensive models [60].
- Configure Cross-Validation: Set up k-fold cross-validation (e.g., k=5 or k=10) to ensure the model's performance is robust and not dependent on a single data split [49].
- Run Optimization: Execute the chosen optimization algorithm, which will train and evaluate the model multiple times with different hyperparameters.
- Identify Best Configuration: Select the hyperparameter set that yielded the highest performance on the validation metric.
Workflow Visualization
Benchmarking and Optimization Workflow
Target Identification and Validation Process
The Scientist's Toolkit: Research Reagent Solutions
Table 2. Essential tools and resources for AI-driven target discovery and model refinement.
| Tool / Resource | Function & Application |
|---|---|
| TargetBench 1.0 | A standardized benchmarking framework for evaluating target identification models against gold standards, ensuring reliability and transparency [97]. |
| Multi-Modal Data Integrator | A system that combines 22 different data types (genomics, proteomics, clinical data) to train robust, disease-specific target identification models [97]. |
| Hyperparameter Optimization Suites (e.g., Optuna) | Software tools that automate the search for optimal model parameters, dramatically improving performance through methods like Bayesian optimization [60] [49]. |
| Explainable AI (XAI) Libraries (e.g., SHAP) | Tools that help interpret model decisions, revealing disease-specific feature importance patterns and building trust in AI predictions [97]. |
| Model Pruning & Quantization Tools | Techniques for making deep learning models faster and smaller without significant performance loss, enhancing their practical deployment [60]. |
This technical support center provides troubleshooting and methodological guidance for researchers implementing the Genome Variant Refinement Pipeline (GVRP), a decision tree-based model designed to improve variant calling accuracy. The GVRP was developed to address a critical challenge in genomic studies, particularly for non-human primates: the significant performance degradation of state-of-the-art variant callers like DeepVariant under suboptimal sequence alignment conditions where alignment postprocessing is limited [98]. The following sections offer a detailed guide to deploying this refinement model, which achieved a 76.20% reduction in the miscalling ratio (MR) in rhesus macaque genomes, helping scientists optimize their workflows for low-accuracy targets [98].
Troubleshooting Guides
Guide 1: Addressing Low Yield or Quality in Input Sequence Data
User Problem: "My final sequencing library yield is unexpectedly low, or the data quality is poor, which I suspect is affecting my variant calling accuracy."
Background: The principle of "Garbage In, Garbage Out" is paramount in bioinformatics. Poor input data quality will compromise all downstream analyses, including variant refinement [33]. Low yield or quality often stems from issues during the initial library preparation steps [99].
Diagnosis and Solutions:
| Problem Area | Symptoms | Possible Root Cause | Corrective Action |
|---|---|---|---|
| Sample Input / Quality | Low yield; smear in electropherogram; low library complexity [99]. | Degraded DNA/RNA; sample contaminants (e.g., phenol, salts); inaccurate quantification [99]. | Re-purify input sample; use fluorometric quantification (e.g., Qubit) instead of just absorbance; ensure proper sample storage at -80°C [99] [100]. |
| Fragmentation & Ligation | Unexpected fragment size; sharp ~70-90 bp peak indicating adapter dimers [99]. | Over- or under-shearing; improper adapter-to-insert molar ratio; poor ligase performance [99]. | Optimize fragmentation parameters; titrate adapter concentration; ensure fresh ligase and optimal reaction conditions [99]. |
| Amplification / PCR | Overamplification artifacts; high duplicate rate; bias [99]. | Too many PCR cycles; enzyme inhibitors; mispriming [99]. | Reduce the number of PCR cycles; ensure complete removal of contaminants; optimize annealing conditions [99]. |
| Purification & Cleanup | Sample loss; carryover of salts or adapter dimers [99]. | Incorrect bead-to-sample ratio; over-drying beads; pipetting error [99]. | Precisely follow cleanup protocol for bead ratios and washing; avoid letting beads become completely dry [99]. |
Guide 2: Troubleshooting Suboptimal Performance of the Refinement Model
User Problem: "I have run the GVRP, but I am not observing a significant improvement in my variant call set, or the results seem unreliable."
Background: The refinement model uses a Light Gradient Boosting Model (LGBM) to filter false positive variants by integrating DeepVariant confidence scores with key alignment quality metrics [98]. Performance issues typically arise from problems with the input data fed into the model or misunderstandings of the model's scope.
Diagnosis and Solutions:
| Problem Symptom | Investigation Questions | Solutions |
|---|---|---|
| No reduction in miscalls | Did you start with suboptimal alignments? The model is designed to refine calls from data where indel realignment and base quality recalibration were not performed [98]. | Re-run your sequence alignment pipeline, deliberately omitting indel realignment and base quality recalibration steps to create the suboptimal SA condition the model requires [98]. |
| High false negative rate | What are your threshold settings? Are you filtering out true positives? | The model may refine homozygous SNVs more effectively than heterozygous SNVs. Analyze the Alternative Base Ratio (ABR) for different variant types. Adjust the model's decision threshold, balancing sensitivity and precision [98]. |
| Inconsistent results between samples | Is there high variability in alignment quality metrics (e.g., read depth, soft-clipping ratio) between your samples? | Ensure consistent sequencing depth and quality across all samples. Check that alignment metrics fall within expected ranges before applying the refinement model. The model relies on consistent feature distributions [98]. |
| Feature extraction errors | Were all required features (DeepVariant score, read depth, soft-clipping ratio, low mapping quality read ratio) correctly extracted? | Validate the output of the feature extraction script. Ensure the BAM and VCF files are correctly formatted and that no errors were reported during this pre-processing step [98]. |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between the DeepVariant caller and the GVRP refinement model?
A1: DeepVariant is a deep learning-based variant caller that identifies genomic variants from sequence alignments by converting data into image-like tensors [98]. The GVRP refinement model is a subsequent, decision tree-based filter that takes the output from DeepVariant (and other alignment metrics) and re-classifies variants to remove false positives, specifically those induced by suboptimal alignments [98].
Q2: Our lab primarily studies human genomes. Can this refinement model still be beneficial?
A2: Yes. The original study demonstrated the model's effectiveness on human data, where it achieved a 52.54% reduction in the miscalling ratio under suboptimal alignment conditions [98]. It is directly applicable to human genomic studies.
Q3: What defines "suboptimal" versus "optimal" sequence alignment for this pipeline?
A3: The key distinction lies in two postprocessing steps [98]:
- Optimal SA: An alignment where all postprocessing steps—including sorting, duplicate marking, indel realignment, and base quality recalibration—have been applied.
- Suboptimal SA: An alignment where indel realignment and base quality recalibration are omitted or performed under limited conditions. This is the intended input for the GVRP.
Q4: I am seeing high levels of noise in my data even before variant calling. What are some common sources of contamination?
A4: Common sources include [33]:
- Cross-sample contamination: Material from one sample leaks into another.
- External contamination: From bacteria, fungi, or human handling during processing.
- Adapter contamination: From library preparation, visible as sharp peaks in the 70-90 bp range on an electropherogram [99].
- Best Practice: Always process negative controls alongside your experimental samples to identify contamination sources.
Q5: Where can I find the GVRP software and its detailed protocol?
A5: The Genome Variant Refinement Pipeline (GVRP) is publicly available under an open-source license at: https://github.com/Jeong-Hoon-Choi/GVRP [98].
Experimental Protocols & Data
Core Methodology: Implementing the Refinement Model
The following workflow outlines the key experimental and computational steps for applying the genomic refinement model as described in the case study.
Quantitative Performance Data
The refinement model's performance was quantitatively assessed by the reduction in the Miscalling Ratio (MR). The results below summarize the key findings from the original research [98].
Table 1: Quantified Miscall Reduction of the Refinement Model
| Test Genome | Alignment Condition | Miscalling Ratio (MR) Reduction | Key Implication |
|---|---|---|---|
| Human | Suboptimal SA | 52.54% | Model is effective in the context it was designed for. |
| Rhesus Macaque | Suboptimal SA | 76.20% | Model is highly beneficial for non-human primate studies with limited curated resources. |
| Additional Finding | Variant Type Refined | Homozygous SNVs > Heterozygous SNVs | Model's refinement power varies by variant type, important for interpreting results [98]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for the GVRP Workflow
| Item | Function / Role in the Workflow | Example / Note |
|---|---|---|
| BWA (Burrows-Wheeler Aligner) | Aligns sequencing reads to a reference genome; the foundational step for all downstream analysis [98]. | Used in the initial sequence alignment step. |
| SAMtools, Picard, GATK | Tools for postprocessing alignments: sorting, duplicate marking, and (if needed) indel realignment and base quality recalibration [98]. | GATK 3.5.0 was used for Indel realignment and base quality recalibration in the study [98]. |
| DeepVariant | A state-of-the-art variant caller that identifies SNVs and Indels from processed alignment files; provides the initial variant calls and confidence scores for refinement [98]. | Transforms alignment data into images for a convolutional neural network (CNN) [98]. |
| Light Gradient Boosting Model (LGBM) | The decision tree-based ensemble learning algorithm that powers the refinement model, filtering false positives from the initial variant calls [98]. | The core of the GVRP, integrating DeepVariant scores with alignment metrics. |
| Monarch Spin gDNA Extraction Kit | For purifying high-quality genomic DNA from cells or tissues, which is critical for robust sequencing results [100]. | Ensure proper tissue homogenization and avoid overloading the column [100]. |
Conclusion
Optimizing the refinement of low-accuracy models is no longer a manual, artisanal process but an engineered, data-driven discipline. The integration of automated workflows like boolmore, machine learning refiners, and rigorous 'fit-for-purpose' validation frameworks provides a powerful toolkit for transforming unreliable initial targets into robust, predictive assets. As demonstrated by initiatives like the FDA's Project Optimus, these approaches are critical for making confident decisions in drug dosage selection, target validation, and beyond. The future of model refinement lies in the continued convergence of AI-driven automation, high-quality mechanistic data, and cross-disciplinary collaboration, ultimately leading to more efficient development cycles and safer, more effective therapies for patients.
References
- 1. Why 90% of clinical drug development fails and how to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9293739/]
- 2. Reproducibility in systems biology modelling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7901289/]
- 3. Target Engagement: A Key Factor in Drug Development ... [https://www.pelagobio.com/cetsa-drug-discovery-resources/blog/target-engagement-drug-failure/]
- 4. Genetic factors associated with reasons for clinical trial ... [https://www.nature.com/articles/s41588-024-01854-z]
- 5. Target identification and mechanism of action in chemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5543995/]
- 6. Systems biology-guided identification of synthetic lethal ... [https://www.nature.com/articles/srep16025]
- 7. Automated model refinement using perturbation- ... [https://www.nature.com/articles/s41540-025-00532-y]
- 8. 5 Strategies to Improve Workflow Efficiency in Drug Discovery [https://genemod.net/blog/5-strategies-to-improve-workflow-efficiency-in-drug-discovery]
- 9. SIGMOD 2025 Tutorial: Navigating Data Errors in Machine ... [https://navigating-data-errors.github.io/]
- 10. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 11. Ultraprocessed food (UPF), health, and mechanistic uncertainty [https://pmc.ncbi.nlm.nih.gov/articles/PMC11479387/]
- 12. Assessing uncertainty in mechanistic models [https://research.fs.usda.gov/treesearch/15898]
- 13. Teaching troubleshooting skills to graduate students - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11407763/]
- 14. Planning an experiment - Working scientifically [https://www.bbc.co.uk/bitesize/articles/zxn896f]
- 15. Deep active optimization for complex systems [https://www.nature.com/articles/s43588-025-00858-x]
- 16. Current Issues in Dose Finding Designs: A Response to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11132935/]
- 17. Key Considerations for Improving Dosage Optimization in ... [https://www.aacr.org/blog/2025/10/03/key-considerations-for-improving-dosage-optimization-in-oncology/]
- 18. FDA-AACR Strategies for Optimizing Dosages for Oncology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12536354/]
- 19. Adaptive phase 2/3 design with dose optimization [https://www.sciencedirect.com/science/article/abs/pii/S1551714425002423]
- 20. Drug Development Tools: Fit-for-Purpose Initiative [https://www.fda.gov/drugs/development-approval-process-drugs/drug-development-tools-fit-purpose-initiative]
- 21. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 22. How to be a Better Troubleshooter in Your Laboratory [https://www.goldbio.com/blogs/articles/how-to-be-a-better-troubleshooter?srsltid=AfmBOootBuSttP3SoYfreLaX1xFMryzehG4JUU3lojx_R3WDwWvvxZVP]
- 23. Long-distance target localization optimization algorithm ... [https://pubmed.ncbi.nlm.nih.gov/40646009/]
- 24. Long-distance target localization optimization algorithm ... [https://www.nature.com/articles/s41598-025-09428-7]
- 25. Accuracy and real time optimization of remote sensing image ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0329447]
- 26. Automated model refinement using perturbation-observation pairs [https://pure.psu.edu/en/publications/automated-model-refinement-using-perturbation-observation-pairs]
- 27. Reproducible Boolean model analyses and simulations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371346/]
- 28. AutoGrow4: an open-source genetic algorithm for de novo ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-020-00429-4]
- 29. Troubleshooting the gene-variant workflow [https://re-docs.genomicsengland.co.uk/gv_faqs/]
- 30. Major Causes of Conflicting Interpretations of Variant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11355203/]
- 31. Discrepancies in Variant Classifications and How to ... [https://www.genomenon.com/blog/discrepancies-variant-classifications-resolve]
- 32. The machine learning algorithm based on decision tree ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0317414]
- 33. Garbage In, Garbage Out: Dealing with Data Errors ... [https://blog.omni-inc.com/blog/garbage-in-garbage-out-dealing-with-data-errors-bioinformatics]
- 34. Exploring Decision Tree Machine Vision Systems in 2025 [https://www.unitxlabs.com/resources/decision-tree-machine-vision-system-2025-accuracy-speed/]
- 35. Changing Colors for Decision Tree Plot Using Sklearn ... [https://www.geeksforgeeks.org/machine-learning/changing-colors-for-decision-tree-plot-using-sklearn-plot-tree/]
- 36. Data-driven identification of biological systems using multi- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611157/]
- 37. Automatic Optimization for High-Quality Dataset Refinement [https://arxiv.org/html/2511.06530v1]
- 38. Driven to Near-Experimental Accuracy by Refinement via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6851469/]
- 39. Physiologically Based Pharmacokinetic Modeling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541349/]
- 40. Quality Assurance of PBPK Modeling Platforms and ... [https://link.springer.com/article/10.1007/s11095-022-03250-w]
- 41. Quantitative Systems Pharmacology: A Framework for Context [https://pmc.ncbi.nlm.nih.gov/articles/PMC4996481/]
- 42. The convergence of pharmacometrics and quantitative ... [https://www.sciencedirect.com/science/article/pii/S0928098723000118]
- 43. Methodologies for Quantitative Systems Pharmacology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5572127/]
- 44. The Impact of QSP Modeling on the Design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12625082/]
- 45. A deep dive into parameter estimation for advanced PBPK ... [https://www.sciencedirect.com/science/article/pii/S134743672400017X]
- 46. Best Practices to Maximize the Use and Reuse of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6533407/]
- 47. ACoP 2025 Insights: Scaling the Future of QSP Modeling ... [https://www.certara.com/blog/acop-2025-insights-scaling-the-future-of-qsp-modeling-with-certara-iq/]
- 48. Genome Variant Refinement Pipeline (GVRP) [https://github.com/Jeong-Hoon-Choi/GVRP]
- 49. Why Your Model Isn't Hitting Target Accuracy [https://www.hivelocity.net/blog/model-accuracy-troubleshooting-guide/]
- 50. Best practices for variant calling in clinical sequencing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7586657/]
- 51. Summoning insights: NGS variant calling best practice [https://www.ogt.com/ca/resources/ngs-resources-and-support/ngs-resources/summoning-insights-ngs-variant-calling-best-practices/]
- 52. Overfitting and Underfitting 2025 Avoid the Biggest Mistakes [https://w3schools.cloud/avoid-the-biggest-overfitting-and-underfitting/]
- 53. How to Fix Overfitting and Underfitting | by Tahir | Oct, 2025 [https://medium.com/@tahirbalarabe2/how-to-fix-overfitting-and-underfitting-4cf8f383ea96]
- 54. "Mastering Model Complexity: A Guide to Selection, ... [https://medium.com/@gowthamiarva28/mastering-model-complexity-a-guide-to-selection-overfitting-and-underfitting-af5024539a65]
- 55. What is Overfitting in Deep Learning [+10 Ways to Avoid It] [https://www.v7labs.com/blog/overfitting]
- 56. ML | Underfitting and Overfitting [https://www.geeksforgeeks.org/machine-learning/underfitting-and-overfitting-in-machine-learning/]
- 57. Model Complexity & Overfitting in Machine Learning [https://www.geeksforgeeks.org/machine-learning/model-complexity-overfitting-in-machine-learning/]
- 58. Balancing Complexity and Interpretability in Machine ... [https://www.linkedin.com/advice/0/how-can-you-balance-complexity-interpretability-machine]
- 59. CERTAINTY 2025: The power of Model-Informed Drug ... [https://www.certara.com/blog/certainty-the-power-of-model-informed-drug-development/]
- 60. AI Model Optimization Techniques for Enhanced ... [https://www.netguru.com/blog/ai-model-optimization]
- 61. Iterative refinement and goal articulation to optimize large ... [https://www.nature.com/articles/s41746-025-01686-z]
- 62. On the Biology of a Large Language Model [https://transformer-circuits.pub/2025/attribution-graphs/biology.html]
- 63. a mechanism analysis within a cluster-randomized controlled ... [https://implementationscience.biomedcentral.com/articles/10.1186/s13012-025-01437-4]
- 64. 10 Techniques to Solve Imbalanced Classes in Machine ... [https://www.analyticsvidhya.com/blog/2020/07/10-techniques-to-deal-with-class-imbalance-in-machine-learning/]
- 65. 8 Tactics to Combat Imbalanced Classes in Your ... [https://www.machinelearningmastery.com/tactics-to-combat-imbalanced-classes-in-your-machine-learning-dataset/]
- 66. Class-imbalanced datasets | Machine Learning [https://developers.google.com/machine-learning/crash-course/overfitting/imbalanced-datasets]
- 67. Class Imbalance Strategies — A Visual Guide with Code [https://medium.com/data-science/class-imbalance-strategies-a-visual-guide-with-code-8bc8fae71e1a]
- 68. Performance Trade-offs of Optimizing Small Language ... [https://arxiv.org/html/2510.21970v1]
- 69. Revisit Reasoning Tasks via a Causal Lens [https://arxiv.org/html/2510.08222v1]
- 70. Common Challenges in Clinical Research and Solutions [https://ccrps.org/clinical-research-blog/common-challenges-in-clinical-research-and-how-to-overcome-them]
- 71. Q&A with Rob Scott: evolving clinical trial with design ... [https://www.zs.com/insights/bringing-clinical-trial-optimization-into-the-21st-century]
- 72. Using Dose-Escalation and -Expansion Cohort Study as ... [https://pubmed.ncbi.nlm.nih.gov/40749153/]
- 73. Principles of designing a clinical trial: optimizing chances of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6241291/]
- 74. Expansion Cohorts: Use in First-In-Human Clinical Trials to ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/expansion-cohorts-use-first-human-clinical-trials-expedite-development-oncology-drugs-and-biologics]
- 75. Approaches to Model Validation [https://select-statistics.co.uk/blog/approaches-to-model-validation/]
- 76. What is the difference between in-sample and out-of- ... [https://milvus.io/ai-quick-reference/what-is-the-difference-between-insample-and-outofsample-forecasting]
- 77. AI Model Validation: Best Practices for Accuracy & Reliability [https://galileo.ai/blog/best-practices-for-ai-model-validation-in-machine-learning]
- 78. How to Check the Accuracy of Your Machine Learning ... [https://www.deepchecks.com/how-to-check-the-accuracy-of-your-machine-learning-model/]
- 79. 12 Important Model Evaluation Metrics for Machine ... [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 80. forecasting - What is difference between “in-sample” and “ ... [https://stats.stackexchange.com/questions/260899/what-is-difference-between-in-sample-and-out-of-sample-forecasts]
- 81. In Sample vs Out of Sample Testing [https://www.benchmarksixsigma.com/forum/topic/39581-in-sample-vs-out-of-sample-testing/]
- 82. Evaluation Metrics for ML Models in Drug Discovery [https://www.elucidata.io/blog/evaluation-metrics-for-ml-models-in-drug-discovery]
- 83. Understanding Precision, Recall, and F1 Score Metrics [https://medium.com/@piyushkashyap045/understanding-precision-recall-and-f1-score-metrics-ea219b908093]
- 84. Classification: Accuracy, recall, precision, and related metrics [https://developers.google.com/machine-learning/crash-course/classification/accuracy-precision-recall]
- 85. What is Accuracy, Precision, Recall and F1 Score? [https://www.labelf.ai/blog/what-is-accuracy-precision-recall-and-f1-score]
- 86. Model Evaluation Metrics — Accuracy, Precision, Recall, and ... [https://ianclemence.medium.com/day-31-model-evaluation-metrics-accuracy-precision-recall-and-f1-score-64c41126a2b9]
- 87. An Improved Metric and Benchmark for Assessing ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/38560736/]
- 88. Confusion Matrix Visualization [https://medium.com/@dtuk81/confusion-matrix-visualization-fc31e3f30fea]
- 89. Cross-Validation Visualized: A Narrative Guide to ... [https://www.mdpi.com/2504-4990/6/2/65]
- 90. “From Hold - Out to K - Fold : Understanding Cross - Validation ... Methods [https://medium.com/@kavyasrirelangi100/from-hold-out-to-k-fold-understanding-cross-validation-methods-in-machine-learning-37402f406759]
- 91. Step Forward Cross for Bioactivity Prediction: Out of... Validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC11245006/]
- 92. Improved protein structure refinement guided by deep ... [https://www.nature.com/articles/s41467-021-21511-x]
- 93. Using Validation Dataset and Cross - validation Techniques [https://www.deepchecks.com/evaluating-model-performance-using-validation-dataset-splits-and-cross-validation-techniques/]
- 94. GitHub - Pradnya1208/ Cross - Validation - techniques : This project... [https://github.com/Pradnya1208/Cross-Validation-techniques]
- 95. Solving 9 Common Cross-Validation Mistakes [https://medium.com/@jan_marcel_kezmann/solving-9-common-cross-validation-mistakes-ac8a6a6944e7]
- 96. Two Common Pitfalls to Avoid When Doing Cross-Validation [https://towardsdatascience.com/two-common-pitfalls-to-avoid-when-doing-cross-validation-c68ed79c0e4e/]
- 97. Transforming Drug Target Discovery ... [https://insilico.com/tpost/v49bfcu0r1-transforming-drug-target-discovery-insil]
- 98. Learning a refinement model for variant analysis in non-human primate genomes | BMC Genomics | Full Text [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11921-2]
- 99. How to Troubleshoot Sequencing Preparation Errors (NGS ... [https://www.cd-genomics.com/resource-sequencing-preparation-troubleshooting.html]
- 100. Troubleshooting Guide for Genomic DNA Extraction & ... [https://www.neb.com/en-us/tools-and-resources/troubleshooting-guides/troubleshooting-guide-for-t3010?srsltid=AfmBOoouY_JCsyGpUNP9FIAnYvO1UoWQfFSi62in92yPsbKtWBLbI-pf]