From Spectra to Signatures: A Modern Pipeline for Biomarker Discovery in Proteomic Mass Spectrometry
This article provides a comprehensive guide for researchers and drug development professionals on the end-to-end pipeline for identifying and validating protein biomarkers using mass spectrometry.
From Spectra to Signatures: A Modern Pipeline for Biomarker Discovery in Proteomic Mass Spectrometry
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the end-to-end pipeline for identifying and validating protein biomarkers using mass spectrometry. Covering the journey from foundational concepts and experimental design to advanced data acquisition, troubleshooting, and rigorous validation, it synthesizes current best practices and technological innovations. Readers will gain a practical framework for designing robust discovery studies, overcoming common analytical challenges, and translating proteomic findings into clinically actionable biomarkers, with insights drawn from recent advancements and comparative platform analyses.
Laying the Groundwork: Principles and Design for Robust Biomarker Discovery
In the realm of modern molecular medicine and proteomic research, biomarkers are indispensable tools for bridging the gap between benchtop discovery and clinical application. The Biomarkers, EndpointS, and other Tools (BEST) resource, a joint initiative by the U.S. Food and Drug Administration (FDA) and the National Institutes of Health (NIH), defines a biomarker as "a defined characteristic that is measured as an indicator of normal biological processes, pathogenic processes, or responses to an exposure or intervention" [1]. Within the pipeline for identifying biomarkers from proteomic mass spectrometry data, a critical first step is the precise classification of these biomarkers based on their clinical application. This classification directly influences study design, analytical validation, and ultimate clinical utility [1] [2]. This article delineates the three foundational classifications—diagnostic, prognostic, and predictive—providing a structured framework for researchers and drug development professionals engaged in mass spectrometry-based biomarker discovery.
Biomarker Classification and Clinical Applications
Biomarkers are categorized by their specific clinical function, which dictates their role in patient management and therapeutic development. The table below summarizes the core definitions and applications of diagnostic, prognostic, and predictive biomarkers.
Table 1: Classification and Application of Key Biomarker Types
| Biomarker Type | Primary Function | Clinical Context of Use | Representative Examples |
|---|---|---|---|
| Diagnostic | Detects or confirms the presence of a disease or a specific disease subtype [1] [3]. | Symptomatic individuals; aims to identify the disease and classify its subtype for initial management [1]. | Prostate-Specific Antigen (PSA) for prostate cancer [4], C-reactive protein (CRP) for inflammation [5], Glial fibrillary acidic protein (GFAP) for traumatic brain injury [3]. |
| Prognostic | Provides information about the likely natural history of a disease, including risk of recurrence or mortality, independent of therapeutic intervention [3] [5]. | Already diagnosed individuals; informs on disease aggressiveness and overall patient outcome, guiding long-term monitoring and care intensity [3]. | Ki-67 (MKI67) protein for cell proliferation in cancers [5], Mutated PIK3CA in metastatic breast cancer [3]. |
| Predictive | Identifies the likelihood of a patient responding to a specific therapeutic intervention, either positively or negatively [1] [5]. | Prior to treatment initiation; enables therapy selection for individual patients, forming the basis of personalized medicine [1]. | HER2/neu status for trastuzumab response in breast cancer [3] [5], EGFR mutation status for tyrosine kinase inhibitors in non-small cell lung cancer [3] [5]. |
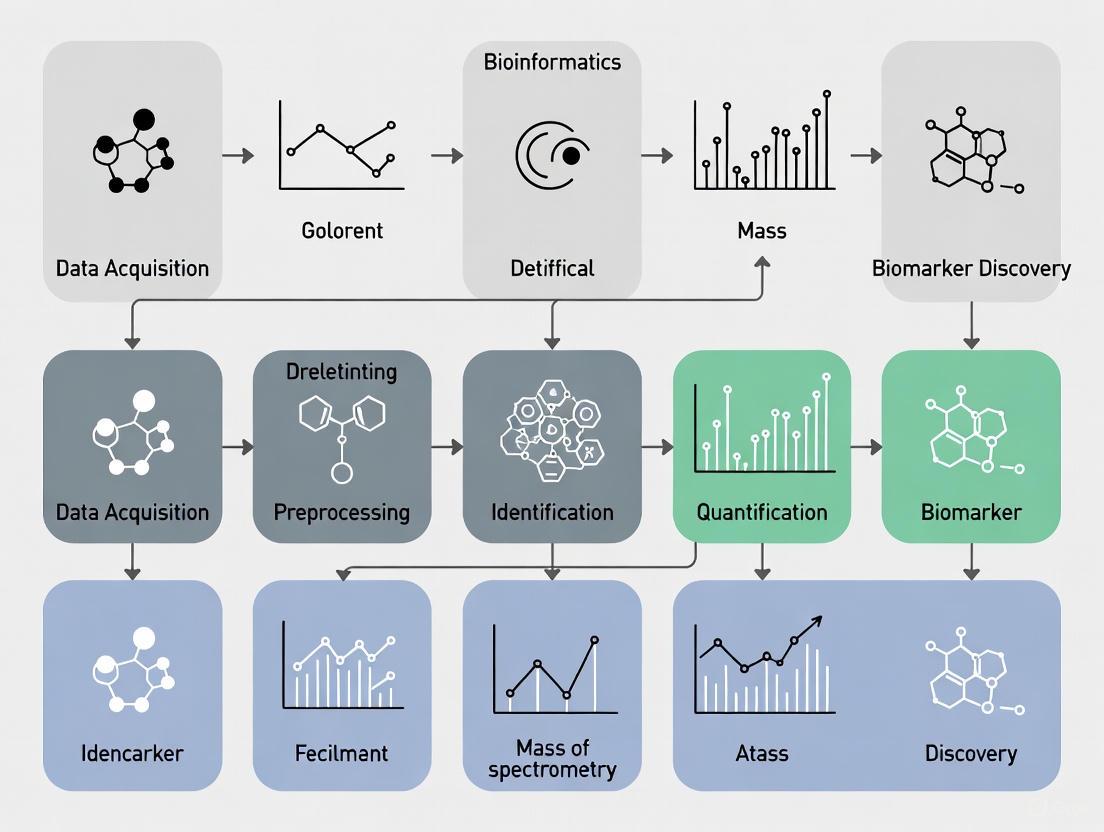
The following diagram illustrates the relationship between these biomarker types and their specific roles in the patient journey.
Integrated Mass Spectrometry Workflow for Biomarker Discovery
The discovery and validation of protein biomarkers using mass spectrometry (MS) require a rigorous, multi-stage pipeline. This process transitions from broad, untargeted discovery to highly specific and validated assays, ensuring that only the most robust candidates advance [6] [2]. The pipeline is characterized by an inverse relationship between the number of proteins quantified and the number of patient samples analyzed, with different MS techniques being optimal for each phase [6].
Stages of the Biomarker Pipeline
- Biomarker Discovery: This initial phase utilizes non-targeted, "shotgun" proteomics to relatively quantify thousands of proteins across a small number of samples (e.g., 10-20 per group) [6] [7]. Techniques like data-independent acquisition (DIA) mass spectrometry or isobaric labeling (e.g., TMT, iTRAQ) are commonly employed to identify proteins that are differentially expressed between diseased and healthy cohorts [6] [8]. The output is a list of hundreds of candidate proteins with associated fold-changes.
- Biomarker Verification: The long list of candidates from the discovery phase is filtered down using higher-specificity mass spectrometry, often targeted methods like Multiple Reaction Monitoring (MRM) or SRM [6]. This step verifies the differential expression of a smaller panel of proteins (tens to hundreds) in a larger, independent set of patient samples (typically 50-100) [6] [2].
- Biomarker Validation: This critical final preclinical phase involves the absolute quantitation of a small number of lead biomarker candidates (fewer than 10) in a large, well-defined clinical cohort (100-500+ samples) [6] [2]. The goal is to rigorously assess the clinical sensitivity, specificity, and predictive power of the biomarker(s) using analytically validated assays, which may still be MS-based or transition to immunoassays [6] [8].
Protocol: Data-Independent Acquisition (DIA) for Biomarker Discovery
Objective: To identify differentially expressed protein biomarkers between case and control groups from plasma/serum samples using a discovery proteomics approach.
Materials:
- Biological Samples: Matched case and control cohorts (e.g., n=492 total for sufficient statistical power) [8].
- Sample Preparation: Equipment for protein digestion (e.g., trypsin), desalting columns (e.g., C18 STAGE tips), and detergent removal.
- Liquid Chromatography-Mass Spectrometry (LC-MS/MS): High-resolution accurate mass (HRAM) instrument coupled to a nano-flow liquid chromatography system [8].
- Data Analysis Software: Tools for DIA data analysis (e.g., Spectronaut, DIA-NN, Skyline) and statistical analysis (e.g., R, Python).
Method Details:
- Sample Preparation and Randomization:
- Deplete high-abundance plasma proteins (e.g., albumin, IgG) to enhance depth of coverage.
- Perform reduction, alkylation, and tryptic digestion of proteins according to standardized protocols [2] [8].
- Desalt and purify peptides.
- Critical Step: Randomize the order of sample analysis by LC-MS/MS to prevent batch effects from confounding biological differences [2].
LC-MS/MS Data Acquisition:
- Separate peptides using a reversed-phase nano-LC gradient.
- Acquire DIA-MS data on the HRAM mass spectrometer. In DIA mode, the instrument fragments all ions within sequential, pre-defined m/z isolation windows, covering the entire mass range of interest [8].
Data Processing and Protein Quantification:
- Process the raw DIA data using specialized software (e.g., TEAQ - Targeted Extraction Assessment of Quantification) to extract peptide precursor signals and quantify proteins [8].
- The software should assess analytical quality criteria, including:
- Linearity: Correlation between peptide abundance and sample load.
- Specificity: Uniqueness of the peptide signal to a single protein.
- Repeatability/Reproducibility: Low coefficient of variation across technical replicates [8].
Statistical Analysis and Biomarker Candidate Selection:
- Normalize protein abundance data across all samples.
- Perform statistical tests (e.g., t-tests, ANOVA) adjusted for multiple comparisons (e.g., Benjamini-Hochberg) to identify proteins significantly differentially expressed between case and control groups.
- Apply feature selection algorithms or machine learning models (e.g., logistic regression, random forest) to identify a panel of biomarker candidates with the highest classification power [9].
Expected Outcomes: A list of verified peptide precursors and their parent proteins that are significantly altered in the disease cohort and meet pre-defined analytical quality metrics, ready for downstream validation.
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential reagents and materials required for a mass spectrometry-based biomarker discovery and validation pipeline.
Table 2: Essential Research Reagents and Materials for MS-Based Biomarker Pipeline
| Reagent / Material | Function / Application |
|---|---|
| Trypsin, Sequencing Grade | Proteolytic enzyme for specific digestion of proteins into peptides for LC-MS/MS analysis [6]. |
| C18 Solid-Phase Extraction Tips | Desalting and purification of peptide mixtures after digestion and prior to LC-MS injection [2]. |
| Isobaric Tagging Reagents (e.g., TMT, iTRAQ) | Chemical labels for multiplexed relative protein quantitation across multiple samples in a single MS run [6]. |
| Stable Isotope-Labeled Peptide Standards (SIS) | Synthetic peptides with heavy isotopes for absolute, precise quantitation of target proteins in validation assays (e.g., MRM) [6]. |
| High-Abundancy Protein Depletion Columns | Immunoaffinity columns for removing highly abundant proteins (e.g., albumin) from plasma/serum to improve detection of low-abundance biomarkers [8]. |
| Quality Control (QC) Pooled Sample | A representative pool of all samples analyzed repeatedly throughout the MS sequence to monitor instrument performance and data quality [2]. |
The precise classification of biomarkers into diagnostic, prognostic, and predictive categories is a foundational element that directs the entire proteomic research pipeline. From initial experimental design to final clinical application, understanding the distinct clinical question each biomarker type addresses is paramount for developing meaningful and impactful tools. The structured workflow from MS-based discovery through rigorous verification and validation, supported by the appropriate toolkit of reagents and protocols, provides a robust pathway for translating proteomic data into clinically actionable biomarkers. This systematic approach ultimately empowers the development of personalized medicine, enabling more accurate diagnoses, informed prognosis, and effective, tailored therapies.
The Critical Role of Experimental Design and Cohort Selection
The journey from a mass spectrometry (MS) run to a clinically validated biomarker is fraught with potential for failure. Often, the root cause of such failures is not the analytical technology itself, but fundamental flaws in the initial planning of the study. Rigorous experimental design and meticulous cohort selection are the most critical, yet frequently underappreciated, components of a successful biomarker discovery pipeline [10] [11]. These initial steps form the foundation upon which all subsequent data generation, analysis, and validation are built; a weak foundation inevitably leads to unreliable and non-reproducible results. This document outlines detailed protocols and application notes to guide researchers in designing robust and statistically sound proteomic studies, thereby enhancing the rigor and credibility of biomarker development [10].
Principles of Cohort Selection
The selection of study subjects is a cornerstone of biomarker research, as an ill-defined cohort can introduce bias and confound results, dooming a project from the start.
Defining Cases and Controls
The clarity and precision with which case and control groups are defined directly impact the specificity and generalizability of the discovered biomarkers [10].
- Cases: Patient groups should be defined using established diagnostic criteria. This includes clear clinical characteristics, standardized laboratory test results, and well-defined disease stages. The stringency of these criteria involves a trade-off between cohort purity and the eventual clinical applicability of the biomarker.
- Controls: Control subjects must be carefully matched to cases to minimize the influence of confounding variables. As outlined in Table 1, control groups can range from healthy individuals to patients with other diseases that share symptomatic similarities. The most robust studies often include multiple control groups to distinguish disease-specific biomarkers from general indicators of inflammation or other physiological states [10].
Managing Bias and Confounding Factors
Observational studies are particularly susceptible to biases that can skew results [10].
- Selection Bias: This occurs when the study subjects are not representative of the target population. To mitigate this, recruitment strategies should be based on well-defined inclusion/exclusion criteria applied equally to all participants. The use of consecutive recruitment from clinical pathways is a recommended practice [10].
- Confounding Factors: These are variables that are associated with both the exposure and the outcome. Common confounders in clinical proteomics include age, sex, body mass index (BMI), and comorbidities. Statistical methods like inverse probability weighting and post-stratification can be employed to adjust for these factors during data analysis [10].
Table 1: Types of Control Groups in Biomarker Studies
| Control Type | Description | Key Utility | Considerations |
|---|---|---|---|
| Healthy Controls | Individuals with no known history of the disease. | Establishes a baseline "normal" proteomic profile. | May not account for proteins altered due to non-specific factors (e.g., stress, minor inflammation). |
| Disease Controls | Patients with a different disease, often with symptomatic overlap. | Helps identify biomarkers specific to the disease of interest rather than general illness. | Crucial for verifying specificity and reducing false positives. |
| Pre-clinical/Longitudinal Controls | Individuals who later develop the disease, identified from longitudinal cohorts. | Allows discovery of early detection biomarkers before clinical symptoms manifest. | Requires access to well-annotated, prospective biobanks. |
Experimental Design and Statistical Considerations
A powerful and well-controlled experimental design is essential for detecting true biological signals amidst technical noise.
Power and Sample Size
A critical early step is the calculation of statistical power to determine the necessary sample size. Underpowered studies are a major contributor to irreproducible research, as they lack the sensitivity to detect anything but very large effect sizes [10]. Sample size should be estimated based on the expected fold-change in protein abundance and the biological variability within the groups. Tools for power analysis in proteomics are available and must be utilized during the planning phase to ensure the study is capable of answering its central hypothesis [10].
Randomization, Blinding, and Replication
Incorporating these elements is non-negotiable for ensuring the integrity of the data [10] [11].
- Randomization: The assignment of samples to processing batches and MS run orders must be randomized. This prevents technical artifacts (e.g., instrument drift, reagent batch effects) from being systematically correlated with biological groups.
- Blinding: Technicians and analysts should be blinded to the group identity of the samples (e.g., case vs. control) during sample processing, data acquisition, and initial data processing to prevent unconscious bias.
- Replication: Both technical and biological replicates are essential.
- Technical Replicates: Multiple injections of the same sample assess instrumental precision.
- Biological Replicates: Multiple individuals per group account for natural biological variation and are required for robust statistical inference.
The following workflow diagram integrates the key components of cohort selection and experimental design into a coherent pipeline.
Quality Control and Data Acquisition
Robust quality control (QC) measures are implemented throughout the process to ensure data reliability [10] [11].
- Sample Preparation QC: Protein concentration should be measured using a standardized assay (e.g., BCA assay) before digestion. A common best practice is to include a "QC pool" sample, created by combining a small aliquot of every sample in the study. This QC pool is then analyzed repeatedly throughout the MS acquisition sequence to monitor technical performance.
- Mass Spectrometry QC: The instrument performance should be evaluated using complex standard digests (e.g., HeLa cell digest) to ensure sensitivity and stability over time. Monitoring metrics like peptide identification rates, retention time stability, and intensity distribution is crucial.
An Integrated Pipeline for Biomarker Translation
The ultimate goal of discovery is translation into a clinically usable assay. The pipeline must therefore be designed with validation in mind from the outset.
From Discovery to Targeted Assays
Data-Independent Acquisition (DIA-MS) has emerged as a powerful discovery strategy because it combines deep proteome coverage with high reproducibility [8]. The data generated can be directly mined to transition into targeted mass spectrometry assays (e.g., SRM/PRM), which are the standard for precise biomarker verification and validation. Software tools like the Targeted Extraction Assessment of Quantification (TEAQ) have been developed to automatically select the most reliable peptide precursors from DIA-MS data based on analytical criteria such as linearity, specificity, and reproducibility, thereby streamlining the development of targeted assays [8].
Integration of Machine Learning
Machine learning (ML) models are increasingly used to identify complex patterns in high-dimensional proteomic data [12] [9]. A typical ML pipeline for biomarker discovery, as applied in areas like prostate cancer research, involves:
- Feature Selection: Reducing the thousands of detected proteins to a panel of the most informative biomarkers using statistical methods or ML-based feature importance [9].
- Model Training: Training multiple classifiers (e.g., Logistic Regression, Random Forest, Support Vector Machines) on the selected features to distinguish between patient groups [9].
- Model Ensembling: Combining predictions from multiple models through a voting mechanism to improve overall classification accuracy and robustness [9]. Such pipelines have demonstrated success in identifying novel peptide panels with high predictive performance for disease classification [9].
Table 2: Essential Research Reagents and Materials for Proteomic Workflows
| Item Category | Specific Examples | Critical Function |
|---|---|---|
| Sample Preparation | Trypsin/Lys-C protease, RapiGest SF, Dithiothreitol (DTT), Iodoacetamide (IAA), C18 solid-phase extraction plates | Protein digestion, disulfide bond reduction, alkylation, and peptide desalting/purification. |
| Chromatography | LC-MS grade water/acetonitrile, Formic Acid, C18 reversed-phase UHPLC columns | Peptide separation prior to MS injection to reduce complexity and enhance identification. |
| Mass Spectrometry | Mass calibration solution (e.g., ESI Tuning Mix), Quality control reference digest (e.g., HeLa digest) | Instrument calibration and performance monitoring to ensure data quality and reproducibility. |
| Data Analysis | Protein sequence databases (e.g., Swiss-Prot), Software platforms (e.g., MaxQuant, Spectronaut, TEAQ), Standard statistical packages (R, Python) | Protein identification, quantification, and downstream bioinformatic analysis for biomarker candidate selection. |
The following diagram illustrates the informatics pipeline that integrates machine learning for biomarker signature identification.
The path to a clinically useful biomarker is long and complex, but its success is largely determined at the very beginning. A deliberate and rigorous approach to cohort selection and experimental design is not merely a procedural formality but the fundamental engine of discovery. By adhering to the principles outlined in this protocol—careful subject matching, power analysis, randomization, blinding, and planning for validation—researchers can significantly enhance the reliability, reproducibility, and translational potential of their proteomic biomarker studies.
In the proteomic mass spectrometry pipeline for biomarker discovery, the choice of biological sample is a foundational decision that profoundly influences the success and clinical relevance of the research. Blood-derived samples (plasma and serum) and proximal fluids represent two complementary approaches, each with distinct advantages for specific clinical questions. Plasma and serum provide a systemic overview of an organism's physiological and pathological state, making them ideal for detecting widespread diseases and monitoring therapeutic responses. In contrast, proximal fluids—bodily fluids in close contact with specific organs or tissue compartments—offer a concentrated source of tissue-derived proteins that often reflect local pathophysiology with greater specificity [13] [14].
The biomarker development pipeline necessitates different sample strategies across its phases. Discovery phases often benefit from the enriched signal in proximal fluids, while validation and clinical implementation typically require the accessibility and systemic perspective of blood samples [6]. This application note examines the advantages, limitations, and appropriate contexts for using these sample types, providing structured comparisons and detailed protocols to inform researchers' experimental designs within the broader biomarker identification pipeline.
Comparative Analysis of Sample Types
Fundamental Characteristics and Applications
Table 1: Core Characteristics and Applications of Major Sample Types
| Sample Type | Definition & Composition | Key Advantages | Primary Limitations | Ideal Use Cases |
|---|---|---|---|---|
| Plasma | Liquid component of blood containing fibrinogen and other clotting factors; obtained via anticoagulants [15]. | - Represents systemic circulation- Good stability of analytes- Enables repeated sampling- Standardized collection protocols | - High dynamic range of protein concentration (~1010)- High abundance of proteins (e.g., albumin) can mask low-abundance biomarkers [13] | - Systemic disease monitoring- Drug pharmacokinetic studies- Cardiovascular and metabolic disorders |
| Serum | Liquid fraction remaining after blood coagulation; fibrinogen and clotting factors largely removed [15]. | - Lacks anticoagulant additives- Clotting process removes some high-abundance proteins- Well-established historical data | - Potential loss of protein biomarkers during clotting- Variable composition due to clotting time/temperature | - Oncology biomarkers (e.g., CA-125, CA19-9) [6]- Historical cohort studies- Autoimmune disease profiling |
| Proximal Fluids | Fluids derived from extracellular milieu of specific tissues (e.g., CSF, synovial fluid, nipple aspirate) [13]. | - Enriched with tissue-derived proteins- Higher relative concentration of disease-related proteins vs. plasma/serum [13]- Reduced complexity and dynamic range | - Often more invasive collection procedures- Lower total volume typically obtained- Potential blood contamination issues [14] | - Central nervous system disorders (CSF) [14] [16]- Breast cancer (nipple aspirate) [17]- Joint diseases (synovial fluid) |
Quantitative Proteomic Depth Across Sample Types
The capability to identify proteins from different sample sources varies significantly based on their complexity and the methodologies employed.
Table 2: Typical Proteomic Depth Achievable Across Sample Types
| Sample Type | Typical Protein Identifications | Key Methodological Considerations | Reported Examples |
|---|---|---|---|
| Cerebrospinal Fluid (CSF) | 2,615 proteins from 6 individual samples using SCX fractionation and LC-MS/MS [14] | - Often requires minimal depletion due to lower albumin content- Fractionation significantly increases proteome coverage | 78 brain-specific proteins identified using Human Protein Atlas database mining [14] |
| Plasma/Serum | 1,179 proteins identified; 326 quantifiable proteins from a cohort of 492 IBD patients using DIA-MS [8] | - Requires high-abundance protein depletion (e.g., albumin, immunoglobulins)- Advanced fractionation and high-resolution MS essential for depth | 8-protein panel for Parkinson's disease prediction validated in plasma [18] |
| Cell Line Media (Proximal Fluid Surrogate) | 249 proteins detected from 7 breast cancer cell lines [17] | - Controlled environment reduces complexity- Enables study of specific cellular phenotypes without in vivo complexity | Predictive categorization of HER2 status using two proteins [17] |
Advantages of Proximal Fluids in Biomarker Discovery
Biological Rationale and Technical Advantages
Proximal fluids offer distinct advantages for biomarker discovery, particularly in the early stages of the pipeline:
Enhanced Biological Relevance: Proximal fluids reside in direct contact with their tissues of origin, creating a dynamic exchange where shed and secreted proteins from the tissue microenvironment accumulate. Cerebrospinal fluid (CSF), for instance, communicates closely with brain tissue and contains numerous brain-derived proteins, with approximately 20% of its total protein content secreted by the central nervous system [14]. This proximity means that disease-related proteins are often present at higher concentrations relative to their diluted counterparts in systemic circulation [13].
Reduced Complexity: The dynamic range of protein concentrations in plasma and serum spans approximately ten orders of magnitude, creating significant analytical challenges for detecting low-abundance, disease-relevant proteins [13]. Proximal fluids like CSF have a less complex proteome with a narrower dynamic range, facilitating the detection of potentially significant biomarkers that would be masked in blood samples.
Tissue-Specific Protein Enrichment: Proximal fluids are enriched for tissue-specific proteins. For example, the CSF proteome is characterized by a high fraction of membrane-bound and secreted proteins, which are overrepresented compared to blood and represent respectable biomarker candidates [14]. Mining of the Human Protein Atlas database against experimental CSF proteome data has identified 78 brain-specific proteins, creating a valuable signature for CNS disease diagnostics [14].
Practical Workflow: CSF Proteomic Analysis
The following diagram illustrates a highly automated, scalable pipeline for CSF proteome analysis, designed for biomarker discovery in central nervous system disorders.
Diagram 1: Automated CSF proteomics workflow for biomarker discovery. This scalable pipeline enables large-scale clinical studies while maintaining comprehensive proteome coverage. Sample preparation begins with clearance centrifugation and proceeds through standard proteolytic processing before strong cation exchange (SCX) fractionation and high-resolution LC-MS/MS analysis [14] [16].
Detailed Protocol: CSF Proteome Preparation for Biomarker Discovery
Protocol Objective: To prepare cerebrospinal fluid samples for comprehensive proteomic analysis using fractionation and LC-MS/MS, enabling identification of brain-enriched proteins.
Materials & Reagents:
- Clear, non-hemolyzed CSF samples (stored at -80°C)
- RapiGest SF Surfactant (Waters)
- Dithiothreitol (DTT)
- Iodoacetamide (IAA)
- Sequencing-grade modified trypsin
- Ammonium bicarbonate
- Trifluoroacetic acid (TFA)
- Formic acid
- Acetonitrile (HPLC grade)
- Strong cation exchange (SCX) PolySULFOETHYL Column
Procedure:
- Sample Preparation: Thaw CSF samples at room temperature and centrifuge at 17,000 × g for 10 minutes to remove any insoluble material or cells [14].
- Protein Denaturation & Reduction: Adjust CSF volume equivalent to 300 µg total protein. Add RapiGest to 0.05% final concentration and DTT to 5 mM final concentration. Incubate at 60°C for 40 minutes [14].
- Alkylation: Add iodoacetamide to 15 mM final concentration. Incubate for 60 minutes in the dark at room temperature [14].
- Trypsin Digestion: Add trypsin in 50 mM ammonium bicarbonate (1:30 trypsin-to-protein ratio). Incubate for 18 hours at 37°C [14].
- Digestion Termination: Add trifluoroacetic acid to 1% final concentration to stop digestion and cleave RapiGest. Centrifuge at 500 × g for 30 minutes to remove insoluble debris [14].
- Peptide Fractionation: Dilute trypsinized samples two-fold with SCX Buffer A (0.26 M formic acid, 5% acetonitrile). Load onto SCX column and elute with a gradient of SCX Buffer B (0.26 M formic acid, 5% acetonitrile, 1 M ammonium formate) over 70 minutes. Collect 15-16 fractions per sample based on UV monitoring at 280 nm [14].
- Desalting: Purify peptides from each fraction using C18 solid-phase extraction tips. Elute with 65% acetonitrile, 0.1% formic acid, and dilute to 0.01% formic acid for MS analysis [14].
Quality Control Notes:
- Monitor sample clarity before processing; discard samples with visible blood contamination.
- Include a pooled quality control sample across runs to monitor technical variability.
- Expected protein identification range: 1,100-1,400 proteins per individual CSF sample with 21% inter-individual variability [14].
Advantages of Plasma and Serum in Biomarker Validation and Clinical Translation
Strategic Value in the Biomarker Pipeline
While proximal fluids excel in discovery phases, plasma and serum offer complementary strengths that make them indispensable for validation and clinical implementation:
Clinical Practicality: Blood collection is minimally invasive, standardized, and integrated into routine clinical practice worldwide. This enables large-scale cohort studies, repeated sampling for longitudinal monitoring, and eventual translation into clinical diagnostics. The recent development of high-throughput targeted mass spectrometry assays has further enhanced the utility of plasma for large validation studies [8] [18].
Systemic Perspective: Plasma and serum provide a comprehensive view of systemic physiology, capturing signaling molecules, tissue leakage proteins, and immune mediators from throughout the body. This systemic perspective is particularly valuable for multifocal diseases, metastatic cancers, and systemic inflammatory conditions.
Established Infrastructure: Well-characterized protocols for sample collection, processing, and storage exist for plasma and serum, along with established quality control measures and commercial reference materials (e.g., NIST SRM 1950) [15]. This infrastructure supports reproducible and comparable results across laboratories and studies.
Advanced Workflow: Plasma Biomarker Verification Pipeline
The following diagram outlines a targeted proteomics pipeline for verification of biomarker candidates discovered in plasma, bridging the gap between discovery and clinical validation.
Diagram 2: Plasma biomarker verification pipeline using TEAQ. The Targeted Extraction Assessment of Quantification (TEAQ) software bridges discovery and validation by selecting precursors, peptides, and proteins from DIA-MS data that meet strict analytical criteria required for clinical assays [8].
Case Study: Plasma Biomarker Panel for Parkinson's Disease
A recent study exemplifies the power of plasma proteomics for neurological disease biomarker development. Researchers employed a multi-phase approach:
Discovery Phase: Unbiased LC-MS/MS analysis of depleted plasma from 10 drug-naïve Parkinson's disease (PD) patients and 10 matched controls identified 895 distinct proteins, with 47 differentially expressed [18].
Targeted Assay Development: A multiplexed targeted MS assay was developed for 121 proteins, focusing on inflammatory pathways implicated in PD pathogenesis [18].
Validation: Application to an independent cohort (99 PD patients, 36 controls, 41 other neurological diseases, 18 isolated REM sleep behavior disorder [iRBD] patients) confirmed 23 significantly differentially expressed proteins in PD versus controls [18].
Panel Refinement: Machine learning identified an 8-protein panel (including Granulin precursor, Complement C3, and Intercellular adhesion molecule-1) that accurately identified all PD patients and 79% of iRBD patients up to 7 years before motor symptom onset [18].
This case study demonstrates how plasma proteomics, coupled with advanced computational analysis, can yield clinically actionable biomarkers even for disorders primarily affecting the central nervous system.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Sample Processing and Analysis
| Category | Specific Product/Technology | Application & Function | Key Considerations |
|---|---|---|---|
| Sample Preparation | RapiGest SF Surfactant (Waters) [14] | Acid-labile surfactant for protein denaturation; improves protein solubilization and digestion efficiency | Compatible with MS analysis; easily removed by acidification and centrifugation |
| Folch Extraction (Chloroform: Methanol, 2:1) [15] | Gold-standard method for lipid extraction from plasma/serum; provides excellent recovery rates and minimal matrix effects | Particularly valuable for lipidomic workflows; superior to single-phase extractions | |
| Chromatography | Strong Cation Exchange (SCX) PolySULFOETHYL Column [14] | Orthogonal peptide separation prior to RP-LC-MS/MS; significantly increases proteome coverage | Critical for deep profiling of complex samples; enables identification of low-abundance proteins |
| C18 Solid-Phase Extraction Tips [14] | Microscale desalting and concentration of peptide mixtures; prepares samples for MS analysis | Essential for cleaning up samples after digestion or fractionation; improves MS sensitivity | |
| Mass Spectrometry | Q-Exactive Plus Mass Spectrometer (Thermo Fisher) [14] | High-resolution accurate mass (HRAM) Orbitrap instrument; enables both discovery and targeted proteomics | Ideal for DIA and targeted methods; high sensitivity and mass accuracy |
| TripleQuadrupole Mass Spectrometer (e.g., SCIEX QTRAP) [6] | Gold standard for targeted quantitation via MRM/SRM; excellent sensitivity and quantitative precision | Preferred for validation studies; high reproducibility across large sample sets | |
| Data Analysis | TEAQ (Targeted Extraction Assessment of Quantification) [8] | Software pipeline for selecting biomarker candidates from DIA-MS data that meet analytical validation criteria | Bridges discovery and validation; selects peptides based on linearity, specificity, repeatability |
| Ingenuity Pathway Analysis (IPA, Qiagen) [18] | Bioinformatics tool for pathway analysis of proteomic data; identifies biologically relevant networks | Helps contextualize biomarker findings; identifies perturbed pathways in disease states |
Integrated Strategy for the Biomarker Pipeline
The most effective biomarker development strategies leverage both proximal fluids and blood samples at different pipeline stages:
Discovery Phase: Utilize proximal fluids (e.g., CSF for neurological disorders, nipple aspirate for breast cancer) to identify high-quality candidate biomarkers with strong biological rationale [14] [17].
Verification Phase: Develop targeted MS assays (e.g., MRM, TEAQ) to verify candidate biomarkers in plasma/serum from moderate-sized cohorts (50-100 patients) [8] [6].
Validation Phase: Conduct large-scale (100-1000+ samples) validation of refined biomarker panels in plasma/serum, focusing on clinical applicability and robustness [18].
Clinical Implementation: Translate validated biomarkers into clinical practice using plasma/serum-based tests, potentially incorporating automated sample preparation and high-throughput MS platforms [19].
This integrated approach maximizes the strengths of each sample type while acknowledging practical constraints, ultimately accelerating the development of clinically impactful biomarkers for early disease detection, prognosis, and therapeutic monitoring.
The journey to discovering a robust, clinically relevant biomarker from proteomic mass spectrometry data is a complex endeavor, highly susceptible to failure in its initial phases. Pre-analytical variability—introduced during sample collection, processing, and storage—represents a paramount challenge to the integrity of biospecimens and the validity of downstream data. In the context of a biomarker identification pipeline, inconsistencies in these early stages can artificially alter the plasma proteome, leading to irreproducible results, false leads, and ultimately, the failure of promising biomarkers to validate in independent cohorts. Evidence suggests that a significant portion of errors in omics studies originate in the pre-analytical phase, underscoring the critical need for standardized protocols [20]. This document outlines essential steps and controls to ensure sample quality, thereby enhancing the reproducibility and translational potential of proteomic mass spectrometry research.
Critical Pre-analytical Variables and Their Effects on the Proteome
A comprehensive understanding of how handling procedures affect biospecimens is the first step toward mitigation. The following variables have been demonstrated to significantly impact the plasma proteome.
Blood Collection and Processing Delays
The time interval between blood draw and plasma separation is one of the most critical factors. Research using an aptamer-based proteomic assay measuring 1305 proteins found that storing whole blood at room temperature for 6 hours prior to processing significantly changed the abundance of 36 proteins compared to immediate processing. When stored on wet ice (0°C) for the same duration, an even greater effect was observed, with 148 proteins changing significantly [21]. Another LC-MS study concluded that pre-processing times of less than 6 hours had minimal effects on the immunodepleted plasma proteome, but delays extending to 96 hours (4 days) induced significant changes in protein levels [22].
Centrifugation Conditions
The force applied during centrifugation to generate plasma can profoundly influence sample composition. The use of a lower centrifugal force (1300 × g) resulted in the most substantial alterations in the aptamer-based study, changing 200 out of 1305 proteins assayed. These changes are likely due to increased contamination of the plasma with platelets and cellular debris [21]. In contrast, a separate proteomic study comparing single- versus double-spun plasma showed minimal differences, suggesting that specific protocols must be benchmarked for their intended application [22].
Post-Processing and Storage Variables
After plasma separation, handling remains crucial. Holding plasma at room temperature or 4°C for 24 hours before freezing has been shown to activate the complement system in vitro and alter the abundance of 75 and 28 proteins, respectively [21]. Furthermore, multiple freeze-thaw cycles are a well-known risk. However, one LC-MS study indicated that the impact of ≤3 freeze-thaw cycles was negligible, regardless of whether they occurred in quick succession or over 14–17 years of frozen storage at -80 °C [22].
Phlebotomy Technique
The method of blood draw itself can be a source of variation. An exploratory study using Multiple Reaction Monitoring Mass Spectrometry (MRM-MS) found that different phlebotomy techniques (e.g., IV with vacutainer, butterfly with syringe) significantly affected 12 out of 117 targeted proteins and 2 out of 11 complete blood count parameters, such as red blood cell count and hemoglobin concentration [23].
Table 1: Summary of Pre-analytical Variable Effects on the Plasma Proteome
| Pre-analytical Variable | Experimental Conditions | Observed Impact on Proteome | Primary Citation |
|---|---|---|---|
| Blood Processing Delay | 6h at Room Temperature | 36 proteins significantly changed | [21] |
| Blood Processing Delay | 6h at 0°C (wet ice) | 148 proteins significantly changed | [21] |
| Blood Processing Delay | 96h at elevated temperature | Significant changes apparent; elevated protein levels | [22] |
| Centrifugation Force | 1300 × g vs. 2500 × g | 200 proteins significantly changed (196 increased) | [21] |
| Plasma Storage Delay | 24h at Room Temperature | 75 proteins changed; complement activation | [21] |
| Plasma Storage Delay | 24h at 4°C | 28 proteins changed; complement activation | [21] |
| Freeze-Thaw Cycles | ≤3 cycles | Negligible impact | [22] |
| Phlebotomy Technique | 4 different methods | 12 of 117 targeted proteins significantly changed | [23] |
Standardized Protocols for Plasma Collection and Processing
To mitigate the variables described above, the implementation of standardized protocols is non-negotiable. The following protocol, synthesizing recommendations from recent literature, is designed for the collection of K2 EDTA plasma, a common starting material for proteomic studies.
Materials and Reagents
- Blood Collection Tubes: Spray-coated K2 EDTA Vacutainer tubes (e.g., BD Vacutainer #368589).
- Equipment: Refrigerated centrifuge capable of maintaining 4°C and equipped with a horizontal rotor (swing-out bucket).
- Consumables: Sterile cryovials for plasma aliquoting.
Step-by-Step Procedure
- Blood Draw: Perform venipuncture with a 21-gauge needle or similar. Release the tourniquet within one minute of application [22]. Invert the K2 EDTA tubes 8 times immediately after collection to ensure proper mixing with the anticoagulant [22].
- Immediate Handling: Transport blood tubes to the processing laboratory at ambient temperature without delay.
- Initial Centrifugation: Centrifuge tubes within 30 minutes of collection. Use a refrigerated centrifuge (4°C) with a horizontal rotor set for 15 minutes at 1500-2500 × g [22] [21].
- Plasma Transfer: Carefully aspirate the upper plasma layer using a pipette, ensuring the buffy coat (white cell layer) is not disturbed. Transfer the plasma to a sterile 15 mL conical tube.
- Secondary Centrifugation (for platelet-poor plasma): To minimize platelet contamination, perform a second centrifugation step on the transferred plasma for 15 minutes at 2000 × g, 4°C [22].
- Aliquoting and Freezing: Pool plasma from the same donor (if multiple tubes were drawn) and aliquot into sterile cryovials (e.g., 0.5-1.0 mL per vial). Snap-freeze aliquots in liquid nitrogen or a dry-ice ethanol bath and transfer to a -80°C freezer for long-term storage [22] [21]. Avoid any freeze-thaw cycles.
Implementing a Comprehensive Quality Control Framework
A robust QC strategy combines the monitoring of known confounders with the use of standardized QC samples to track technical performance across the entire workflow.
Monitoring Key Pre-analytical Confounders
The International Society for Extracellular Vesicles (ISEV) Blood Task Force's MIBlood-EV framework provides a excellent model for reporting pre-analytical variables, focusing on key confounders [24]:
- Hemolysis: Qualitatively assess by visual inspection or quantitatively using a haematology analyzer. Hemolysis can release abundant cellular proteins that interfere with the plasma proteome.
- Residual Platelets: Quantify using a haematology analyzer post-centrifugation to ensure the effectiveness of the plasma preparation protocol.
- Lipoproteins: Monitor as these can co-isolate with targets of interest like extracellular vesicles and confound analysis.
Quality Control Samples for Mass Spectrometry
Incorporating well-characterized QC samples into the mass spectrometry workflow is essential for inspiring confidence in the generated data. These materials can be used for System Suitability Testing (SST) before a batch run and as process controls run alongside experimental samples [25].
Table 2: Quality Control Samples for Mass Spectrometry-Based Proteomics
| QC Level | Description | Example Materials | Primary Application |
|---|---|---|---|
| QC1 | Known mixture of purified peptides or protein digest | Pierce Peptide Retention Time Calibration (PRTC) Mixture | System Suitability Testing (SST), retention time calibration |
| QC2 | Digest of a known, complex whole-cell lysate or biofluid | HeLa cell digest, commercial yeast or E. coli lysate digest | Process control; monitors overall workflow performance |
| QC3 | QC2 sample spiked with isotopically labeled peptides (QC1) | Labeled peptides spiked into a HeLa cell digest | SST; enables monitoring of quantitative accuracy and detection limits |
| QC4 | Suite of different samples or mixed ratios | Two different cell lysates mixed in known ratios (e.g., 1:1, 1:2) | Evaluating quantitative accuracy and precision in label-free experiments |
These QC samples allow for the separation of instrumental variance from intrinsic biological variability. Data from many commercially available QC standards are available in public repositories like ProteomeXchange, enabling benchmarking of laboratory performance and data analysis workflows [25].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Kits for Standardized Proteomic Sample Preparation
| Reagent / Kit Name | Supplier | Function / Application |
|---|---|---|
| BD Vacutainer K2 EDTA Tubes | BD | Standardized blood collection for plasma preparation; contains spray-coated K2 EDTA anticoagulant. |
| Pierce Peptide Retention Time Calibration (PRTC) Mixture | Thermo Fisher Scientific | A known mixture of 15 stable isotope-labeled peptides used for LC-MS system suitability and retention time calibration. |
| MARS Hu-14 Immunoaffinity Column | Agilent Technologies | Depletes the top 14 high-abundance plasma proteins to enhance detection of lower-abundance potential biomarkers. |
| PreOmics iST Kit | PreOmics | An integrated sample preparation kit that streamlines protein extraction, digestion, and peptide cleanup into a single, automatable workflow. |
| SOMAscan Assay | SomaLogic | An aptamer-based proteomic assay for quantifying >1000 proteins in a small volume of plasma; useful for pre-analytical stability studies. |
The following diagram synthesizes the key stages, decisions, and quality control points in a standardized pre-analytical workflow for proteomic biomarker discovery.
In conclusion, the fidelity of a biomarker discovery pipeline is fundamentally rooted in the rigor of its pre-analytical phase. By systematically standardizing blood collection, processing, and storage protocols, and by integrating a multi-layered quality control strategy that includes monitoring key confounders and using standardized QC materials, researchers can significantly reduce technical noise. This disciplined approach ensures that the biological signal of interest, rather than pre-analytical artifact, drives discovery, thereby accelerating the development of reliable, clinically translatable biomarkers.
Mass Spectrometry Platforms and Acquisition Modes
Mass spectrometry (MS) platforms are defined by how key instrument components are configured and operated. Core components include the ion source (converts molecules to ions), mass analyzer(s) (separates ions by mass-to-charge ratio, m/z), collision cell (fragments ions), and detector (quantifies ions) [26]. The combination of scan modes used in these components defines the data acquisition strategy, primarily categorized into untargeted and targeted approaches [26].
Untargeted Acquisition Modes
Data-Dependent Acquisition (DDA) is a foundational untargeted strategy. The instrument first performs a full MS1 scan to detect all ions, then automatically selects the most abundant precursor ions for MS/MS fragmentation [26]. DDA provides high-resolution, clean MS2 spectra but is biased toward high-intensity ions and can exhibit poor reproducibility across replicates [26].
Data-Independent Acquisition (DIA) was designed to enhance reproducibility. It systematically divides the full m/z range into consecutive windows. All precursors within each window are fragmented simultaneously, providing comprehensive MS2 data for nearly all detectable ions independent of intensity [26]. DIA offers excellent reproducibility and sensitivity for low-abundance analytes but produces complex data that requires advanced deconvolution algorithms [26].
Targeted Acquisition Modes
Multiple Reaction Monitoring (MRM), performed on triple quadrupole instruments, is the gold standard for targeted quantification. It uses predefined precursor-to-product ion transitions (MRM transitions) for highly selective and sensitive detection of known compounds [26]. MRM delivers unmatched specificity and linearity but requires significant upfront method development and is limited to known targets [26].
Parallel Reaction Monitoring (PRM) is a high-resolution targeted mode. It combines MRM-like specificity with the collection of full, high-resolution fragment ion spectra, providing rich spectral information for confident identification and quantification [27].
Table 1: Comparison of Key Mass Spectrometry Acquisition Modes
| Feature | DDA (Untargeted) | DIA (Untargeted) | MRM (Targeted) | PRM (Targeted) |
|---|---|---|---|---|
| Primary Goal | Discovery, identification | Comprehensive profiling, quantification | Precise, sensitive quantification | High-resolution targeted quantification |
| Scan Mode | Full scan (MS1), then targeted MS/MS on intense ions | Sequential full MS/MS on all ions in defined m/z windows | Selective monitoring of predefined precursor/fragment pairs | Selective MS2 with full fragment scan |
| Multiplexing | Limited by dynamic exclusion | High, all analytes in windows | High for known transitions | Moderate |
| Reproducibility | Moderate (ion intensity bias) | High (systematic acquisition) | Very High | Very High |
| Ideal For | Novel biomarker discovery, spectral library generation | Large-scale quantitative studies, biomarker verification | Validated biomarker assays, clinical diagnostics | Biomarker validation, PTM analysis |
| Key Limitation | Bias against low-abundance ions | Complex data deconvolution | Limited to known targets; requires method development | Lower throughput than MRM |
Experimental Workflows in Biomarker Research
A coherent pipeline connecting biomarker discovery with established evaluation and validation is critical for developing robust, clinically relevant assays [28]. This pipeline integrates both untargeted and targeted MS approaches.
Figure 1: Integrated biomarker discovery and validation pipeline.
Sample Preparation
Robust sample preparation is essential for clinical proteomics. Common biofluids include blood (plasma/serum), urine, and cerebrospinal fluid (CSF) [19]. Proteins are typically denatured, reduced, alkylated, and digested with trypsin into peptides for LC-MS/MS analysis [19]. Depletion of high-abundance proteins or enrichment of target analytes is often necessary to detect lower-abundance cancer biomarkers, especially in plasma and serum [29]. For formalin-fixed paraffin-embedded (FFPE) tissues, reversal of chemical cross-linking is required prior to digestion [19].
Untargeted Discovery Workflow
- LC-MS/MS Analysis: Digested peptides are separated by liquid chromatography and analyzed using DDA or DIA on high-resolution mass spectrometers (e.g., Q-TOF, Orbitrap) [19].
- Database Searching: MS/MS spectra are searched against protein sequence databases using algorithms (e.g., Sequest, Mascot, X!Tandem) to identify peptide sequences [28].
- Bioinformatics Validation: Identified peptides are rigorously validated. This includes:
- Concordance Analysis: Using multiple database search algorithms to increase confidence in peptide identifications [28].
- Uniqueness Check: Using tools like BLAST to ensure peptide biomarkers are unique to the organism or disease of interest and absent in related species [28].
- False Discovery Rate (FDR) Estimation: Using target-decoy search strategies to measure and control for incorrect peptide assignments [28].
Targeted Verification and Validation Workflow
- Assay Development: Proteotypic peptides representing candidate biomarkers are selected. For MRM, optimal precursor-fragment ion transitions are determined experimentally [29] [27].
- Absolute Quantification: Stable Isotope-labeled Standard (SIS) peptides are added to the sample at a known concentration [29] [27]. These "heavy" peptides have identical physicochemical properties to their endogenous "light" counterparts but are distinguishable by MS. Quantification is based on the light-to-heavy peptide intensity ratio [27].
- LC-MRM/PRM Analysis: Samples are analyzed using targeted MS on triple quadrupole (for MRM) or high-resolution (for PRM) instruments [29].
Figure 2: Targeted proteomics workflow with isotope dilution.
Detailed Experimental Protocols
Protocol for Untargeted Profiling using DIA (SWATH-MS)
This protocol is adapted for biomarker discovery from biofluids using a high-resolution Q-TOF mass spectrometer [19].
I. Sample Preparation
- Plasma/Serum Depletion: Use an immunoaffinity column to remove the top 14 abundant proteins from 20 µL of plasma/serum.
- Protein Digestion:
- Reduce proteins with 10 mM dithiothreitol (56°C, 30 min).
- Alkylate with 25 mM iodoacetamide (room temperature, 30 min in the dark).
- Digest with sequencing-grade trypsin (1:20 enzyme-to-protein ratio, 37°C, overnight).
- Desalt peptides using C18 solid-phase extraction cartridges and dry in a vacuum concentrator.
II. Liquid Chromatography
- Column: C18 reversed-phase column (75 µm i.d. x 25 cm length, 1.6 µm particle size).
- Gradient: 2-35% mobile phase B (0.1% formic acid in acetonitrile) over 120 minutes at a flow rate of 300 nL/min.
III. Data-Independent Acquisition (DIA) on Q-TOF Mass Spectrometer
- MS1 Survey Scan: Acquire one full-scan MS1 spectrum (m/z 350-1400, 250 ms accumulation time).
- DIA MS/MS Scans: Cycle through 64 variable windows covering the m/z 400-1200 range.
- Fragmentation: Use collision energy rolling based on precursor m/z.
- Resolution: Ensure MS2 fragments are acquired with a resolution of at least 30,000.
- Quality Control: Inject a pooled quality control sample every 6-8 experimental samples to monitor instrument performance.
IV. Data Processing
- Process DIA data using specialized software (e.g., Spectronaut, DIA-NN, or Skyline).
- Use a project-specific or public spectral library (e.g., from DDA runs of sample aliquots) to extract and quantify peptide intensities.
- Perform statistical analysis (e.g., t-tests, ANOVA) to identify significantly differentially expressed proteins between case and control groups.
Protocol for Targeted Verification using LC-MRM/MS
This protocol is for verifying a panel of candidate protein biomarkers in plasma [29] [27].
I. Sample Preparation with SIS Peptides
- Follow steps in Section 3.1.I for plasma depletion and digestion.
- Internal Standard Addition: After digestion, add a known amount (e.g., 25-100 fmol) of stable isotope-labeled (SIS) peptides to each sample digest. SIS peptides are spiked in prior to LC-MS analysis.
II. Liquid Chromatography
- Use the same LC conditions as in Section 3.1.II, but the gradient can be shortened to 30-60 minutes for higher throughput.
III. Multiple Reaction Monitoring (MRM) on Triple Quadrupole Mass Spectrometer
- Method Development: For each target peptide, define the precursor ion (m/z) and at least three specific fragment ions. The most intense transition is the quantifier, and the others are qualifiers.
- Chromatographic Method: Schedule MRM transitions within a specific retention time window (e.g., 3-5 minutes wide) to maximize the number of data points per peak and monitor more peptides.
- MS Parameters:
- Dwell time: 10-50 ms per transition.
- Collision energy: Optimized for each peptide.
- Resolution: Unit resolution for both Q1 and Q3.
IV. Data Analysis and Quantification
- Peak Integration: Manually review and integrate peaks for both endogenous ("light") and SIS ("heavy") peptides for all transitions.
- Calculate Ratios: For each peptide, calculate the peak area ratio of light to heavy.
- Determine Concentration: Calculate the absolute concentration of the endogenous peptide using the known concentration of the spiked SIS peptide and the light/heavy ratio.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Proteomic Mass Spectrometry
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Stable Isotope-Labeled Standard (SIS) Peptides | Internal standards for absolute quantification; correct for analytical variability [29] [27]. | Synthesized with 13C/15N on C-terminal Lys/Arg; spiked into sample post-digestion. |
| Trypsin (Sequencing Grade) | Proteolytic enzyme; cleaves proteins at lysine and arginine residues to generate peptides for MS analysis [19]. | Use 1:20-1:50 enzyme-to-protein ratio; ensure purity to minimize autolysis peaks. |
| Immunoaffinity Depletion Columns | Remove high-abundance proteins (e.g., albumin, IgG) from plasma/serum to enhance detection of low-abundance biomarkers [29]. | Critical for plasma/serum analysis; can deplete top 7-14 proteins. |
| C18 Solid-Phase Extraction (SPE) Tips/Cartridges | Desalt and concentrate peptide mixtures after digestion; remove interfering salts and detergents [19]. | Standard step before LC-MS/MS; improves chromatographic performance and signal. |
| Formic Acid | Ion-pairing agent in mobile phase; improves chromatographic peak shape and ionization efficiency in positive ESI mode [19]. | Used at 0.1% in water (mobile phase A) and acetonitrile (mobile phase B). |
| Dithiothreitol (DTT) & Iodoacetamide (IAA) | Reduce disulfide bonds (DTT) and alkylate cysteine residues (IAA); denatures proteins and prevents disulfide bond reformation [19]. | Standard step in "bottom-up" proteomics workflow. |
The Proteomic Workflow in Action: From Sample to Spectral Data
In mass spectrometry (MS)-based proteomics, the profound complexity and vast dynamic range of protein concentrations in biological samples present a significant analytical challenge. Sample preparation, particularly through depletion, enrichment, and fractionation, is therefore not merely a preliminary step but a critical determinant for the success of downstream analyses, especially in biomarker discovery pipelines [30] [31]. Effective sample preparation mitigates the dynamic range issue, reduces complexity, and enhances the detection of lower-abundance proteins, which are often the most biologically interesting candidates for disease biomarkers [28] [31]. This application note details standardized protocols and strategic frameworks for preparing proteomic samples, providing researchers with the tools to deepen proteome coverage and improve the robustness of their identifications and quantifications.
Core Principles and Strategic Framework
The primary goal of sample preparation is to simplify complex protein or peptide mixtures to facilitate more comprehensive MS analysis. The strategies can be conceptualized in a hierarchical manner:
- Depletion: The selective removal of a small number of highly abundant proteins (e.g., albumin, immunoglobulins from plasma) that otherwise dominate the MS signal [31]. This is often the first step when analyzing biofluids.
- Enrichment: The affirmative selection and concentration of specific protein subsets, such as those with post-translational modifications (e.g., phosphorylation) or low molecular weight (LMW) proteins, from a complex background [32] [33].
- Fractionation: The separation of a complex mixture into simpler, less complex sub-fractions based on properties like isoelectric point (pI), hydrophobicity, or molecular weight. This can be applied at the protein or peptide level and is often performed after digestion [28] [34].
The following workflow diagram illustrates how these strategies integrate into a coherent proteomic analysis pipeline for biomarker discovery.
Detailed Experimental Protocols
Protocol 1: Immunoaffinity Depletion of High-Abundance Plasma Proteins
This protocol describes the use of a Multiple Affinity Removal System (MARS) column to deplete the top 7 or 14 most abundant proteins from human plasma, thereby enhancing the detection of medium- and low-abundance proteins [31].
Materials:
- MARS-7 or MARS-14 column (Agilent)
- HPLC system with UV detection
- Load/wash buffer and elution buffer (supplied with column)
- Amicon 5 kDa molecular weight cutoff filters (Millipore)
- BCA protein assay kit (Pierce)
Method:
- Sample Preparation: Dilute plasma fourfold with the specified load/wash buffer. Remove particulates by centrifuging the diluted plasma through a 0.22 µm spin filter for 1 minute at 16,000 × g.
- Column Equilibration: Equilibrate the MARS column with load/wash buffer at room temperature.
- Sample Loading: Load 160 µL of the diluted, filtered plasma onto the column at a low flow rate (0.125 mL/min for MARS-14, 0.5 mL/min for MARS-7).
- Fraction Collection:
- Collect the flow-through fraction, which contains the depleted plasma, and store at -20°C.
- Use elution buffer to release the bound fraction containing the abundant proteins.
- Buffer Exchange and Concentration: Concentrate the depleted plasma fraction using a 5 kDa MWCO filter and exchange the buffer to 50 mM ammonium bicarbonate.
- Protein Quantification: Determine the protein concentration of the depleted sample using the BCA assay.
Performance Notes: This depletion process is highly reproducible and results in an average 2 to 4-fold global enrichment of non-targeted proteins. However, even after depletion, the 50 most abundant proteins may still account for ~90% of the total MS signal, underscoring the need for subsequent fractionation or enrichment steps for deep proteome mining [31].
Protocol 2: Automated In-Solution Digestion for High-Throughput Analysis
This protocol is designed for robust, high-throughput sample preparation without depletion or pre-fractionation, suitable for large-scale clinical cohorts [35]. It can be performed using an automated liquid-handling platform.
Materials:
- LH-1808 or equivalent liquid handling robot (AMTK)
- Tris(2-carboxyethyl)phosphine hydrochloride (TCEP)
- 2-Chloroacetamide (CAA)
- Sequencing-grade trypsin and LysC
- Trifluoroacetic acid (TFA)
- Home-made C18 spintips (3M Empore C18 material)
Method:
- Dilution & Denaturation: Transfer 5 µL of plasma into a 96-well plate. Add 95 µL of reduction-alkylation buffer (10 mM TCEP, 50 mM CAA, 50 mM Tris-HCl, pH 8). Mix thoroughly by pipetting.
- Aliquot & Heat Denature: Transfer a 20 µL aliquot of the diluted plasma to a new plate. Heat at 95°C for 15 minutes to denature proteins, then cool to room temperature.
- Enzymatic Digestion: Add a mixture of Lys-C and trypsin (1:100 enzyme-to-protein ratio, 0.6 µg of each enzyme). Incubate the plate at 37°C for 3 hours.
- Reaction Quenching: Quench the digestion by adding 50 µL of 0.1% (v/v) TFA.
- Peptide Cleanup: Desalt the digested peptides using home-made C18 spintips. Lyophilize the eluted peptides for storage or resuspend in 0.1% formic acid for LC-MS analysis.
Performance Notes: This automated workflow achieves a median coefficient of variation (CV) of 9% for label-free quantification and identifies over 300 proteins from 1 µL of plasma without depletion, making it ideal for high-throughput biomarker verification studies [35].
Protocol 3: Micro-Purification and Enrichment Using StageTips
StageTips are low-cost, disposable pipette tips containing disks of chromatographic media for micro-purification, enrichment, and pre-fractionation of peptides [36].
Materials:
- Pipette tips (200 µL)
- Teflon mesh-embedded disks (C18, cation-exchange, anion-exchange, TiO₂, ZrO₂)
- Solvents: 0.1% TFA, 0.1% Formic Acid, LC-MS grade water and acetonitrile
Method (C18 Desalting and Concentration):
- Conditioning: Pass 100 µL of methanol through the C18 StageTip by centrifugation.
- Equilibration: Wash with 100 µL of solvent B (80% acetonitrile, 0.1% TFA), followed by 100 µL of solvent A (0.1% TFA).
- Sample Loading: Acidify the peptide sample and load it onto the StageTip slowly by centrifugation.
- Washing: Wash with 100 µL of solvent A to remove salts and contaminants.
- Elution: Elute peptides with 50-100 µL of solvent B into a clean tube. Evaporate the solvent in a vacuum concentrator.
Performance Notes: StageTips can be configured with multiple disks for multi-functional applications. For example, combining TiO₂ disks with C18 material enables efficient phosphopeptide enrichment. The entire process for desalting takes ~5 minutes, while fractionation or enrichment requires ~30 minutes [36].
Research Reagent Solutions
The following table catalogues essential reagents and tools for implementing the described strategies.
Table 1: Key Research Reagent Solutions for Proteomic Sample Preparation
| Item | Function/Description | Example Application |
|---|---|---|
| MARS Column (Agilent) | Immunoaffinity column for depletion of top 7 or 14 abundant plasma proteins. | Deep plasma proteome profiling prior to discovery LC-MS/MS [31]. |
| PreOmics iST Kit | Integrated workflow for lysis, digestion, and peptide purification in a single device. | Standardized, high-throughput sample preparation for cell and tissue lysates [37]. |
| StageTip Disks (C18, TiO₂, etc.) | Self-made micro-columns for peptide desalting, fractionation, and specific enrichment. | Desalting peptide digests; enriching phosphopeptides with TiO₂ disks [36]. |
| Rapigest SF | Acid-labile surfactant for protein denaturation; cleaved under acidic conditions to prevent MS interference. | Efficient protein solubilization and digestion without detergent-related ion suppression [38]. |
| Tris(2-carboxyethyl)phosphine (TCEP) | MS-compatible reducing agent for breaking protein disulfide bonds. | Protein reduction under denaturing conditions as part of the digestion protocol [38] [35]. |
| Tryptsin/Lys-C Mix | Proteolytic enzymes for specific protein digestion into peptides. | High-efficiency, in-solution digestion of complex protein mixtures [35] [34]. |
Quantitative Comparison of Method Performance
The selection of a sample preparation strategy involves trade-offs between depth of analysis, throughput, and reproducibility. The following table summarizes quantitative data from the cited studies to aid in method selection.
Table 2: Performance Metrics of Different Sample Preparation Strategies
| Strategy / Workflow | Proteins Identified (Single Run) | Quantitative Reproducibility (Median CV) | Sample Processing Time | Key Applications |
|---|---|---|---|---|
| Immunodepletion (MARS-14) [31] | ~25% increase vs. undepleted plasma (Shotgun MS) | -- | ~40 min/sample (depletion only) | Enhancing detection of medium-abundance proteins in plasma. |
| Automated In-Solution Digestion [35] | >300 proteins (from 1 µL plasma) | 9% | High-throughput, 32 samples simultaneously | Large-scale clinical cohort verification studies. |
| SISPROT with 2D Fractionation [35] | 862 protein groups (from 1 µL plasma) | -- | Longer, includes fractionation | Deep discovery profiling from minimal sample input. |
| StageTip Desalting [36] | -- | -- | ~5 minutes | Routine peptide cleanup and concentration for any workflow. |
Integrated Workflow for Biomarker Discovery
The individual strategies of depletion, enrichment, and fractionation find their greatest utility when combined into a coherent pipeline. This is particularly true for biomarker discovery, which progresses from comprehensive discovery to targeted validation. The following diagram outlines an integrated workflow that connects sample preparation strategies with the phases of biomarker development.
This integrated approach ensures that the sample preparation methodology is tailored to the specific goal. The discovery phase leverages extensive fractionation and enrichment to maximize proteome coverage and identify potential biomarker candidates. In contrast, the validation phase prioritizes robustness, reproducibility, and high throughput to confidently assess candidate performance across large patient cohorts [28] [38] [35].
Mass spectrometry (MS)-based proteomics has become an indispensable tool in biomedical research for the discovery and validation of protein biomarkers [19] [39]. The identification of reliable biomarkers is crucial for early disease detection, prognosis, and monitoring treatment responses [40]. The core of this process lies in the analytical techniques used to acquire proteomic data, with Data-Dependent Acquisition (DDA), Data-Independent Acquisition (DIA), and tandem mass tag (TMT)/isobaric Tags for Relative and Absolute Quantitation (iTRAQ) labeling emerging as the three principal methods [41] [42]. Each technique offers distinct advantages and limitations in terms of quantification accuracy, proteome coverage, and suitability for different experimental designs within the biomarker discovery pipeline [43] [41]. This article provides a detailed comparison of these core acquisition techniques and presents standardized protocols for their application in clinical and research settings focused on biomarker identification.
Core Principles of MS Acquisition Techniques
Data-Dependent Acquisition (DDA), often used in label-free quantification, operates by selecting the most abundant peptide precursor ions from an MS1 survey scan for subsequent fragmentation and MS2 analysis [41] [42]. This intensity-based selection provides high-quality spectra for protein identification but can introduce stochastic sampling variability and miss lower-abundance peptides, potentially limiting proteome coverage [41] [19].
Data-Independent Acquisition (DIA) addresses this limitation through a systematic approach where the entire mass range is divided into consecutive isolation windows, and all precursors within each window are fragmented simultaneously [43] [42]. This comprehensive fragmentation strategy reduces missing values and improves quantitative precision, making it particularly valuable for analyzing complex clinical samples where consistency across many samples is crucial [43] [19].
TMT/iTRAQ Labeling utilizes isobaric chemical tags that covalently bind to peptide N-termini and lysine side chains [41] [44]. These tags have identical total mass but release reporter ions of different masses upon fragmentation, enabling multiplexed quantification of multiple samples in a single MS run [41] [44]. The isobaric nature means peptides from different samples appear as a single peak in MS1 but can be distinguished based on their reporter ion intensities in MS2 or MS3 spectra [42] [44].
Comparative Performance in Biomarker Research
Table 1: Comprehensive Comparison of Core MS Acquisition Techniques for Biomarker Discovery
| Parameter | DDA (Label-Free) | DIA | TMT/iTRAQ |
|---|---|---|---|
| Quantification Principle | Peak intensity or spectral counting [42] | Extraction of fragment ion chromatograms [42] | Reporter ion intensities [41] |
| Multiplexing Capacity | Low (individual analysis) [41] | Low (individual analysis) [41] | High (up to 18 samples simultaneously) [42] |
| Proteome Coverage & Missing Values | Moderate, higher missing values [42] | High, fewer missing values [43] [42] | High with fractionation [42] |
| Quantitative Accuracy & Precision | Moderate, susceptible to instrument variation [41] | High, particularly with library-free approaches [43] | High intra-experiment precision [41] |
| Dynamic Range | Broader linear dynamic range [42] | Not specified in sources | Limited by ratio compression [42] |
| Cost & Throughput | Cost-effective for large cohorts [42] | Cost-effective, reduced sample prep [43] | Higher reagent costs, medium throughput [43] [42] |
| Key Advantages | Experimental flexibility, no labeling cost [41] [42] | Comprehensive data recording, high reproducibility [43] [42] | High quantification accuracy, reduced technical variability [43] [41] |
| Key Limitations | Higher missing values, requires strict instrument stability [41] [42] | Complex data analysis [41] [42] | Ratio compression effects, batch effects [42] |
The selection of an appropriate acquisition technique significantly impacts the depth and quality of data obtained in biomarker discovery. DIA, particularly in library-free mode using software such as DIA-NN, has demonstrated performance comparable to TMT-DDA in detecting target engagement in thermal proteome profiling experiments, making it a cost-effective alternative [43]. TMT methods excel in multiplexing capacity, allowing up to 18 samples to be analyzed simultaneously, thereby reducing technical variability [42]. However, they suffer from ratio compression effects that can underestimate true quantification differences [42]. Label-free DDA provides maximum experimental flexibility and is suitable for large-scale studies, though it typically yields higher missing values and requires stringent instrument stability [41] [42].
Experimental Protocols
Protocol for DIA-Based Biomarker Screening
Sample Preparation and Liquid Chromatography
- Protein Extraction and Digestion: Extract proteins from biological samples (e.g., cell lysates, tissue, plasma) using appropriate lysis buffers. Digest proteins into peptides using trypsin following standard protocols [43] [40].
- Peptide Cleanup: Desalt peptides using C18 solid-phase extraction cartridges or stage tips.
- Liquid Chromatography: Separate peptides using nano-flow liquid chromatography with a reversed-phase C18 column and a gradient of 60-120 minutes, depending on desired depth of analysis [19].
Mass Spectrometry Data Acquisition
- MS Instrument Setup: Utilize a high-resolution mass spectrometer (e.g., Q-TOF, Orbitrap) capable of DIA acquisition.
- DIA Method Configuration: Divide the typical m/z range (e.g., 400-1000) into consecutive isolation windows. Window size can be fixed (e.g., 25 m/z) or variable, with narrower windows in crowded regions [43] [42].
- Cycling Method: Implement a cycle consisting of one MS1 scan followed by MS2 scans of all isolation windows. Adjust cycle time to ensure sufficient points across chromatographic peaks [42].
Data Processing and Analysis
- Library Generation: Generate a spectral library using either:
- Peptide Identification and Quantification: Match DIA data against the spectral library to identify peptides and extract fragment ion chromatograms for quantification [43] [42].
- Statistical Analysis: Process quantitative data using bioinformatics tools to identify differentially expressed proteins with statistical significance.
Protocol for TMT/iTRAQ-Based Biomarker Verification
Sample Labeling and Pooling
- Peptide Labeling: Reconstitute desalted peptides from each sample in 50 mM HEPES buffer (pH 8.5). Dissolve TMT or iTRAQ reagents in anhydrous acetonitrile and add to respective peptide samples. Incubate at room temperature for 1-2 hours [41] [44].
- Reaction Quenching: Add 5% hydroxylamine to stop the labeling reaction and incubate for 15 minutes.
- Sample Pooling: Combine equal amounts of each labeled sample into a single tube. Vacuum centrifuge to reduce volume if necessary [42] [44].
Fractionation and Mass Spectrometry
- Peptide Fractionation: Perform high-pH reversed-phase fractionation to reduce sample complexity. Use a C18 column with a stepwise or shallow gradient of acetonitrile in ammonium hydroxide (pH 10) to collect 8-16 fractions [42].
- LC-MS/MS Analysis: Reconstitute each fraction in loading solvent and analyze using nano-LC-MS/MS with a DDA method.
- MS Method: Acquire MS1 spectra at high resolution (e.g., 60,000-120,000). Select top N most intense precursors for HCD fragmentation. Set HCD collision energy to optimize reporter ion generation [44].
Data Analysis
- Database Searching: Search raw files against appropriate protein sequence databases using search engines such as Mascot, SEQUEST, or Andromeda [12] [45].
- Reporter Ion Quantification: Extract reporter ion intensities from MS2 or MS3 spectra. Apply isotope correction factors as recommended by reagent manufacturers [44].
- Normalization and Statistical Analysis: Normalize data across channels and perform statistical tests to identify significantly altered proteins between sample groups.
The Scientist's Toolkit
Essential Research Reagent Solutions
Table 2: Key Research Reagents and Materials for MS-Based Biomarker Studies
| Reagent/Material | Function | Application Notes |
|---|---|---|
| TMTpro 18-plex | Multiplexed peptide labeling for quantitative comparison of up to 18 samples [42] | Enables two conditions with 9 temperature points in single TPP experiment; reduces batch effects [43] |
| iTRAQ 8-plex | Isobaric labeling for 8-plex quantitative experiments [41] | Suitable for smaller multiplexing needs; similar chemistry to TMT [41] |
| Trypsin (Sequencing Grade) | Proteolytic digestion of proteins into peptides for MS analysis [19] | Standard enzyme for bottom-up proteomics; specific cleavage C-terminal to Arg and Lys [19] |
| C18 Solid-Phase Extraction Cartridges | Desalting and cleanup of peptides prior to LC-MS | Removes contaminants, improves MS signal; available in various formats [40] |
| High-pH Reversed-Phase Columns | Peptide fractionation to reduce sample complexity | Increases proteome coverage; essential for deep profiling with TMT [42] |
| Lysis Buffers (RIPA, UA) | Protein extraction from cells and tissues | Composition varies by sample type; may include protease inhibitors [40] |
Bioinformatics Tools for Data Analysis
The analysis of proteomics data requires specialized bioinformatics tools that vary by acquisition method [12]. For DDA data, search engines such as MaxQuant (with Andromeda), Mascot, and SEQUEST are widely used for peptide identification and quantification [12] [45]. DIA data analysis employs specialized tools like DIA-NN (particularly effective in library-free mode), Spectronaut (with DirectDIA), and Skyline [43] [12]. For TMT/iTRAQ data, tools such as IsobaricAnalyzer (within OpenMS) and MSstats enable robust quantification and statistical analysis [44]. Protein inference and downstream analysis can be performed using Perseus, which provides comprehensive tools for statistical analysis, visualization, and interpretation of proteomics data [12].
The selection of appropriate MS acquisition techniques is pivotal for successful biomarker discovery and verification. DIA approaches, particularly library-free methods using DIA-NN, offer a cost-effective alternative to TMT-DDA with comparable performance in detecting target engagement, as demonstrated in thermal proteome profiling studies [43]. TMT/iTRAQ labeling provides excellent multiplexing capacity and precision for medium-scale studies, despite challenges with ratio compression [42]. Label-free DDA remains valuable for large-scale studies where experimental flexibility is paramount [41]. Understanding the strengths and limitations of each technique enables researchers to design optimal proteomics workflows for biomarker pipeline development, ultimately advancing clinical applications in disease diagnosis, prognosis, and treatment monitoring.
Data-Independent Acquisition (DIA) for Deep, Unbiased Proteome Profiling
Data-Independent Acquisition (DIA) has emerged as a transformative mass spectrometry (MS) strategy for deep, unbiased proteome profiling, positioning itself as a cornerstone technology in modern biomarker discovery pipelines. Unlike traditional Data-Dependent Acquisition (DDA) methods that stochastically select abundant precursors for fragmentation, DIA systematically fragments all detectable ions within predefined mass-to-charge (m/z) windows across the entire chromatographic run [46] [47]. This fundamental shift in acquisition strategy enables comprehensive recording of fragment ion data for all eluting peptides, substantially mitigating the issue of missing values that frequently plagues large-scale cohort studies using DDA approaches [46] [48].
The application of DIA within clinical proteomics and biomarker research represents a paradigm shift, offering unprecedented capabilities for generating reproducible, high-quality quantitative data across complex sample sets. DIA's ability to provide continuous fragment ion data across all acquired samples ensures that valuable information is never irretrievably lost, allowing retrospective re-analysis of datasets as new hypotheses emerge or improved computational tools become available [46] [47]. This characteristic is particularly valuable in biomarker discovery, where precious clinical samples can be comprehensively profiled once, with the resulting data repositories serving as enduring resources for future investigations. The technology's enhanced quantitative accuracy, precision, and reproducibility compared to traditional methods make it ideally suited for identifying subtle but biologically significant protein abundance changes that often characterize disease states or therapeutic responses [46] [49].
DIA vs. DDA: A Comparative Analysis
Fundamental Technical Differences
The distinction between DIA and DDA represents more than a mere technical variation in mass spectrometry operation; it constitutes a fundamental difference in philosophy toward proteome measurement. In DDA, the mass spectrometer operates in a target-discard mode, first performing a survey scan (MS1) to identify the most intense peptide ions, then selectively isolating and fragmenting a limited number of these "top N" precursors (typically 10-15) for subsequent MS2 analysis [46] [47]. This approach generates relatively simple, interpretable MS2 spectra but introduces substantial stochastic sampling bias, as low-abundance peptides consistently fail to trigger fragmentation events, leading to significant missing data across sample replicates [48].
In contrast, DIA employs a comprehensive fragmentation strategy that eliminates precursor selection bias. Instead of selecting specific ions, DIA methods sequentially isolate and fragment all precursor ions within consecutive, predefined m/z windows (typically ranging from 4-25 Th) covering the entire mass range of interest [46] [49]. Early implementations like MSE and all-ion fragmentation (AIF) fragmented all ions simultaneously, while more advanced techniques including SWATH-MS and overlapping window methods fragment ions within sequential isolation windows [46]. This systematic approach ensures that fragment ion data is captured for all eluting peptides regardless of abundance, though it generates highly complex, chimeric MS2 spectra where fragment ions from multiple co-eluting precursors are intermixed [46] [47]. The deconvolution of these complex spectra requires sophisticated computational approaches and typically relies on spectral libraries, though library-free methods are increasingly viable [46] [50].
Performance Comparison in Proteomic Profiling
Table 1: Comparative Performance of DIA versus DDA in Proteomic Profiling
| Performance Metric | Data-Independent Acquisition (DIA) | Data-Dependent Acquisition (DDA) |
|---|---|---|
| Proteome Coverage | 10,000+ protein groups (mouse liver) [48] | 2,500-3,600 protein groups (mouse liver) [48] |
| Quantitative Reproducibility | ~93% data matrix completeness [48] | ~69% data matrix completeness [48] |
| Missing Values | Greatly reduced; minimal missing values across samples [46] | Significant missing values due to stochastic sampling [46] |
| Dynamic Range | Extended by at least an order of magnitude [48] | Limited coverage of low-abundance proteins [48] |
| Quantitative Precision | High quantitative accuracy and precision [46] | Moderate quantitative precision [47] |
| Acquisition Bias | Unbiased; all peptides fragmented regardless of abundance [47] | Biased toward most abundant precursors [47] |
| Data Complexity | Highly complex, chimeric MS2 spectra [46] | Simpler, cleaner MS2 spectra [47] |
| Computational Demand | High; requires specialized software [50] [47] | Moderate; established analysis pipelines [47] |
The practical implications of these technical differences become evident when examining experimental data. In a direct comparison using mouse liver tissue analyzed on the Orbitrap Astral platform, DIA identified over 10,000 protein groups compared to only 2,500-3,600 with DDA methods [48]. More significantly, the quantitative data matrix generated by DIA demonstrated 93% completeness across replicates, dramatically higher than the 69% achieved with DDA [48]. This enhanced reproducibility stems from DIA's systematic acquisition scheme, which ensures consistent measurement of the same peptides across all runs in a cohort study.
For biomarker discovery applications, DIA's extended dynamic range proves particularly valuable. The technology identifies and quantifies more than twice as many peptides (~45,000 versus ~20,000 in the mouse liver study), with the additional identifications primarily deriving from low-abundance proteins that frequently include biologically relevant regulators and potential disease biomarkers [48]. The histogram of protein abundance distributions clearly shows DIA's enhanced capability to detect proteins across a wider concentration range, extending coverage by at least an order of magnitude into the low-abundance proteome [48].
DIA Experimental Workflow for Biomarker Discovery
Comprehensive Biomarker Pipeline Using DIA
Diagram 1: End-to-end biomarker discovery pipeline using DIA mass spectrometry. The workflow integrates sample preparation, data acquisition, computational analysis, and analytical validation stages.
The application of DIA within a biomarker discovery pipeline follows a structured workflow that integrates wet-lab procedures with sophisticated computational analysis. As illustrated in Diagram 1, the process begins with rigorous sample preparation using standardized protocols for protein extraction, digestion, and cleanup to minimize technical variability [51]. Following quality control measures to ensure sample integrity, the critical decision point involves spectral library selection, where researchers can choose between project-specific libraries generated via DDA, publicly available resources (PeptideAtlas, MassIVE-KB, ProteomeXchange), or predicted libraries generated in silico [46] [52]. For clinical applications where project-specific libraries may be impractical due to sample limitations, predicted libraries enable unbiased and reproducible analysis [46].
The DIA LC-MS/MS acquisition follows, with modern high-resolution instruments like the Orbitrap Astral or timsTOF systems providing the speed and sensitivity required for deep proteome coverage [46] [48]. Following data acquisition, computational extraction and quantification of peptide signals using tools like DIA-NN or Spectronaut transforms raw data into peptide-level measurements [50]. Statistical analysis identifies differentially expressed proteins, with biomarker candidates subsequently undergoing rigorous analytical validation using tools like the Targeted Extraction Assessment of Quantification (TEAQ) to evaluate linearity, specificity, repeatability, and reproducibility against clinical-grade standards [8]. Promising candidates then transition to targeted mass spectrometry methods (PRM, MRM) for high-throughput verification in expanded clinical cohorts [8] [49].
Key Software Tools for DIA Data Analysis
Table 2: Essential Computational Tools for DIA Data Analysis in Biomarker Research
| Software Tool | Primary Function | Key Features | Application in Biomarker Pipeline |
|---|---|---|---|
| DIA-NN [50] | DIA data processing | Deep neural networks, library-free capability, high sensitivity | Primary analysis for peptide identification and quantification |
| Skyline [51] | Targeted mass spectrometry | Method development, data visualization, result validation | Transitioning biomarker candidates to targeted assays |
| TEAQ [8] | Analytical validation | Assesses linearity, specificity, reproducibility | Selecting clinically viable biomarker candidates |
| FragPipe/MSFragger [50] | DDA library generation | Ultra-fast database searching, spectral library building | Generating project-specific spectral libraries |
| ProteomeXchange [52] | Data repository | Public data deposition, dataset discovery | Accessing public spectral libraries and validation datasets |
The computational ecosystem supporting DIA analysis has matured substantially, with specialized tools addressing each stage of the biomarker discovery workflow. DIA-NN has emerged as a gold-standard tool leveraging deep neural networks for precise identification and quantification, particularly effective for processing complex DIA datasets [50]. Its capability for library-free analysis enables applications where project-specific spectral libraries are impractical. For the critical transition from discovery to validation, Skyline provides a comprehensive environment for developing targeted assays, while the recently developed TEAQ (Targeted Extraction Assessment of Quantification) software enables systematic evaluation of biomarker candidates against analytical performance criteria required for clinical applications [8].
The expanding availability of public data resources through ProteomeXchange consortium members (PRIDE, MassIVE, PeptideAtlas) provides essential infrastructure for biomarker research, offering access to spectral libraries, standardized datasets, and orthogonal validation resources [52]. These repositories have accumulated over 37,000 datasets, with nearly 70% publicly accessible, creating an extensive knowledge base for comparative analysis and validation [52]. The growing trend toward data sharing and reanalysis of public proteomics data further enhances the value of these resources for biomarker discovery [52].
Detailed Protocol: DIA Analysis Using DIA-NN
Spectral Library Preparation and Data Acquisition
This protocol provides a step-by-step workflow for analyzing DIA data using the DIA-NN software suite, optimized for biomarker discovery applications. The process begins with experimental design and sample preparation, where consistent protein extraction, digestion, and cleanup procedures are critical for minimizing technical variability. For clinical samples, incorporate appropriate sample randomization and blocking strategies to account for potential batch effects.
Spectral library generation represents a critical foundation for DIA analysis. Researchers can select from three primary approaches:
- Project-specific DDA libraries: Generate using deep fractionation or gas-phase fractionation of pooled samples, processed through FragPipe/MSFragger for rapid spectral searching [50].
- Public spectral libraries: Download organism-specific libraries from resources like PeptideAtlas (https://www.peptideatlas.org/) or MassIVE-KB (https://massive.ucsd.edu/) [52].
- Predicted libraries: Generate in silico using DIA-NN's built-in prediction algorithms, particularly valuable when sample material is limited for library generation [46] [50].
For predicted library generation in DIA-NN:
- Download the appropriate reference proteome (FASTA file) from UniProt (https://www.uniprot.org/proteomes/) [50].
- Load the FASTA file into DIA-NN and select both "FASTA digest for library-free search/library generation" and "Deep learning-based spectra, RTs and IMs prediction" under the Precursor ion generation section [50].
- Execute library generation; the resulting spectral library file can be reused for other experiments with similar acquisition settings.
For DIA data acquisition on high-resolution mass spectrometers:
- Implement variable window schemes optimized for your specific instrument platform to maximize peptide coverage [46].
- Set MS1 and MS2 resolution parameters to maximize sensitivity while maintaining acceptable cycle times (typically ~1.5-3 seconds) [48].
- For Orbitrap-based instruments, utilize overlapping window schemes when possible to enhance peptide identifications [46].
Data Processing and Statistical Analysis
Raw data processing in DIA-NN follows a structured workflow:
- Load acquired DIA data (.raw or .mzML format) into DIA-NN, requiring MSFileReader for Thermo Fisher raw file processing [50].
- Set Mass Accuracy and MS1 Accuracy to 0.0 ppm under Algorithm settings to enable auto-calibration [50].
- Adjust precursor and fragment mass range settings based on experimental parameters (typical m/z range: 300-1800) [50].
- Configure digestion specificity (Trypsin/P with 1-2 missed cleavages), peptide length (7-30 amino acids), and charge states (1-4+) according to experimental design [50].
- Enable appropriate variable modifications (e.g., Methionine oxidation, Cysteine carbamidomethylation) for comprehensive modification profiling [50].
- Activate "Match Between Runs" (MBR) to transfer identifications across samples, enhancing completeness of the data matrix, though this should be disabled for highly heterogeneous samples [50].
- Execute the analysis, generating primary output files including the main report (.tsv) and quantitative matrices.
Statistical analysis and biomarker candidate selection:
- Import DIA-NN output into R or Python environments for downstream processing.
- Perform data quality assessment using metrics including missing value distributions, coefficient of variation analyses, and principal component analysis to identify potential batch effects or outliers.
- Apply normalization procedures (typically median normalization or variance-stabilizing normalization) to correct for technical variation.
- Implement imputation strategies for missing values (e.g., minimum value imputation, k-nearest neighbors) with careful consideration of the missingness mechanism.
- Conduct differential expression analysis using linear models (limma) or mixed-effects models that incorporate relevant experimental factors.
- Generate diagnostic visualizations including volcano plots, heatmaps, and correlation matrices to contextualize results.
- Adjust for multiple testing using Benjamini-Hochberg false discovery rate (FDR) control, with significance thresholds typically set at FDR < 0.05.
- Apply the TEAQ algorithm to evaluate analytical performance of candidate biomarkers, assessing linearity, specificity, repeatability, and reproducibility to prioritize candidates for validation [8].
Table 3: Essential Research Reagents and Resources for DIA Biomarker Studies
| Category | Specific Items | Function and Application |
|---|---|---|
| Sample Preparation | Trypsin/Lys-C protease mixtures | Protein digestion for peptide generation |
| RapiGest, SDS, urea-based buffers | Protein extraction and denaturation | |
| C18 and SCX purification cartridges | Sample cleanup and fractionation | |
| Stable isotope-labeled standard (SIS) peptides | Absolute quantification internal standards | |
| Chromatography | C18 reverse-phase columns (25-50cm) | Nanoflow LC peptide separation |
| Mobile phase buffers (water/acetonitrile with formic acid) | LC-MS/MS solvent system | |
| Mass Spectrometry | High-resolution mass spectrometer (Orbitrap Astral, timsTOF, Q-TOF) | DIA data acquisition |
| Calibration solutions (ESI-L Low Concentration Tuning Mix) | Mass accuracy calibration | |
| Computational Resources | DIA-NN, Skyline, FragPipe software suites | Data processing and analysis |
| ProteomeXchange public repositories (PRIDE, MassIVE) | Data sharing and spectral libraries [52] | |
| UniProt, PeptideAtlas databases | Reference proteomes and spectral libraries [52] [50] |
Successful implementation of DIA biomarker studies requires careful selection of reagents and resources across the entire workflow. Sample preparation reagents must ensure efficient, reproducible protein extraction and digestion, with trypsin remaining the workhorse protease due to its well-characterized cleavage specificity and compatibility with MS analysis [51]. For absolute quantification applications, stable isotope-labeled standard (SIS) peptides provide essential internal standards for precise measurement [49].
Chromatographic consumables directly impact peptide separation quality, with 25-50cm C18 columns providing the resolving power necessary for complex clinical samples. The recent introduction of the Orbitrap Astral mass spectrometer represents a significant advancement, demonstrating approximately 3x improved proteome coverage compared to previous generation instruments [48]. This enhanced sensitivity proves particularly valuable for biomarker applications where detection of low-abundance proteins is often critical.
The computational ecosystem forms an equally essential component, with DIA-NN emerging as a leading solution for DIA data processing due to its robust performance and active development [50]. The expansion of public data resources through ProteomeXchange provides essential infrastructure for biomarker research, offering access to spectral libraries and validation datasets that enhance reproducibility and accelerate discovery [52].
Data-Independent Acquisition has fundamentally transformed the landscape of proteomic biomarker discovery, offering unprecedented capabilities for deep, reproducible profiling of clinical samples. The technology's systematic acquisition scheme addresses critical limitations of traditional DDA methods, particularly the problem of missing values that undermines statistical power in cohort studies [46] [48]. When integrated within a structured pipeline encompassing robust sample preparation, appropriate spectral library selection, sophisticated computational analysis, and rigorous analytical validation using tools like TEAQ, DIA enables translation of discovery findings into clinically viable biomarker candidates [8].
The continuing evolution of DIA technology—driven by advances in instrumentation, acquisition strategies, and computational tools—promises to further enhance its utility in biomarker research. Emerging trends including the use of predicted spectral libraries, library-free analysis methods, and integration with ion mobility separation are expanding applications in precision medicine and clinical proteomics [46]. As these developments mature and standardization efforts progress, DIA is positioned to become an increasingly central technology in the biomarker development pipeline, potentially enabling the discovery and validation of protein signatures for early disease detection, patient stratification, and therapeutic monitoring.
Mass spectrometry (MS)-based proteomics has become the cornerstone of large-scale, unbiased protein profiling, enabling transformative discoveries in biological research and biomarker identification [53]. The journey from raw spectral data to reliable protein quantification involves a sophisticated bioinformatics pipeline. This process is critical for transforming the millions of complex spectra generated by mass spectrometers into biologically meaningful information about protein expression, modifications, and interactions [54]. Within biomarker discovery research, the robustness of this pipeline directly determines the validity of candidate biomarkers identified through proteomic analysis.
The fundamental challenge addressed by bioinformatics pipelines lies in managing the high complexity and volume of raw MS data while controlling for technical variability introduced during sample preparation, instrumentation, and data processing [53]. A well-structured pipeline ensures this transformation occurs efficiently, accurately, and reproducibly—essential qualities for research intended to identify clinically relevant biomarkers. Modern pipelines achieve this through automated workflows that integrate various specialized tools for each analytical step, from initial peak detection to final statistical analysis [55] [56].
The proteomics bioinformatics pipeline follows a structured sequence that transforms raw instrument data into quantified protein identities. Figure 1 illustrates the complete pathway from spectral acquisition to biological insight, highlighting key stages including raw data processing, peptide identification, protein inference, quantification, and downstream analysis for biomarker discovery.
Figure 1: Overall proteomics bioinformatics workflow from raw spectra to biomarker discovery.
The pipeline begins with raw data conversion, where vendor-specific files are transformed into open formats like mzML or mzXML using tools such as MSConvert from ProteoWizard [53]. This standardization ensures compatibility with downstream analysis tools. The core computational stages then proceed through spectral processing (peak detection, retention time alignment), peptide and protein identification (database searching, false discovery rate control), quantification (label-free or label-based methods), and finally statistical analysis for biomarker candidate identification [54] [53].
Efficient pipeline architecture must emphasize reproducibility, scalability, and shareability—qualities enabled by workflow managers like Nextflow, Snakemake, or Galaxy [56]. These systems automate task execution, manage software dependencies through containerization (Docker, Singularity), and ensure consistent results across computing environments. For biomarker discovery studies, this reproducibility is paramount, as findings must be validated across multiple sample cohorts and research laboratories [55].
Detailed Experimental Protocols
Raw Data Preprocessing and Peptide Identification
The initial computational stage transforms raw instrument data into peptide identifications through a multi-step process requiring careful parameter optimization. Raw MS data, characterized by high complexity and volume, undergoes sophisticated preprocessing to convert millions of spectra into reliable peptide identifications [53].
Peptide Spectrum Matching (PSM) represents the core identification step where experimental MS/MS spectra are compared against theoretical spectra generated from protein sequence databases. Search engines like Andromeda (in MaxQuant) perform this matching by scoring similarity between observed and theoretical fragmentation patterns [57]. The standard protocol requires:
- Database Preparation: Using a species-specific protein sequence database (e.g., UniProt) while ensuring no decoy entries are present, as MaxQuant generates these automatically for false discovery rate estimation [57].
- Search Parameters: Configuring enzyme specificity (typically Trypsin/P with 1-2 missed cleavages), fixed modifications (e.g., Carbamidomethylation of cysteine), and variable modifications (e.g., Oxidation of methionine, Acetylation of N-termini) [57].
- Peptide Validation: Applying strict false discovery rate (FDR) controls using target-decoy approaches to filter incorrect peptide-spectrum matches, with the Human Proteome Organization (HUPO) recommending global FDR ≤1% for both peptide-spectrum matches and protein identifications [53].
Following peptide identification, protein inference assembles identified peptides into protein identities, with proteins sharing peptides grouped together. The HUPO guidelines recommend supporting each protein identification with at least two distinct, non-nested peptides of nine or more amino acids in length for reliable results [53]. This conservative approach minimizes false positives in downstream biomarker candidates.
Protein Quantification Methods
Protein quantification strategies vary based on experimental design, with each method offering distinct advantages for biomarker discovery applications. The selection between label-free and label-based approaches significantly impacts experimental design, cost, and data quality [54].
Table 1: Comparison of Quantitative Proteomics Methods
| Method | Principle | Acquisition Mode | Advantages | Limitations | Biomarker Applications |
|---|---|---|---|---|---|
| Label-Free (LFQ) | Compares peptide intensities or spectral counts across runs [54] | DDA or DIA | Suitable for large sample numbers, no chemical labeling required [53] | Higher technical variability, requires precise normalization [58] | Discovery studies with many samples |
| Isobaric Labeling (TMT, iTRAQ) | Uses isotope-encoded tags for multiplexing [54] | DDA with MS2 reporter ions | Reduces run-to-run variation, enables multiplexing (up to 16-18 samples) [53] | Ratio compression from co-isolated peptides, limited multiplexing capacity [53] | Small-to-medium cohort studies |
| SILAC | Metabolic incorporation of heavy amino acids [54] | DDA with MS1 peak pairs | High accuracy, minimal technical variation | Limited to cell culture systems, more expensive | Cell line models, stable systems |
| DIA/SWATH | Cycles through predefined m/z windows [54] | DIA | Comprehensive data acquisition, high reproducibility [58] | Complex data deconvolution, requires specialized analysis [54] | Ideal for biomarker verification |
For label-free quantification, the Extracted Ion Chromatogram (XIC) method quantifies peptides by extracting mass-to-charge ratios of precursor ions across retention time to generate chromatograms, with the area under these curves used for quantification [54]. Alternatively, Spectral Counting (SC) quantifies proteins based on the principle that higher abundance proteins produce more detectable peptide spectra, using the number of peptide spectrum matches associated with a protein to infer relative abundance [54].
Data-Independent Acquisition (DIA) methods like SWATH-MS have emerged as particularly powerful approaches for biomarker discovery due to comprehensive proteome coverage and high data completeness [58]. In DIA, the mass spectrometer cycles through predefined m/z windows, fragmenting all ions within each window rather than selecting specific precursors. This captures nearly all ion information, resulting in high data reproducibility—a critical feature for biomarker studies [54] [58].
Data Normalization for Biomarker Studies
Normalization represents a critical step in the quantification pipeline, particularly for label-free approaches where each sample is run individually, introducing potential systematic bias. This is especially crucial in SWATH-MS analyses where variations can significantly impact relative quantification and biomarker identification [58].
A systematic evaluation of normalization methods for SWATH-MS data demonstrated that while conventional statistical criteria might identify methods like VSN-G as optimal, biologically relevant normalization should enable precise stratification of comparison groups [58]. In this study, Loess-R normalization combined with p-value-based differentiator identification proved most effective for segregating test and control groups—the essential function of biomarkers [58].
The recommended normalization protocol includes:
- Log2 transformation of raw protein abundances to improve data distribution
- Application of Loess-R normalization to correct for systematic bias
- Implementation of median normalization or total ion current normalization as alternatives for specific data characteristics
- careful imputation of missing values using methods such as k-nearest neighbors (kNN) or random forest (RF), with evaluation to prevent overrepresentation of artifactual changes [53]
Proteogenomic Integration for Variant Biomarker Discovery
Proteogenomics integrates genomic variant data with proteomic analysis to identify variant protein biomarkers—an emerging approach with particular relevance to cancer and neurodegenerative diseases [59]. This strategy enables detection of mutant proteins and novel peptides resulting from disease-specific genomic alterations.
The proteogenomic workflow involves:
- Variant Identification: Performing whole-exome sequencing or RNA sequencing to identify single nucleotide variants, insertions/deletions, and mis-splicing events
- Custom Database Construction: Building a customized peptide library incorporating identified variants into normal protein sequences
- Variant Peptide Detection: Interrogating discovery proteomics data using the custom database to identify variant peptides
- Biomarker Validation: Confirming candidate variant biomarkers in large cohorts using targeted MS approaches [59]
This approach has successfully identified mutant KRAS proteins in colorectal and pancreatic cancers, and novel alternative splice variant proteins associated with Alzheimer's disease cognitive decline [59]. The proteogenomic strategy is particularly valuable for detecting tumor-specific somatic mutations and their translated products that could serve as highly specific biomarkers.
The Scientist's Toolkit
Essential Research Reagents and Materials
Table 2: Essential Research Reagents for Proteomics Biomarker Studies
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Trypsin (Proteomic Grade) | Protein digestion into peptides; cleaves C-terminal of R and K [57] | Use 1:50 trypsin:protein ratio (w/w); 16h digestion at 37°C; prevent autolysis |
| Iodoacetamide (IAA) | Alkylation of cysteine residues to prevent reformation of disulfide bridges [57] | 200mM concentration; incubate 1h in dark; follow DTT reduction |
| Dithiothreitol (DTT) | Reduction of disulfide bonds [57] | 200mM concentration; incubate 1h at room temperature |
| TMT or iTRAQ Reagents | Isobaric chemical labeling for multiplexed quantification [54] [53] | 6-16 plex available; monitor for ratio compression effects |
| SILAC Amino Acids | Metabolic labeling with stable isotope-containing amino acids [54] | Requires cell culture adaptation; effective incorporation check required |
| Heavy Isotope-Labeled Peptide Standards | Absolute quantification internal standards [53] | Essential for targeted proteomics; pre-quantified concentrations |
| C18 Desalting Columns | Peptide cleanup and purification [58] | Remove detergents, salts after digestion; improve MS sensitivity |
| SDS Buffer | Protein extraction and denaturation [58] | 2% SDS, 10% glycerol, 62.5mM Tris pH 6.8; boil 10min |
Bioinformatics Tools and Software
Table 3: Essential Bioinformatics Tools for Proteomics Pipelines
| Tool Category | Software Options | Primary Function | Biomarker Application |
|---|---|---|---|
| Workflow Managers | Nextflow, Snakemake, Galaxy [55] [56] | Pipeline automation, reproducibility, scalability | Ensures consistent analysis across sample batches |
| Raw Data Processing | MSConvert (ProteoWizard) [53] | Format conversion (to mzML/mzXML) | Standardization for public data deposition |
| DDA Analysis | MaxQuant, FragPipe, PEAKS [53] | Peptide identification, label-free quantification | Comprehensive proteome profiling |
| DIA Analysis | DIA-NN, Spectronaut [54] [53] | DIA data processing, library-free analysis | Ideal for biomarker verification studies |
| Targeted Analysis | Skyline, SpectroDive [53] | SRM/PRM assay development, absolute quantitation | Biomarker validation in large cohorts |
| Statistical Analysis | Limma, MSstats [53] | Differential expression, quality control | Identify statistically significant biomarkers |
| Visualization/QC | Omics Playground, PTXQC [53] [57] | Data exploration, quality assessment | Interactive biomarker candidate evaluation |
Advanced Data Analysis and Biomarker Discovery
Downstream Analysis Workflow
Following protein quantification and normalization, the pipeline progresses to downstream analysis specifically designed for biomarker discovery. This stage focuses on identifying biologically significant patterns rather than technical processing, with the goal of selecting the most promising biomarker candidates for validation.
Figure 2 illustrates the key computational and statistical processes in the downstream analysis workflow, showing how normalized quantitative data undergoes quality control, functional analysis, and machine learning to yield validated biomarker candidates.
Figure 2: Downstream analysis workflow for biomarker discovery from quantified proteomics data.
The downstream analysis encompasses three primary stages:
Functional Analysis: Annotating identified proteins with Gene Ontology terms, protein domains, and pathway information using tools like PANTHER and InterPro. This is followed by enrichment analysis to identify biological processes, molecular functions, and pathways significantly over-represented among differential proteins [53].
Network Analysis: Constructing protein-protein interaction networks using databases like STRING and visualization tools like Cytoscape. Co-expression analysis methods like WGCNA identify clusters of co-regulated proteins linked to phenotypic traits of interest, revealing functional modules beyond individual proteins [53].
Machine Learning Validation: Applying supervised learning algorithms (LASSO, random forests, support vector machines) to validate candidate proteins by correlating expression patterns with clinical outcomes. Cross-validation and independent cohort testing ensure robustness, while receiver operating characteristic (ROC) curves assess diagnostic accuracy of biomarker panels [53].
Data Visualization and Interpretation
Effective visualization is crucial for interpreting complex proteomics data and communicating findings to diverse audiences. Heatmaps represent one of the most valuable visualization tools, enabling researchers to identify patterns in large protein expression datasets across multiple samples [60] [61].
For proteomic applications, clustered heatmaps with dendrograms are particularly useful, as they group similar expression profiles together, revealing sample clusters and protein co-regulation patterns [60] [61]. These visualizations help identify biomarker signatures capable of stratifying patient groups—a fundamental requirement in diagnostic development.
When creating heatmaps for biomarker studies:
- Use diverging color palettes (blue-white-red) for expression data centered around zero
- Apply row-wise z-score normalization to emphasize relative expression patterns across samples
- Include sample annotations (clinical variables, treatment groups) to correlate protein patterns with phenotypes
- Implement interactive features (tooltips, zooming) for exploring large datasets in tools like Omics Playground [53] [61]
These visualization approaches transform quantitative protein data into actionable biological insights, facilitating the identification of robust biomarker candidates with true clinical potential.
Statistical Analysis and Machine Learning for Biomarker Candidate Selection
Mass spectrometry (MS)-based proteomics has emerged as a powerful platform for biomarker discovery, enabling the identification and quantification of thousands of proteins in biological specimens [19]. The high sensitivity, specificity, and dynamic range of modern MS instruments make them particularly suitable for detecting potential disease biomarkers in complex clinical samples such as blood, urine, and tissues [28] [19]. However, the enormous datasets generated in proteomic studies present significant analytical challenges that require sophisticated computational approaches for meaningful biological interpretation [62] [12].
Statistical analysis and machine learning (ML) serve as critical bridges between raw MS data and biologically relevant biomarker candidates. These computational methods enable researchers to distinguish meaningful patterns from analytical noise, address multiple testing problems inherent in high-dimensional data, and build predictive models for disease classification [63] [64]. The selection of robust biomarker candidates depends not only on appropriate computational methods but also on rigorous study design, proper sample preparation, and careful validation—all essential components of a reliable biomarker discovery pipeline [10].
This protocol outlines a comprehensive framework for biomarker candidate selection, integrating statistical and machine learning approaches within a mass spectrometry-based proteomics workflow. We provide detailed methodologies for experimental design, data processing, and analytical validation, with particular emphasis on addressing the unique characteristics of proteomics data that differentiate it from other omics datasets [63].
Experimental Design and Sample Preparation
Foundational Study Design Considerations
Robust biomarker discovery begins with meticulous experimental design that accounts for potential biases and confounding factors. Key considerations include proper cohort selection, statistical power assessment, sample blinding, randomization, and implementation of quality control measures throughout the workflow [10].
- Cohort Selection: Case-control studies should carefully match participants based on relevant clinical and demographic characteristics to minimize selection bias [10]. Sample size calculation should be performed a priori to ensure adequate statistical power for detecting biologically meaningful effect sizes [10].
- Sample Randomization and Blinding: Samples should be randomized throughout processing and analysis batches to prevent technical artifacts from being confounded with biological effects. Operators should be blinded to sample group assignments during data acquisition and initial processing phases [10].
- Quality Control: Implement systematic quality control procedures including use of internal standards, process controls, and technical replicates to monitor analytical performance throughout the workflow [10] [29].
Sample Preparation Protocols
Proper sample preparation is critical for generating high-quality MS data. While specific protocols vary based on sample type, the following general procedures apply to most clinical specimens:
Materials Required:
- Protein extraction buffer (e.g., RIPA buffer with protease inhibitors)
- Reduction and alkylation reagents (DTT or TCEP, and iodoacetamide)
- Proteolytic enzyme (typically sequencing-grade trypsin)
- Solid-phase extraction cartridges for cleanup (C18 or similar)
- Stable isotope-labeled standards (SIS) for quantification
Protocol for Plasma/Serum Samples:
- Depletion of High-Abundance Proteins: Remove top 14-20 abundant proteins using immunodepletion columns to enhance detection of lower-abundance potential biomarkers [29].
- Protein Digestion: Denature proteins with 8M urea, reduce disulfide bonds with 5mM DTT (30min, 60°C), alkylate with 15mM iodoacetamide (30min, room temperature in dark), and digest with trypsin (1:20-1:50 enzyme-to-protein ratio, 37°C, 12-16 hours) [19] [29].
- Peptide Cleanup: Desalt peptides using C18 solid-phase extraction cartridges and quantify using amino acid analysis or peptide quantification assays [19].
- Standard Addition: Add known quantities of stable isotope-labeled peptide standards (SIS) to enable absolute quantification [29].
Table 1: Critical Research Reagents for Sample Preparation
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| Protein Digestion Enzymes | Sequencing-grade trypsin | Specific proteolytic cleavage | Minimize autolysis; optimize ratio |
| Reduction/Alkylation Reagents | DTT/TCEP; iodoacetamide | Disulfide bond reduction and cysteine alkylation | Protect from light; fresh preparation |
| Stable Isotope Standards | SIS peptides, SIS proteins | Absolute quantification | Match to target peptides; account for digestion efficiency |
| Depletion Columns | Multiple affinity removal columns | Remove high-abundance proteins | Potential co-depletion of bound proteins |
| Solid-Phase Extraction | C18 cartridges | Peptide desalting and concentration | Recovery efficiency; salt removal |
Mass Spectrometry Data Acquisition and Preprocessing
Data Acquisition Strategies
Three primary MS acquisition methods are used in biomarker discovery, each with distinct advantages for downstream statistical analysis:
- Data-Dependent Acquisition (DDA): The most common discovery approach where the instrument automatically selects the most abundant precursor ions for fragmentation. While comprehensive, DDA can suffer from stochastic sampling and limited reproducibility across runs [19].
- Data-Independent Acquisition (DIA): Sequentially isolates and fragments all ions within predefined m/z windows, providing more comprehensive coverage and better quantitative reproducibility. DIA methods like SWATH-MS enable retrospective analysis of datasets as new hypotheses emerge [19].
- Targeted Acquisition: Using multiple reaction monitoring (MRM) or parallel reaction monitoring (PRM) to specifically quantify predetermined peptides with high sensitivity, precision, and accuracy. Particularly suited for verification and validation phases [19] [29].
Data Preprocessing Pipeline
Raw MS data requires extensive preprocessing before statistical analysis. The workflow includes:
- Peptide Identification: Match MS/MS spectra to peptide sequences using database search engines (e.g., Mascot, Sequest, X!Tandem) or de novo sequencing algorithms [28] [12].
- Protein Inference: Assemble identified peptides into proteins using algorithms that handle shared peptides and parsimony principles [12].
- Quantification: Extract peptide intensities using label-free methods, isobaric labeling (TMT, iTRAQ), or labeled internal standards [12].
- Quality Filtering: Remove poor-quality spectra, contaminants, and decoy hits based on false discovery rate (FDR) thresholds [28].
- Data Normalization: Correct for technical variation using methods like quantile normalization, LOESS, or global standards [63].
Diagram 1: MS Data Preprocessing Workflow. This workflow transforms raw mass spectrometry data into a cleaned, normalized data matrix suitable for statistical analysis and machine learning.
Statistical Analysis for Biomarker Discovery
Feature Extraction and Differential Analysis
The feature extraction approach involves detecting and quantifying discrete features (peaks or spots) that theoretically correspond to different proteins in the sample [63]. Statistical methods for identifying differentially expressed proteins include:
- Univariate Methods: Apply t-tests, ANOVA, or non-parametric equivalents (Mann-Whitney, Kruskal-Wallis) to individual features with multiple testing correction using False Discovery Rate (FDR) methods [63].
- Multivariate Methods: Use principal component analysis (PCA) for exploratory data analysis and dimensionality reduction, or partial least squares-discriminant analysis (PLS-DA) for supervised pattern recognition [63].
- Functional Modeling Approaches: Model the proteomic data in their entirety as functions or images using techniques like wavelet-based functional mixed models, which can detect features that might be missed by peak detection algorithms [63].
Table 2: Statistical Methods for Biomarker Discovery
| Method Category | Specific Techniques | Use Case | Advantages | Limitations |
|---|---|---|---|---|
| Univariate Analysis | t-test, ANOVA, Mann-Whitney | Initial screening for differential expression | Simple implementation; easy interpretation | Multiple testing burden; ignores correlations |
| Multiple Testing Correction | Benjamini-Hochberg FDR, Bonferroni | Control false positives in high-dimensional data | Balance between discovery and false positives | May be conservative; depends on effect size distribution |
| Multivariate Analysis | PCA, PLS-DA | Pattern recognition; dimensionality reduction | Captures covariance structure; visualization | Interpretation complexity; potential overfitting |
| Functional Data Analysis | Wavelet-based functional mixed models | Analyze raw spectral data without peak detection | Utilizes full data structure; detects subtle patterns | Computational intensity; methodological complexity |
| Power Analysis | Sample size calculation | Study design; validation planning | Ensures adequate statistical power | Requires preliminary effect size estimates |
Addressing Statistical Challenges in Proteomic Data
Proteomic data presents unique statistical challenges that require specialized approaches:
- Multiple Testing Problem: With thousands of simultaneous hypothesis tests, standard significance thresholds yield excessive false positives. Implement FDR control at 1-5% using Benjamini-Hochberg or related procedures [63].
- Missing Data: Abundance-dependent missingness is common in proteomics. Use methods specifically designed for missing-not-at-random data rather than simple imputation [63].
- Batch Effects: Technical variability across runs can introduce systematic biases. Implement randomization, include quality control samples, and use statistical correction methods like ComBat [10].
- Power Considerations: Proteomic studies often have limited sample sizes relative to feature numbers. Conduct power analysis during experimental design and consider sample pooling when appropriate [10].
Machine Learning for Biomarker Selection and Classification
Machine Learning Workflow and Algorithms
Machine learning provides powerful tools for both biomarker selection and sample classification. The typical workflow involves feature selection, model training, and validation [62] [64].
Diagram 2: Machine Learning Workflow for Biomarker Selection. This workflow demonstrates the iterative process of feature selection, model training, and validation used to identify robust biomarker panels.
Feature Selection Techniques
Feature selection is critical for identifying the most informative proteins from high-dimensional datasets:
- Filter Methods: Rank features based on univariate statistical tests (t-test, ANOVA) or correlation metrics, then select top performers. Efficient but ignores feature interactions [62] [64].
- Wrapper Methods: Use subset selection algorithms (forward/backward selection) with model performance as the selection criterion. Computationally intensive but considers feature interactions [64].
- Embedded Methods: Utilize algorithms that perform feature selection as part of the model building process, including LASSO regularization, random forests, and support vector machines with recursive feature elimination [62] [64].
Classification Algorithms for Biomarker-Based Diagnostics
Multiple machine learning algorithms can be applied to build classification models for disease diagnosis or stratification:
- Support Vector Machines (SVM): Effective in high-dimensional spaces, handle non-linear relationships using kernel tricks, and robust to overfitting [62] [64].
- Random Forests: Ensemble method that provides built-in feature importance measures, handles non-linear relationships, and reduces overfitting through bagging [64].
- Regularized Regression: LASSO and elastic net regression perform continuous variable selection while building predictive models, particularly useful when features are correlated [64].
Biomarker Validation and Clinical Translation
Validation Framework and Regulatory Considerations
Moving from biomarker discovery to clinical application requires rigorous validation:
- Technical Validation: Assess analytical performance including accuracy, precision, sensitivity, specificity, and reproducibility using established guidelines such as CLSI C64 [29].
- Biological Validation: Confirm association with disease across independent cohorts that reflect intended use population [10].
- Clinical Validation: Demonstrate clinical utility for intended use, such as diagnostic accuracy, prognostic value, or predictive capability for treatment response [29].
For regulatory approval of Laboratory Developed Tests (LDTs), targeted proteomics assays must undergo extensive validation including:
- Determination of analytical sensitivity (limit of detection, lower limit of quantification)
- Assessment of precision (intra- and inter-assay variability)
- Evaluation of analytical specificity (interferences, cross-reactivity)
- Verification of reportable range and reference intervals [29]
Targeted Proteomics for Verification
Targeted mass spectrometry using multiple reaction monitoring (MRM) or parallel reaction monitoring (PRM) provides highly specific verification of candidate biomarkers:
MRM Assay Development Protocol:
- Proteotypic Peptide Selection: Choose peptides unique to the target protein, ideally 7-20 amino acids long, avoiding missed cleavage sites and modifications [29].
- Transition Optimization: Directly infuse synthetic peptides to optimize collision energy and select optimal precursor-fragment ion pairs (typically 2-3 transitions per peptide) [29].
- Chromatographic Optimization: Develop LC methods to separate target peptides from potential interferences with appropriate retention time scheduling [29].
- Assay Characterization: Determine linear range, limit of detection, limit of quantification, precision, and accuracy using calibrated reference materials [29].
The integration of statistical analysis and machine learning with mass spectrometry-based proteomics has revolutionized biomarker discovery, enabling the identification of robust candidate biomarkers from complex biological samples. Success requires careful attention to all pipeline stages—from experimental design and sample preparation through data acquisition, computational analysis, and rigorous validation.
This protocol provides a comprehensive framework for statistical analysis and machine learning approaches in biomarker candidate selection, with detailed methodologies applicable across various disease contexts and sample types. As proteomic technologies continue to advance, these computational approaches will play an increasingly critical role in translating proteomic discoveries into clinically useful biomarkers that improve patient diagnosis, prognosis, and treatment selection.
Future directions in the field include the development of integrated multi-omics analysis pipelines, advanced machine learning methods that better handle the unique characteristics of proteomic data, and standardized frameworks for clinical validation and implementation of proteomic biomarkers.
Navigating Challenges: Common Pitfalls and Optimization Strategies in MS-Based Proteomics
Addressing the Dynamic Range Challenge in Complex Biofluids
Complex biofluids like human plasma and serum are invaluable sources for proteomic biomarker discovery, offering a rich composition of proteins and peptides that can reflect physiological and pathological states. However, these biofluids present a formidable analytical challenge: their protein concentrations span an extraordinary dynamic range, often exceeding 10 orders of magnitude [65]. Highly abundant proteins such as albumin, immunoglobulins, and fibrinogen can constitute over 90% of the total protein content, effectively masking the detection of low-abundance proteins that often hold high biological and clinical relevance as potential biomarkers [65] [19]. This dynamic range problem significantly impedes the sensitivity and depth of proteomic analyses, limiting our ability to discover novel disease biomarkers. This Application Note outlines standardized protocols and analytical strategies to overcome this challenge, enabling more comprehensive proteome coverage from complex biofluids within the context of biomarker discovery pipelines.
Sample Preparation Strategies
Effective management of the dynamic range challenge begins with strategic sample preparation to reduce complexity and enhance the detection of low-abundance species. The choice of method depends on whether the goal is broad depletion of abundant proteins or targeted enrichment of specific analytes.
Table 1: Comparison of Sample Preparation Methods for Dynamic Range Management
| Method | Principle | Best For | Advantages | Limitations |
|---|---|---|---|---|
| Bead-Based Enrichment [65] | Paramagnetic beads coated with binders selectively capture low-abundance proteins | High-throughput processing of plasma/serum; Automatable workflows | Exceptional reproducibility; Quick processing (∼5 hours); Low CVs | Requires specialized kits; Method development needed |
| Immunoaffinity Depletion [19] | Antibodies immobilized on resins remove top 7-14 abundant proteins | Deep proteome discovery; Reducing masking effects | Significant dynamic range compression; Commercial kits available | Costly; Potential co-depletion of bound LAPs; Sample loss |
| Protein Precipitation [66] | Organic solvents (e.g., acetonitrile) precipitate proteins from solution | Rapid cleanup of blood-derived samples | Simple, inexpensive; Minimal method development | Only removes proteins; Limited specificity |
| Phospholipid Depletion [66] | Scavenging adsorbents remove phospholipids post-PPT | Reducing ion suppression in LC-MS/MS | Improved data quality; Cleaner spectra | Does not target specific analytes |
| Supported Liquid Extraction (SLE) [66] | Liquid-liquid extraction on solid support for cleaner samples | Targeted analyte extraction | Higher recovery vs. traditional LLE; Easier automation | More complex method development |
Bead-Based Enrichment Protocol for Low-Abundance Proteins
Bead-based enrichment strategies offer a powerful solution for accessing the low-abundance proteome. The following protocol, adapted from the ENRICH-iST kit workflow [65], provides a standardized approach for enriching low-abundance proteins from plasma and serum samples.
Materials:
- ENRICH-iST Kit or similar bead-based enrichment platform
- Paramagnetic beads with functionalized surfaces
- Binding buffer, wash buffers, and elution buffers
- LYSE reagent for denaturation
- Sequencing-grade trypsin for digestion
- Solid-phase extraction (SPE) cartridges for cleanup
- Thermal shaker
- Centrifuge and vacuum manifold
Procedure:
- Sample Preparation: Dilute plasma/serum samples 1:10 with binding buffer to reduce viscosity and non-specific binding.
- Binding: Incubate diluted samples with paramagnetic beads for 45 minutes at room temperature with gentle agitation. The beads are coated with specific binders that selectively capture low-abundance proteins.
- Washing: Separate beads magnetically and discard supernatant. Wash beads twice with wash buffer to remove non-specifically bound material and highly abundant proteins.
- Lysis/Denaturation: Resuspend beads in LYSE reagent and incubate in a thermal shaker at 55°C for 10 minutes to denature captured proteins, reduce disulfide bonds, and alkylate cysteine residues.
- Digestion: Add sequencing-grade trypsin (1:20-1:50 enzyme-to-protein ratio) and incubate at 37°C for 4 hours or overnight to digest proteins into peptides.
- Peptide Purification: Acidify digested peptides and purify using SPE cartridges or StageTips to remove salts, detergents, and other contaminants.
- Analysis: Reconstitute purified peptides in LC-MS compatible solvent (e.g., 0.1% formic acid) for mass spectrometry analysis.
This protocol enables processing of up to 96 samples in approximately 5 hours, making it suitable for high-throughput biomarker discovery studies [65]. The method is compatible with human samples and other mammalian species including mice, rats, pigs, and dogs.
Mass Spectrometry Acquisition Methods
The choice of mass spectrometry acquisition method significantly impacts the ability to detect and quantify proteins across a wide concentration range in complex biofluids. Each approach offers distinct advantages for addressing dynamic range challenges.
Table 2: Mass Spectrometry Acquisition Methods for Complex Biofluids
| Method | Principle | Dynamic Range | Applications in Biomarker Discovery | Considerations |
|---|---|---|---|---|
| Data-Dependent Acquisition (DDA) [19] | Selects most intense precursor ions for fragmentation | Moderate | Discovery proteomics; Untargeted biomarker identification | Under-sampling of low-abundance peptides; Stochasticity |
| Data-Independent Acquisition (DIA) [19] | Fragments all ions in sequential m/z windows | High | Comprehensive biomarker discovery; SWATH-MS | Complex data analysis; Requires spectral libraries |
| Multiple Reaction Monitoring (MRM) [19] | Monitors predefined precursor-fragment ion pairs | Very High | Targeted biomarker verification/validation; Clinical assays | Requires prior knowledge; Limited multiplexing |
| Parallel Reaction Monitoring (PRM) [19] | High-resolution monitoring of all fragments for targeted precursors | High | Targeted quantification with high specificity | Requires high-resolution instrument |
Liquid Chromatography and Mass Spectrometry Parameters
For optimal coverage across the dynamic range, the following LC-MS/MS parameters are recommended:
Liquid Chromatography:
- Column: Reversed-phase C18 (75µm i.d. × 25cm, 1.6-2µm particle size)
- Gradient: 90-180 minutes linear gradient from 2% to 35% acetonitrile/0.1% formic acid
- Flow rate: 200-300 nL/min
- Temperature: 40-50°C
Mass Spectrometry (DIA method - SWATH-MS):
- MS1 Resolution: 30,000-60,000
- MS2 Resolution: 15,000-30,000
- Isolation Windows: 20-40 variable windows covering 400-1000 m/z
- Collision Energy: Stepped (e.g., 20, 35, 50 eV)
- Cycle Time: ~1-3 seconds
This DIA approach enables detection of 30,000-40,000 peptides across large sample sets, providing comprehensive coverage of the proteome [19].
Data Processing and Bioinformatics
Robust bioinformatics pipelines are essential for extracting meaningful biological information from the complex datasets generated in proteomic studies of biofluids. These pipelines address challenges in protein identification, quantification, and statistical analysis.
Protein Identification and Database Searching
Protein identification typically employs database search algorithms that match experimental MS/MS spectra to theoretical spectra derived from protein sequence databases [28] [12]. The concordance of multiple search algorithms significantly enhances the robustness of biomarker candidates.
Table 3: Bioinformatics Tools for Proteomic Data Analysis
| Tool Category | Software Examples | Key Functionality | Application in Biomarker Discovery |
|---|---|---|---|
| Database Search [12] | Mascot, SEQUEST, X!Tandem, Andromeda | Peptide identification from MS/MS spectra | Initial protein identification from complex mixtures |
| De Novo Sequencing [12] | PEAKS, NovoHMM, DeepNovo-DIA | Peptide sequencing without database | Identification of novel peptides, variants |
| Quantification [12] | MaxQuant, Skyline, Progenesis | Label-free or labeled quantification | Biomarker quantification across samples |
| Statistical Analysis [12] | Perseus, Normalyzer, EigenMS | Differential expression, normalization | Identifying significantly altered proteins |
| Machine Learning [64] | Random Forests, SVM, PLS-DA | Pattern recognition, classification | Sample classification, biomarker panel development |
Recommended Database Search Parameters:
- Enzyme: Trypsin (specific) with up to 2 missed cleavages
- Precursor Mass Tolerance: 10-20 ppm
- Fragment Mass Tolerance: 0.02-0.05 Da
- Modifications: Fixed - carbamidomethylation (C); Variable - oxidation (M), acetylation (protein N-term)
- False Discovery Rate (FDR): ≤1% at peptide and protein levels
Normalization Strategies for Quantitative Proteomics
Normalization is critical for accounting for technical variability and making samples comparable. Variance Stabilization Normalization (Vsn) has been shown to effectively reduce variation between technical replicates while maintaining sensitivity for detecting biologically relevant changes [67]. Alternative methods include linear regression normalization and local regression normalization, which also perform systematically well in proteomic datasets [67].
Integrated Biomarker Discovery Pipeline
A coherent pipeline connecting biomarker discovery with established approaches for evaluation and validation is essential for developing robust biomarkers [28]. This integrated approach increases the robustness of candidate biomarkers at each stage of the pipeline.
Experimental Design Considerations
Proper experimental design is fundamental for successful biomarker discovery:
Cohort Selection:
- Implement appropriate sample blinding and randomization
- Ensure sufficient statistical power through adequate sample size
- Match cases and controls for potential confounders (age, gender, BMI)
- Include independent validation cohorts
Quality Control:
- Implement quality control samples (pooled reference samples)
- Monitor technical variability throughout the workflow
- Establish standardized operating procedures for all pre-analytical steps [68]
Biomarker Verification and Validation
The biomarker development pipeline progresses through distinct stages:
- Discovery Phase: Untargeted proteomic analysis of well-designed sample cohorts
- Verification Phase: Targeted MS (MRM/PRM) analysis of candidate biomarkers in hundreds of samples
- Validation Phase: Large-scale analysis in independent cohorts (thousands of samples)
- Clinical Translation: Development of clinical grade assays for routine use
This structured approach ensures that only the most promising biomarker candidates advance through the resource-intensive validation process [69] [19].
Research Reagent Solutions
Table 4: Essential Research Reagents for Dynamic Range Management
| Reagent/Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Bead-Based Enrichment Kits [65] | ENRICH-iST Kit | Selective capture of low-abundance proteins | Compatible with human, mouse, rat, pig, dog samples; 5h processing time |
| Immunoaffinity Depletion Columns [19] | MARS-14, SuperMix Depletion | Remove top abundant proteins | Can process serum, plasma, CSF; Risk of co-depletion |
| Digestion Enzymes | Sequencing-grade trypsin | Protein digestion to peptides | Optimized ratio 1:20-1:50; 4h-overnight digestion |
| Protein Standard Mixes | UPS2, SIS peptides | Quantification standardization | Internal standards for absolute quantification |
| LC-MS Solvents & Additives | LC-MS grade water, acetonitrile, formic acid | Mobile phase components | Minimize background interference; Improve ionization |
| Solid-Phase Extraction | C18, HLB, SDB-RPS cartridges | Peptide cleanup | Remove salts, detergents, lipids |
Addressing the dynamic range challenge in complex biofluids requires an integrated approach spanning sample preparation, advanced mass spectrometry, and sophisticated bioinformatics. The protocols and methodologies outlined in this Application Note provide a standardized framework for enhancing the detection of low-abundance proteins in plasma and serum, thereby enabling more effective biomarker discovery. As MS-based proteomics continues to evolve, these strategies will play an increasingly vital role in translating proteomic discoveries into clinically useful biomarkers for diagnosis, prognosis, and treatment monitoring. The implementation of robust, standardized protocols across the entire workflow—from sample collection to data analysis—is essential for improving the reproducibility and clinical translation of proteomic biomarker research.
Mitigating Technical Variability and Batch Effects
Technical variability and batch effects present significant challenges in mass spectrometry-based proteomic studies, particularly in the context of biomarker discovery pipelines. Batch effects are technical, non-biological variations introduced into high-throughput data due to changes in experimental conditions over time, the use of different equipment or reagents, variations across personnel, or data processing through different analysis pipelines [70]. In proteomics, these effects can manifest as systematic shifts in protein quantification measurements, potentially obscuring true biological signals and leading to misleading conclusions if not properly addressed [70] [6].
The impact of batch effects on research outcomes can be profound. In the most benign cases, they increase variability and decrease statistical power for detecting genuine biological effects. More problematically, when batch effects correlate with outcomes of interest, they can lead to incorrect conclusions and contribute to the reproducibility crisis in biomedical research [70]. For biomarker discovery pipelines, where the goal is to identify robust protein signatures that distinguish health from disease, effectively mitigating technical variability is not merely an analytical optimization but a fundamental requirement for generating clinically relevant results [2] [6].
Technical variability in proteomic studies arises from multiple sources throughout the experimental workflow. Understanding these sources is essential for implementing effective mitigation strategies.
Table: Major Sources of Batch Effects in Proteomic Studies
| Experimental Stage | Specific Sources of Variability | Impact on Data |
|---|---|---|
| Study Design | Non-randomized sample collection, confounded experimental designs | Systematic differences between batches difficult to correct |
| Sample Preparation | Different reagent lots, protocol variations, personnel differences | Introduction of non-biological variance in protein measurements |
| Data Acquisition | Instrument calibration differences, column performance variations, LC-MS system maintenance | Systematic shifts in retention times, ion intensities, and mass accuracy |
| Data Processing | Different software versions, parameter settings, or analysis pipelines | Inconsistent protein identification and quantification across batches |
The fundamental cause of batch effects can be partially attributed to the basic assumptions of data representation in omics data. In quantitative omics profiling, the absolute instrument readout or intensity is often used as a surrogate for analyte concentration, relying on the assumption that there is a linear and fixed relationship between intensity and concentration under any experimental conditions. In practice, due to differences in diverse experimental factors, this relationship may fluctuate, making intensity measurements inherently inconsistent across different batches and leading to inevitable batch effects [70].
Impact on Biomarker Discovery
The pipeline for mass spectrometry-based biomarker discovery consists of several stages: discovery, verification, and validation [6]. Different mass spectrometric methods are used for each phase, with discovery typically employing non-targeted "shotgun" proteomics for relative quantification of thousands of proteins in small sample sizes. Batch effects can significantly impact each stage:
- Discovery Phase: Technical variability can lead to false positives or obscure true differentially expressed proteins, reducing the reliability of candidate biomarker lists [6].
- Verification Phase: Batch effects may compromise the selection of proteins for further validation, particularly when verification is performed on different instrumentation or with different technical protocols [6].
- Validation Phase: Uncorrected batch effects can lead to failure in clinical validation, wasting significant resources and delaying the translation of potential biomarkers to clinical use [2].
The problem is particularly acute in longitudinal studies and multi-center collaborations, which are common in biomarker development. In these scenarios, technical variables may affect outcomes in the same way as biological variables of interest, making it challenging to distinguish true biological changes from technical artifacts [70].
Strategic Approaches for Batch Effect Mitigation
Pre-analytical Strategies
Strategic experimental design represents the most effective approach for managing batch effects. Proper randomization of samples across batches ensures that technical variability does not confound biological factors of interest. When processing multiple sample groups, samples from each group should be distributed across all batches rather than processed as complete sets in separate batches [2] [70].
The implementation of quality control samples is critical for monitoring technical performance. Pooled quality control samples, created by combining small aliquots from all experimental samples, should be analyzed repeatedly throughout the batch sequence. These QC samples serve as a benchmark for assessing technical variation and can be used to monitor instrument performance over time [2].
Sample blinding and randomization are essential practices often underappreciated in proteomic studies. Technicians should be blinded to sample groups to prevent unconscious processing biases, and samples should be randomized across batches to avoid confounding biological variables with batch effects [2]. For longitudinal studies, where samples from multiple time points are analyzed, all time points for a given subject should be processed within the same batch whenever possible to minimize technical confounding of temporal patterns [71].
Computational Correction Methods
When batch effects cannot be prevented through experimental design, computational correction methods offer a powerful approach for mitigating their impact during data analysis.
Table: Computational Methods for Batch Effect Correction
| Method | Underlying Approach | Applicability to Proteomic Data | Key Considerations |
|---|---|---|---|
| ComBat | Empirical Bayes framework to adjust for batch effects | Well-established for microarray and proteomic data | Effectively removes batch effects while preserving biological signals; performs well when combined with quantile normalization [71] |
| Quantile Normalization | Aligns distribution of measurements across batches | Suitable for various proteomic quantification data | Normalizes overall distribution shape; effective as pre-processing step before other correction methods [71] |
| Harmony | Iterative clustering and integration based on principal components | Applicable to various high-dimensional data types | Effectively integrates datasets while preserving fine-grained subpopulations |
| MMUPHin | Specifically designed for microbiome data with unique characteristics | Limited direct applicability to proteomics | Demonstrates approach for data with high zero-inflation and over-dispersion |
For proteomic data, the combination of quantile normalization followed by ComBat has been shown to effectively reduce batch effects while maintaining biological variability in longitudinal gene expression data, an approach that can be adapted for proteomic applications [71]. The selection of an appropriate batch correction method should be guided by the specific characteristics of the proteomic data and experimental design, with validation performed to ensure that biological signals of interest are preserved.
Integrated Protocols for Batch Effect Management
Protocol 1: Quality Control and Sample Processing
Objective: To standardize sample processing procedures to minimize technical variability in mass spectrometry-based proteomic studies for biomarker discovery.
Materials:
- Protein Extraction Buffer: Lysis buffer containing appropriate detergents and protease inhibitors for efficient and reproducible protein extraction
- Digestion Reagents: High-purity trypsin or other proteolytic enzymes, dithiothreitol (DTT), iodoacetamide (IAA) for standardized protein digestion
- Quality Control Materials: Standard protein mixtures, pooled quality control samples from study specimens
- Chromatographic Standards: Retention time calibration standards for monitoring LC performance
Procedure:
- Sample Randomization: Randomize all samples across processing batches using a validated randomization scheme, ensuring balanced representation of experimental groups within each batch
- Quality Control Preparation: Create pooled quality control (QC) samples by combining small aliquots (e.g., 10-20 μL) from each study sample; prepare sufficient volume for multiple injections throughout the analytical sequence
- Standardized Processing: Process all samples using identical reagents from the same lots, with consistent incubation times and temperatures across all samples
- Batch Size Management: Limit batch sizes to maintain processing consistency; for large studies, implement a balanced block design with appropriate QC sampling
- Documentation: Meticulously document all processing parameters, including reagent lot numbers, instrument performance metrics, and any deviations from standard protocols
Validation: Monitor technical performance by analyzing QC samples throughout the sequence; evaluate metrics including total ion current, retention time stability, and intensity distributions of high-abundance features to identify potential batch effects.
Protocol 2: Data Acquisition and Processing
Objective: To acquire consistent, high-quality mass spectrometry data with minimal technical variability across multiple batches and analytical sessions.
Materials:
- Calibration Solutions: ESI-L low concentration tuning mix or appropriate mass calibration standards for the specific mass spectrometer platform
- Chromatographic Columns: Consistent source and lot of reverse-phase LC columns to minimize retention time variability
- Mobile Phase Reagents: High-purity solvents from single lots for entire study, mass spectrometry-grade additives (formic acid, ammonium bicarbonate)
- Data Processing Software: Uniform software versions and processing parameters across all datasets (e.g., FragPipe, MSstats, ProtPipe) [72] [73]
Procedure:
- System Calibration: Perform full instrument calibration before each batch analysis; verify performance using quality control standards
- Sample Order Randomization: Inject samples in randomized order with pooled QC samples inserted at regular intervals (e.g., every 6-10 samples)
- Reference Sample Analysis: Analyze a common reference sample at the beginning and end of each batch to monitor system performance drift
- Data Acquisition Parameters: Maintain consistent MS acquisition parameters across all batches, including collision energies, mass resolutions, and scan ranges
- Data Processing Consistency: Process all raw data files using identical software versions, database search parameters, and filtering criteria
Validation: Assess quantitative precision using coefficient of variation calculations for features detected in QC samples; evaluate batch effects using principal component analysis before and after computational correction.
Protocol 3: Computational Batch Effect Correction
Objective: To identify and correct for batch effects in processed proteomic data while preserving biological variability of interest.
Materials:
- Software Environment: R statistical environment (v4.0 or higher) with appropriate packages (sva, limma, ProtPipe) or Python with scikit-learn and batch correction modules [72] [71]
- Computational Resources: Adequate computing capacity for processing large proteomic datasets (recommended minimum 16GB RAM for moderate-sized studies)
- Data Input: Properly formatted protein or peptide quantification matrix with associated sample metadata including batch identifiers
Procedure:
- Batch Effect Assessment: Perform exploratory data analysis using principal component analysis (PCA) to visualize batch-associated clustering
- Method Selection: Select appropriate batch correction method based on data characteristics:
- For moderate batch effects with balanced design: ComBat or parametric empirical Bayes methods
- For severe batch effects with distributional shifts: Quantile normalization followed by ComBat [71]
- For complex multi-batch studies: Harmony or other advanced integration methods
- Correction Implementation: Apply selected correction method to normalized protein intensity data, specifying batch as the known technical variable and preserving biological covariates of interest
- Post-correction Validation: Verify effectiveness of correction by repeating PCA to confirm reduction of batch-associated clustering
- Biological Signal Preservation: Confirm that known biological differences (e.g., between clear positive controls) are maintained after correction
Validation: Use multiple metrics to assess correction effectiveness, including reduction in batch-associated variance, preservation of biological effect sizes, and improved classification accuracy in positive control samples.
The Scientist's Toolkit
Research Reagent Solutions
Table: Essential Materials for Batch Effect Mitigation in Proteomic Studies
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Pooled Quality Control Sample | Monitors technical performance across batches | Created by combining small aliquots of all study samples; analyzed repeatedly throughout sequence to track system performance |
| Standard Protein Mixture | Calibrates instrument response and monitors quantification accuracy | Commercial or custom mixtures with known protein concentrations; used for system suitability testing |
| Retention Time Calibration Standards | Aligns chromatographic elution profiles across batches | Chemical standards or digested protein standards that elute across the chromatographic gradient; enables retention time alignment |
| Single-Lot Reagents | Minimizes variability from different reagent batches | Critical for digestion enzymes, surfactants, and reduction/alkylation reagents; purchase in sufficient quantity for entire study |
| Standard Reference Materials | Benchmarks platform performance across laboratories | Well-characterized reference materials (e.g., NIST SRM 1950 for plasma proteomics) enable cross-study comparisons |
Implementation in Biomarker Discovery Pipeline
Integrating batch effect mitigation strategies throughout the biomarker discovery pipeline is essential for generating robust, reproducible results. The ProtPipe pipeline exemplifies this integrated approach, providing a comprehensive solution that streamlines and automates the processing and analysis of high-throughput proteomics and peptidomics datasets [72]. This pipeline incorporates DIA-NN for data processing and includes functionalities for data quality control, sample filtering, and normalization, ensuring robust and reliable downstream analyses.
For the discovery phase, where thousands of proteins are quantified across limited samples, implementing balanced block designs with embedded quality controls helps identify technical variability early in the process. As candidates move to verification phase, typically using targeted approaches like multiple reaction monitoring (MRM) on larger sample sets, maintaining consistent processing protocols across batches becomes critical [6]. Finally, during validation phase, where hundreds of samples may be analyzed, formal batch correction methods combined with rigorous quality control are essential for generating clinically relevant results.
The implementation of these strategies within a structured computational framework, such as the snakemake-ms-proteomics pipeline, enables reproducible and transparent processing of proteomic data [73]. This workflow automates key steps from raw data processing through statistical analysis, incorporating tools like FragPipe for peptide identification and MSstats for statistical analysis of differential expression, while providing comprehensive documentation of all processing parameters.
Effective management of technical variability and batch effects is not merely a quality control measure but a fundamental component of rigorous proteomic research, particularly in the context of biomarker discovery. By implementing strategic experimental designs, standardized processing protocols, and appropriate computational corrections, researchers can significantly enhance the reliability and reproducibility of their findings. The integrated approach presented in this protocol—combining practical laboratory strategies with validated computational methods—provides a comprehensive framework for mitigating batch effects throughout the proteomic workflow. As the field continues to advance toward clinical applications, with pipelines like ProtPipe offering automated solutions [72], the systematic addressing of technical variability will remain essential for translating proteomic discoveries into clinically useful biomarkers.
Best Practices for Improving Sensitivity and Reproducibility
The critical importance of sensitivity and reproducibility in mass spectrometry (MS)-based proteomics cannot be overstated, particularly in the high-stakes context of biomarker discovery pipelines. The fluctuating reproducibility of scientific reports presents a well-recognised issue, frequently stemming from insufficient standardization, transparency, and a lack of detailed information in scientific publications [74]. In proteomics, this challenge is compounded by the complexity of sample processing, data acquisition, and computational analysis, where minor methodological variations can significantly impact the quantitative accuracy and reliability of results [75] [76]. Simultaneously, achieving sufficient analytical sensitivity is paramount for detecting low-abundance protein biomarkers that often hold the greatest clinical significance. This protocol details comprehensive strategies addressing both fronts—implementing robust experimental practices to enhance reproducibility while leveraging cutting-edge technological advances to maximize sensitivity—thereby establishing a foundation for credible, translatable biomarker research.
Experimental Design for Enhanced Reproducibility
Sensitivity Screens for Parameter Assessment
A powerful approach to systematically assess and improve methodological robustness involves implementing sensitivity screens. This intuitive evaluation tool helps identify critical reaction parameters that most significantly influence experimental outcomes [74]. The basic concept involves varying single reaction parameters in both positive and negative directions while keeping all other parameters constant, then measuring the impact on key output metrics such as yield, selectivity, or in the case of proteomics, protein quantification accuracy.
- Experimental Protocol:
- Define Standard Conditions: Establish baseline protocol parameters for your proteomics sample preparation (e.g., digestion time, enzyme-to-protein ratio, purification method).
- Select Key Parameters: Identify variables for testing (e.g., trypsin concentration, digestion duration, temperature, buffer pH, solid-phase extraction sorbent chemistry) [77].
- Systematic Variation: Vary each selected parameter individually across a defined range (e.g., ±50% for concentration, ±10°C for temperature) while maintaining other parameters at standard conditions [74].
- Quantitative Assessment: Measure the impact on critical outcomes (e.g., number of proteins identified, coefficient of variation in quantitation, signal-to-noise ratio for low-abundance proteins).
- Visualization: Plot results on a radar/spider diagram to graphically represent parameter sensitivity, highlighting areas requiring strict control [74].
Automated Liquid Handling Implementation
Manual pipetting variability represents a significant source of technical noise in proteomics workflows. Several studies have demonstrated that manual pipetting introduces measurable intra- and inter-individual imprecision that can compromise data quality [78]. Implementing automated liquid handling systems addresses this fundamental limitation.
- Implementation Protocol:
- System Selection: Choose a non-contact liquid handling system capable of dispensing appropriate volumes for your workflow (e.g., picoliter to microliter range) [78].
- Volume Optimization: Conduct pilot tests to determine optimal dispensing volumes that maintain detection sensitivity while minimizing reagent consumption.
- Process Validation: Perform precision testing using standard protein digests to confirm CV improvements over manual pipetting.
- Workflow Integration: Implement the automated system for critical variable steps such as reagent addition, sample transfer, and SPE elution [77].
Table 1: Sensitivity Screen Parameters for Proteomic Sample Preparation
| Parameter Category | Specific Variables | Recommended Testing Range | Impact Assessment Metric |
|---|---|---|---|
| Enzymatic Digestion | Trypsin:Protein Ratio | 1:10 to 1:100 | Peptide sequence coverage |
| Digestion Time | 4-18 hours | Quantitative reproducibility | |
| Digestion Temperature | 25-45°C | Missed cleavage rate | |
| Sample Cleanup | SPE Sorbent Chemistry | C18, C8, mixed-mode | Matrix effect reduction |
| Elution Solvent | 40-80% organic | Target analyte recovery | |
| Wash Stringency | 5-25% organic | Selective impurity removal |
Sample Preparation and Processing
Solid-Phase Extraction Optimization
Solid-phase extraction (SPE) remains a cornerstone technique for sample cleanup and enrichment in proteomics workflows. Optimal SPE performance directly enhances both sensitivity (through analyte enrichment) and reproducibility (through consistent matrix removal) [77].
- Optimization Protocol:
- Sorbent Selection: Choose sorbent chemistry based on your target analytes' physicochemical properties (e.g., C18 for hydrophobic peptides, mixed-mode for broader selectivity) [77].
- Conditioning Optimization: Test various conditioning solvents (e.g., methanol, acetonitrile, isopropanol) followed by equilibration with aqueous buffer to activate sorbent sites.
- Sample Loading: Adjust sample loading conditions including pH and ionic strength to maximize target analyte retention.
- Wash Step Optimization: Implement progressively stronger wash solvents to remove interfering compounds while retaining analytes of interest.
- Elution Optimization: Use the minimum sufficient elution solvent strength to recover analytes while concentrating the sample and leaving highly interferring compounds behind [77].
Standardized Processing Protocols
Inconsistent sample processing introduces significant variability in proteomic analyses, particularly when working with clinical specimens. Implementing standardized protocols with strict quality control checkpoints ensures comparable results across samples and batches [76].
- Standardization Protocol:
- Processing Time Control: Establish and adhere to strict processing timelines, particularly for plasma/serum separation (e.g., process all samples within 1 hour of collection) [76].
- Anticoagulant Consistency: Use the same anticoagulant across studies (e.g., heparin or EDTA) as this significantly impacts protein measurements [76].
- QC Samples: Incorporate quality control samples including pooled reference samples and process blanks in each batch.
- Centrifugation Parameters: Standardize centrifugation speed, duration, and temperature for all sample processing steps.
Table 2: Impact of Pre-Analytical Variables on Proteomic Reproducibility
| Pre-Analytical Variable | Impact on Reproducibility | Mitigation Strategy |
|---|---|---|
| Delayed Processing | Decreased correlation (r < 0.75 for 24% of proteins after 24-hour delay) [76] | Process samples within 1 hour of collection |
| Anticoagulant Type | Higher CV in EDTA (34% proteins with CV >10%) vs. heparin (8% proteins with CV >10%) [76] | Standardize anticoagulant across study |
| Freeze-Thaw Cycles | Variable protein degradation | Single freeze-thaw cycle maximum; proper aliquotting |
| Storage Duration | Moderate long-term stability effects (91% proteins with ICC ≥0.4 over 1 year) [76] | Standardize storage conditions and duration |
Mass Spectrometry Acquisition
High-Sensitivity PASEF Workflows
The parallel accumulation-serial fragmentation (PASEF) technology represents a breakthrough in sensitive proteomic analysis, particularly when implemented on trapped ion mobility spectrometry (TIMS) platforms [79]. This approach maximizes ion usage and simplifies spectra, enabling unprecedented sensitivity and depth in proteome coverage.
- PASEF Implementation Protocol:
- Instrument Setup: Utilize a TIMS-QTOF mass spectrometer (e.g., timsTOF) coupled with nanoflow liquid chromatography [79].
- Method Generation: Employ the py_diAID tool to optimally position isolation windows in the mass-to-charge and ion mobility space for data-independent acquisition (DIA) [79].
- Chromatographic Optimization: Use pre-formed gradients (e.g., Evosep One system) with tip-based sample preparation for robust analysis [79].
- Acquisition Parameters: For deep proteome coverage, apply the following typical settings:
- Mobility Range: 0.7-1.3 Vs/cm²
- Mass Range: 100-1700 m/z
- Accumulation Time: 100 ms
- Ramp Time: 200 ms
- Throughput Optimization: For high-throughput applications, employ 21-min gradients while maintaining identification of ~7,000 proteins in human cell lines [79].
Data Acquisition Modes and Parameters
Strategic selection of acquisition modes significantly impacts the balance between proteome coverage, quantitative accuracy, and analytical sensitivity. Understanding the strengths of different approaches allows researchers to match acquisition strategies to study goals.
- Acquisition Protocol Selection:
- Data-Dependent Acquisition (DDA): Optimal for comprehensive protein identification and discovery workflows.
- Data-Independent Acquisition (DIA): Superior for quantitative reproducibility and completeness of data recording, particularly when combined with PASEF (diaPASEF) [79].
- Targeted Acquisition: Maximum sensitivity for predetermined protein panels using parallel reaction monitoring (PRM) or multiple reaction monitoring (MRM).
High-Sensitivity PASEF Proteomics Workflow
Data Processing and Analysis
Reproducible Computational Processing
Computational processing represents a critical potential source of variation in proteomic analyses, particularly for untargeted experiments. Establishing standardized, reproducible data processing pipelines ensures that results reflect biological reality rather than analytical artifacts [80].
- MZmine 3 Processing Protocol:
- Data Import: Convert raw data to open formats (e.g., mzML) using ProteoWizard's msConvert tool [80] [81].
- Mass Detection: Identify masses in each spectrum using appropriate noise levels (e.g., FTMS: 1E3, ITMS: 1E1).
- Chromatogram Building: Construct chromatograms using a minimum height of 1E4 for centroid data.
- Chromatogram Deconvolution: Apply the "Local Minimum Search" algorithm with a chromatographic threshold of 90%, minimum search range of 0.5 minutes, and minimum absolute height of 1E4.
- Spectral Deisotoping: Use the "Isotopic Peaks Grouper" with a m/z tolerance of 0.001 (or 5 ppm) and retention time tolerance of 0.05 minutes.
- Alignment: Perform join alignment with a m/z tolerance of 0.001 (or 5 ppm) and weight for m/z set to 20.
- Gap Filling: Apply the "Peak Finder" gap filler with an m/z tolerance of 0.001 (or 5 ppm).
Statistical Considerations for Functional Enrichment
Methodological choices in statistical analysis profoundly impact functional enrichment results and biological interpretation in proteomics studies. A recent meta-analysis demonstrated that statistical hypothesis testing approaches and criteria for defining biological relevance significantly influence functional enrichment concordance [75].
- Statistical Analysis Protocol:
- Differential Expression: Apply multiple statistical approaches (e.g., t-test, Limma, DEqMS, MSstats, Bayesian methods) to assess robustness of findings [75].
- Consistency Assessment: Compare results across statistical methods; prioritize proteins consistently identified as significant.
- Functional Enrichment: Conduct Gene Ontology (GO) and KEGG pathway analysis using consistent relevance criteria (e.g., fold change thresholds) across comparisons.
- Concordance Evaluation: Assess functional enrichment consistency using Jaccard indices and correlation metrics [75].
Table 3: Essential Research Reagents and Tools for Sensitive Proteomics
| Reagent/Equipment Category | Specific Examples | Function in Workflow |
|---|---|---|
| Sample Preparation | Evotips (Evosep One) | Robust, standardized sample loading for nanoLC |
| Trypsin/Lys-C Mix | High-efficiency protein digestion | |
| S-Trap or FASP filters | Efficient detergent removal and digestion | |
| Chromatography | Pre-formed gradients (Evosep) | Ultra-robust chromatographic separation |
| C18 analytical columns (15-25cm) | High-resolution peptide separation | |
| Mass Spectrometry | PASEF-enabled methods | Maximum sensitivity acquisition |
| Data-independent acquisition | Comprehensive data recording | |
| Data Processing | MZmine 3 | Reproducible untargeted data processing |
| Spectronaut/AlphaDIA | DIA data analysis with high reproducibility |
Quality Control and Validation
Systematic QC Implementation
Comprehensive quality control measures are essential for monitoring both technical performance and data quality throughout the biomarker discovery pipeline. Implementing a multi-layered QC strategy enables early detection of issues and ensures data integrity.
- QC Implementation Protocol:
- System Suitability Standards: Analyze complex protein digests (e.g., HeLa cell lysate) at the beginning of each batch to verify instrument performance.
- Internal Standard Peptides: Incorporate stable isotope-labeled standard peptides for retention time monitoring and quantitative calibration.
- Pooled QC Samples: Include a pooled sample from all study groups as a recurrent quality control throughout the acquisition sequence.
- Process Blanks: Regularly analyze blank samples to monitor background contamination and carryover.
- Data Quality Metrics: Track key parameters including:
- Total identifications (coefficient of variation <15%)
- Median CV for quantitative measurements (<20%)
- Retention time stability (drift <0.5 minutes)
Reproducibility Assessment Framework
Quantifying reproducibility at multiple levels provides critical information about data quality and methodological robustness. Implementing a structured assessment framework enables objective evaluation of technical performance.
- Assessment Protocol:
- Technical Replicates: Process and analyze a subset of samples in replicate (n≥3) to measure intra-batch precision.
- Inter-Batch Correlation: Include reference samples in multiple batches to assess inter-batch reproducibility.
- Longitudinal Stability: For longitudinal studies, assess within-person stability over time using intra-class correlation coefficients (ICC) [76].
- Platform Reproducibility: For aptamer-based platforms like SOMAscan, demonstrate that ≥92% of proteins show CV<10% in heparin samples [76].
Comprehensive Quality Control Framework
Implementing the comprehensive practices detailed in this protocol establishes a robust foundation for sensitive and reproducible proteomic research essential for credible biomarker discovery. By addressing critical factors across the entire workflow—from experimental design and sample preparation through data acquisition and computational analysis—researchers can significantly enhance the reliability and translational potential of their findings. The integration of systematic sensitivity assessments [74], advanced acquisition technologies like PASEF [79], standardized processing workflows [80], and rigorous quality control [76] creates a synergistic framework that maximizes both analytical sensitivity and methodological reproducibility. As proteomic technologies continue to evolve toward single-cell analysis and spatial proteomics, adherence to these fundamental principles will remain essential for generating biologically meaningful, clinically relevant results that withstand the scrutiny of validation studies and ultimately contribute to advancements in precision medicine.
Avoiding Overfitting in High-Dimensional Data Analysis
In the field of proteomic mass spectrometry data research, the pursuit of robust biomarkers is fundamentally challenged by the curse of high-dimensionality. Modern mass spectrometry technologies can generate data with thousands of features (m/z values) from relatively few biological samples, creating an analytical landscape where the number of variables (p) far exceeds the number of observations (n) [82] [83]. This p≫n scenario creates a fertile ground for overfitting, where models mistakenly learn noise and random variations instead of genuine biological signals, ultimately compromising their generalizability to new datasets [84].
The implications of overfitting are particularly severe in clinical biomarker development, where unreliable models can lead to failed validation studies and misguided research directions. Studies have shown that without proper safeguards, mass spectrometry-based models may achieve deceptively high accuracy on initial datasets while failing completely in independent cohorts [82] [69]. This article establishes a rigorous framework of protocols and analytical safeguards designed to detect, prevent, and mitigate overfitting throughout the biomarker discovery pipeline, with particular emphasis on proteomic mass spectrometry applications.
Foundational Principles and Key Challenges
The Mechanism of Overfitting in High-Dimensional Spaces
Overfitting occurs when a machine learning model becomes overly complex and captures not only the underlying true signal but also the random noise present in the training data [84]. In high-dimensional proteomic data, this phenomenon is exacerbated by several interconnected factors:
- Data Sparsity: As dimensionality increases, data points become increasingly spread out through the feature space, making it difficult to estimate population parameters accurately from limited samples [83]
- Distance Metric Degradation: In high-dimensional spaces, Euclidean distances between points become less meaningful, affecting clustering and similarity-based algorithms [85]
- Multicollinearity: Mass spectrometry features often exhibit strong correlations, where multiple m/z values may represent related peptide fragments, creating redundancy that inflates model variance [84]
- False Discovery Inflation: With thousands of simultaneous hypothesis tests, the probability of falsely identifying insignificant m/z ratios as biomarkers increases dramatically without proper statistical correction [82]
Quantitative Manifestations of Overfitting
Table 1: Characteristic Signs of Overfitting in Proteomic Data Analysis
| Indicator | Acceptable Range | Concerning Pattern | Implication |
|---|---|---|---|
| Training vs. Test Performance Gap | <5% difference | >15% difference | Poor generalization |
| Feature-to-Sample Ratio | <1:10 | >1:2 | High overfitting risk |
| Model Complexity | Appropriate for data size | Excessive parameters | Noise memorization |
| Cross-Validation Variance | <10% between folds | >20% between folds | Instability |
Methodological Framework: Protocols to Mitigate Overfitting
Experimental Design and Preprocessing Protocol
Protocol 1: Sample Preparation and Data Acquisition
Proper experimental design begins before mass spectrometry data collection and represents the first line of defense against overfitting:
Cohort Sizing and Power Analysis: Prior to sample collection, perform statistical power analysis to determine the minimum sample size required for reliable detection of biomarker effects. For proteomic studies, a minimum of 50-100 samples per group is often necessary to achieve adequate power in high-dimensional settings [69].
Block Randomization: Implement randomized block designs to account for technical variability. Process case and control samples in interspersed runs across multiple days to prevent batch effects from being confounded with biological signals [82].
Blinding Procedures: Ensure technicians and analysts are blinded to group assignments during sample processing and initial data analysis to prevent unconscious bias introduction [69].
Quality Control Metrics: Establish predetermined quality thresholds for spectrum quality, signal-to-noise ratios, and calibration accuracy. Exclude samples failing these criteria before analysis begins.
Protocol 2: Data Preprocessing and Feature Stabilization
Signal Processing: Apply discrete wavelet transformation (DWT) to raw mass spectra using bi-orthogonal bior3.7 wavelet bases, which effectively denoise spectra while preserving peak information [82].
Normalization Procedure:
- Perform total ion current normalization to correct for overall intensity variations
- Apply quantile normalization to make intensity distributions comparable across samples
- Validate normalization using internal standards and quality control pools
Missing Value Imputation:
- For proteomic data with missing values, use probabilistic principal component analysis (PPCA) for imputation
- Limit imputation to features with <20% missingness
- Document imputation parameters for reproducibility
Dimensionality Reduction and Feature Selection Protocol
Protocol 3: Statistically-Guided Feature Selection
Effective feature selection reduces the dimensionality of the analysis, directly combating overfitting:
Univariate Filtering:
- Apply Mann-Whitney U-test or Kolmogorov-Smirnov test to identify features with significant differential expression
- Implement Benjamini-Yekutieli false discovery rate (FDR) control to account for multiple testing, targeting q<0.05
- Retain top 500-1000 features for subsequent multivariate analysis [82]
Multivariate Embedded Methods:
- Utilize LASSO (Least Absolute Shrinkage and Selection Operator) regularization to perform feature selection while building predictive models
- Implement recursive feature elimination with cross-validation (RFECV) to identify optimal feature subsets
- Employ stability selection to assess feature selection robustness across data perturbations
Biological Prior Integration:
- Incorporate domain knowledge by prioritizing features with established biological relevance
- Use pathway databases to weight features from biologically meaningful processes
- Balance data-driven and knowledge-driven selection to avoid exclusive reliance on either approach
Protocol 4: Dimensionality Reduction Techniques
Table 2: Comparison of Dimensionality Reduction Methods for Proteomic Data
| Method | Mechanism | Advantages | Limitations | Recommended Use |
|---|---|---|---|---|
| Principal Component Analysis (PCA) | Linear projection maximizing variance | Computationally efficient, deterministic | Assumes linear relationships | Initial exploration, large datasets |
| t-SNE | Nonlinear neighborhood preservation | Excellent cluster visualization | Computational intensity O(n²), stochastic | Final visualization of clusters |
| UMAP | Manifold learning with topological constraints | Preserves global structure, faster than t-SNE | Parameter sensitivity | General purpose nonlinear reduction |
Model Building and Validation Protocol
Protocol 5: Regularized Machine Learning Implementation
Algorithm Selection Guidelines:
- For linear models: Implement elastic net regularization combining L1 (LASSO) and L2 (ridge) penalties
- For complex relationships: Use support vector machines (SVM) with radial basis function kernels, optimizing complexity parameters via grid search
- For ensemble methods: Apply random forests with limited tree depth and feature sampling at splits
Regularization Parameter Tuning:
- Perform k-fold cross-validation (k=5-10) to determine optimal regularization strength
- Use one standard error rule to select the simplest model within one standard error of best performance
- Document all tuned parameters for reproducibility
Implementation Example - Regularized SVM:
Protocol 6: Rigorous Validation Framework
Double Cross-Validation:
- Implement nested cross-validation with inner loop for parameter tuning and outer loop for performance estimation
- Ensure feature selection is included within the cross-validation loop to prevent data leakage
- Report both inner and outer performance metrics with confidence intervals
Validation Cohort Requirements:
- Allocate 30-40% of total samples to an independent validation set before any analysis begins
- Ensure validation cohort matches discovery cohort in relevant clinical and technical characteristics
- Pre-specify success criteria for validation before conducting discovery analysis
Performance Metrics and Reporting:
- Report sensitivity, specificity, total recognition rate, and area under ROC curve
- Calculate precision-recall curves for imbalanced datasets
- Provide confusion matrices and per-class performance for multi-class problems
- Document number of support vectors (for SVM) as indicator of model complexity [82]
Integrated Workflow Visualization
Biomarker Discovery Pipeline with Integrated Overfitting Safeguards
Case Study: Colorectal Cancer Biomarker Discovery
A seminal study on matrix-assisted laser desorption ionization time-of-flight (MALDI-TOF) serum protein profiles from 66 colorectal cancer patients and 50 controls demonstrates the successful implementation of these overfitting prevention protocols [82]. The researchers employed:
- Discrete Wavelet Transformation for spectral denoising and compression
- Statistical feature selection using Mann-Whitney tests with Benjamini-Yekutieli FDR control
- Support Vector Machine classification with double cross-validation
- Generalizability assessment through analysis of support vector counts
This approach achieved a remarkable 97.3% recognition rate with 98.4% sensitivity and 95.8% specificity, while maintaining robustness against overfitting as evidenced by the high generalization power of the resulting classifiers [82].
Table 3: Performance Metrics from CRC Biomarker Study Implementation
| Validation Metric | Training Performance | Test Performance | Generalization Gap |
|---|---|---|---|
| Total Recognition Rate | 99.1% | 97.3% | 1.8% |
| Sensitivity | 99.2% | 98.4% | 0.8% |
| Specificity | 98.9% | 95.8% | 3.1% |
| Number of Support Vectors | - | 18.3±2.1 (mean±sd) | Indicator of simplicity |
Essential Research Reagents and Computational Tools
Table 4: Research Reagent Solutions for Robust Proteomic Biomarker Discovery
| Reagent/Tool | Function | Implementation Example | Overfitting Prevention Role |
|---|---|---|---|
| Magnetic Beads (MB-HIC Kit) | Serum peptide isolation | Bruker Daltonics MB-HIC protocol | Standardizes sample preparation to reduce technical variance |
| α-Cyano-4-hydroxycinnamic acid | MALDI matrix substance | 0.3 g/L in ethanol:acetone 2:1 | Ensures consistent crystal formation for reproducible spectra |
| Quality Control Pools | Process monitoring | Inter-spaced reference samples | Detects batch effects and analytical drift |
| Discrete Wavelet Transform | Spectral denoising | bior3.7 wavelet basis | Reduces noise while preserving signal, minimizing noise fitting |
| LASSO Regularization | Feature selection & shrinkage | GLMNET implementation | Automatically selects relevant features, excludes redundant ones |
| UMAP | Nonlinear dimensionality reduction | umap-learn Python package | Enables visualization without over-interpretation of clusters |
| Double Cross-Validation | Performance estimation | scikit-learn Pipeline | Provides unbiased performance estimate, prevents data leakage |
Avoiding overfitting in high-dimensional proteomic mass spectrometry data requires a comprehensive, multi-layered approach spanning experimental design, data preprocessing, analytical methodology, and validation. By implementing the protocols outlined in this article—including adequate sample sizing, appropriate feature selection, regularization techniques, and rigorous validation—researchers can develop biomarker signatures with genuine biological relevance and clinical utility. The framework presented here provides a standardized methodology for maximizing discovery while minimizing false leads in the challenging landscape of high-dimensional proteomic data analysis.
Troubleshooting Guide for Sample Preparation and Instrument Performance
In mass spectrometry-based proteomic pipelines for biomarker discovery, the reliability of your final results is entirely dependent on the quality of sample preparation and instrument performance. Flawed processes in these early stages can lead to irreproducible data, false leads, and ultimately, failed biomarker validation [7]. This guide provides a systematic approach to troubleshooting both sample preparation and instrument issues, framed within the context of a multi-stage biomarker pipeline that progresses from discovery to verification and validation [6]. By implementing these protocols, researchers can minimize analytical variability, thereby increasing the likelihood of identifying clinically relevant biomarkers.
Troubleshooting Mass Spectrometry Instrument Performance
Instrument performance issues can manifest as sensitivity loss, poor mass accuracy, or chromatographic abnormalities. Systematic troubleshooting is essential for maintaining data quality throughout large-scale biomarker studies.
Common Instrument Issues and Solutions
The table below summarizes frequent instrument-related problems and their recommended solutions:
Table 1: Common Mass Spectrometry Instrument Issues and Solutions
| Problem | Possible Causes | Recommended Solutions |
|---|---|---|
| Loss of sensitivity [86] [87] | Ion source contamination, gas leaks, detector issues | Clean ionization source; check for gas leaks using a leak detector; verify detector settings and performance [86] [87]. |
| Poor vacuum [86] | Vacuum system leaks, pump failures | Use leak detector to identify and repair leaks; check pump oil levels and performance; inspect and replace worn vacuum system components [86]. |
| No or low signal/peaks [87] | Sample not reaching detector, column cracks | Check auto-sampler and syringe function; inspect column for cracks; ensure flame is lit (if applicable) and gases flowing correctly; verify sample preparation [87]. |
| Poor chromatographic performance [88] [89] | Contaminated LC system, inappropriate mobile phase | Use volatile mobile phase additives (e.g., formic acid); avoid non-volatile salts and phosphates; perform sufficient sample clean-up; use divert valve to protect MS from contamination [88] [89]. |
| Inaccurate mass measurement [90] | Instrument requires calibration | Recalibrate using appropriate calibration solutions; verify correct database search parameters (species, enzyme, fragment ions, mass tolerance) [90]. |
| High background noise [88] [89] | Mobile phase contaminants, dirty ion source | Use highest purity additives; clean ion source; ensure water quality is HPLC grade and freshly prepared; use mobile phase bottles dedicated for LC-MS only [88] [89]. |
Systematic Instrument Troubleshooting Workflow
The following decision tree outlines a logical approach to diagnosing and resolving common instrument performance issues:
Figure 1: Logical workflow for systematic troubleshooting of mass spectrometry instrument issues. Begin with a benchmarking method to isolate problems to either samples or the instrument itself, then follow specific diagnostic paths based on symptom type [90] [89].
Instrument Performance Assessment Protocol
Purpose: To diagnose whether performance issues originate from the instrument or sample preparation.
Materials:
- Pierce HeLa Protein Digest Standard (or equivalent performance standard) [90]
- Pierce Peptide Retention Time Calibration Mixture [90]
- Appropriate LC-MS calibration solution for your instrument [90]
- LC-MS system with benchmarking method
Procedure:
- System Performance Check:
- Inject 5 replicates of HeLa protein digest standard using your standard proteomic method [90].
- Evaluate key parameters: number of protein identifications, peptide intensity reproducibility, retention time stability.
LC System Assessment:
- Use peptide retention time calibration mixture to diagnose LC system and gradient performance [90].
- Check for retention time shifts, peak broadening, or abnormal peak shapes.
Mass Accuracy Verification:
- Run appropriate calibration solution for your instrument.
- Verify mass accuracy is within manufacturer specifications for your instrument type.
Data Analysis:
- Compare results to historical performance data for your system.
- If benchmark results are normal, problem likely lies with sample preparation [89].
- If benchmark results are abnormal, proceed with instrument-specific troubleshooting.
Troubleshooting Sample Preparation in Proteomics
Sample preparation is often the greatest source of variability in proteomic studies. Consistent, high-quality sample preparation is particularly crucial for biomarker discovery where quantitative accuracy across many samples is required.
Common Sample Preparation Issues and Solutions
Table 2: Common Sample Preparation Issues and Solutions in Proteomics
| Problem | Impact on Data Quality | Solutions & Preventive Measures |
|---|---|---|
| Polymer contamination [88] | Ion suppression, obscured peaks, reduced sensitivity | Avoid surfactants like Tween, Triton X-100; use filter tips; avoid chemical wipes containing PEG; implement solid-phase extraction (SPE) clean-up if contamination occurs [88]. |
| Keratin contamination [88] | Reduced depth of proteome coverage | Wear gloves; perform sample prep in laminar flow hood; avoid natural fiber clothing (wool); replace gloves after touching contaminated surfaces [88]. |
| Protein/peptide adsorption [88] | Loss of low-abundance proteins/peptides | Use "high-recovery" LC vials; prime vessels with BSA; avoid complete drying of samples; limit sample transfers using "one-pot" methods (e.g., SP3, FASP) [88]. |
| Incomplete protein digestion [91] | Reduced peptide counts, poor protein coverage | Optimize digestion time; consider double digestion with different proteases; use controlled enzymatic digestion protocols; verify digestion efficiency with quality control measures [91] [37]. |
| Protein degradation [91] | Artificial proteome patterns, missing biomarkers | Add protease inhibitor cocktails (EDTA-free); work at low temperatures (4°C); use PMSF; avoid repeated freeze-thaw cycles [91]. |
| Sample loss (low-abundance proteins) [91] | Inability to detect potential low-level biomarkers | Scale up experiment; use fractionation protocols; implement immunoenrichment; use integrated sample preparation methods like iST [91] [37]. |
| Matrix effects (ion suppression) [37] | Quantitative inaccuracy | Implement robust sample clean-up; use selective peptide enrichment; standardize sample matrices across preparations; use internal standards [37]. |
Sample Preparation Troubleshooting Workflow
The following workflow provides a systematic approach to diagnosing sample preparation issues:
Figure 2: Systematic approach to troubleshooting sample preparation issues in proteomics. This workflow emphasizes verification at each step to identify where problems occur, from initial protein extraction to final peptide recovery [91] [88].
Protocol: GeLC-MS/MS Sample Preparation for Complex Samples
Purpose: To provide a robust protein separation and digestion method suitable for complex biomarker discovery samples, combining SDS-PAGE fractionation with mass spectrometric analysis [92].
Materials:
- SDS-PAGE equipment and reagents [92]
- Destaining Buffer: 50% acetonitrile, 50% 100 mM EPPS pH 8.5 [92]
- Digestion Buffer: 100 mM EPPS pH 8.5 [92]
- Trypsin, sequencing grade [92]
- Reduction/Alkylation reagents: TCEP, IAA, DTT [92]
- Peptide Extraction Solution: 1% formic acid, 75% acetonitrile [92]
- StageTip materials: Empore C18 Membrane, pipette tips [92]
Procedure:
- Protein Denaturation, Reduction and Alkylation:
Protein Precipitation (Methanol-Chloroform Method):
- Dilute sample to ~100 µl in 1.5 ml microcentrifuge tube [92].
- Add 400 µl 100% methanol, vortex 5 sec [92].
- Add 100 µl 100% chloroform, vortex 5 sec [92].
- Add 300 µl water, vortex 5 sec [92].
- Centrifuge 1 min at 14,000 g, remove aqueous and organic layers, retain protein disk [92].
- Add 400 µl 100% methanol, vortex, centrifuge 2 min at 14,000 g [92].
- Remove supernatant, air dry protein pellet [92].
SDS-PAGE Fractionation:
In-Gel Digestion:
Peptide Extraction:
Peptide Cleanup (StageTip Protocol):
- Prepare StageTip with C18 membrane [92].
- Condition with 100 µl methanol, then 100 µl StageTip wash buffer [92].
- Load sample in StageTip reconstitution buffer [92].
- Wash with 100 µl StageTip wash buffer [92].
- Elute with 50 µl StageTip elution buffer [92].
- Dry peptides and reconstitute in mass spectrometry loading buffer [92].
Essential Research Reagent Solutions
The table below outlines key reagents and materials essential for successful proteomic sample preparation and mass spectrometry analysis in biomarker research:
Table 3: Essential Research Reagent Solutions for Proteomic Mass Spectrometry
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Protein Digest Standards [90] | System performance verification; troubleshooting sample preparation issues | Pierce HeLa Protein Digest Standard; used to test sample clean-up methods and LC-MS system performance [90]. |
| Retention Time Calibrants [90] | LC system diagnosis; gradient performance assessment | Pierce Peptide Retention Time Calibration Mixture; synthetic heavy peptides for troubleshooting LC systems [90]. |
| Mass Calibration Solutions [90] | Mass accuracy verification; instrument calibration | Pierce Calibration Solutions; instrument-specific solutions for accurate mass measurement [90]. |
| Trypsin, Sequencing Grade [92] | Protein digestion; generates peptides for mass analysis | Promega Trypsin; high-purity enzyme for reproducible protein digestion [92]. |
| Reduction/Alkylation Reagents [92] | Protein denaturation; prevents disulfide bond reformation | TCEP, IAA, DTT; used in sequence for effective protein reduction and alkylation [92]. |
| StageTip Materials [92] | Peptide desalting and cleanup; sample preparation | Empore C18 Membrane; pipette tip-based cleanup system for peptide purification [92]. |
| Protease Inhibitor Cocktails [91] | Prevention of protein degradation; maintains sample integrity | EDTA-free cocktails with PMSF; broad-spectrum inhibition of aspartic, serine, and cysteine proteases [91]. |
| iST Sample Preparation Kits [37] | Integrated sample preparation; streamlined workflow for proteomics | PreOmics iST technology; combines protein extraction, digestion, and cleanup in single device [37]. |
Quality Control and Data Assessment in Biomarker Studies
Rigorous quality control is essential throughout the biomarker discovery pipeline to ensure reliable and reproducible results.
Key Parameters for Mass Spectrometry Data Quality Assessment
Purpose: To provide standardized metrics for evaluating the quality of proteomic data in biomarker studies.
Assessment Criteria:
- Intensity: Measure of peptide abundance; influenced by protein abundance and ionization efficiency [91].
- Peptide Count: Number of different detected peptides from the same protein; low counts may indicate poor digestion or low abundance [91].
- Coverage: Proportion of protein sequence covered by detected peptides; good coverage typically 40-80% for purified proteins, 1-10% for complex proteomes [91].
- Statistical Significance: P-value/Q-value (< 0.05) or Score indicating confidence in peptide identification [91].
- False Discovery Rate (FDR): Probability that significant signals are actually false positives; should be controlled (< 1-5%) in biomarker studies [91].
Protocol: Quality Control Check for Biomarker Discovery Experiments
Purpose: To verify data quality before proceeding with statistical analysis and biomarker candidate selection.
Procedure:
- Sample Quality Verification:
LC-MS Performance Metrics:
Digestion Efficiency Assessment:
- Evaluate missed cleavage rates (< 20%).
- Monitor peptide length distribution (optimal range 7-25 amino acids).
- Assess quantitative reproducibility across sample preparations.
Contamination Screening:
By implementing these comprehensive troubleshooting guides and quality control protocols, researchers in biomarker discovery can significantly improve the reliability of their proteomic data, thereby increasing the likelihood of successful biomarker verification and validation in subsequent pipeline stages.
From Candidates to Clinics: Verification, Validation, and Technology Assessment
In the rigorous pipeline for identifying biomarkers from proteomic mass spectrometry data, the transition from broad, discovery-phase profiling to focused, high-confidence verification is a critical step. Targeted mass spectrometry techniques, primarily Selected Reaction Monitoring (SRM) and Parallel Reaction Monitoring (PRM), are the cornerstones of this verification process [93]. While discovery proteomics (e.g., data-dependent acquisition or DDA) excels at identifying hundreds to thousands of potential biomarker candidates across a small sample set, it often lacks the quantitative precision, sensitivity, and reproducibility required for validation [93]. Targeted methods address these limitations by enabling highly sensitive, specific, and accurate quantification of a predefined set of proteins across large sample cohorts, making them indispensable for confirming the clinical relevance of candidate biomarkers before costly validation studies [94].
The core principle shared by SRM and PRM is the selective monitoring of signature peptides, which act as surrogates for the proteins of interest. This targeted approach significantly enhances sensitivity and quantitative accuracy compared to non-targeted methods. SRM, also known as Multiple Reaction Monitoring (MRM), is historically considered the "gold standard" for targeted quantification and is typically performed on a triple quadrupole (QQQ) mass spectrometer [95] [93]. PRM is a more recent technique that leverages high-resolution, accurate-mass (HRAM) instruments, such as quadrupole-Orbitrap systems, offering distinct advantages in specificity and simplified method development [96] [97]. This application note provides a detailed comparison of these two techniques and outlines standardized protocols for their application in the verification of biomarker candidates.
Principles and Instrumentation
Selected Reaction Monitoring (SRM) operates on a triple quadrupole mass spectrometer. The first quadrupole (Q1) is set to filter a specific precursor ion (peptide of interest). The second quadrupole (Q2) acts as a collision cell, fragmenting the precursor. The third quadrupole (Q3) is then set to filter one or several specific fragment ions derived from that precursor [98] [94]. The instrument cycles through a predefined list of these precursor-fragment ion pairs (transitions), providing highly sensitive detection. However, developing a robust SRM assay requires extensive upfront optimization to select the most sensitive and interference-free transitions and to determine ideal instrument parameters like collision energy [95].
Parallel Reaction Monitoring (PRM) is performed on HRAM instruments, most commonly a quadrupole-Orbitrap platform. Similar to SRM, the first quadrupole (Q1) isolates a specific precursor ion, which is then fragmented in a collision cell (e.g., via Higher-energy Collisional Dissociation, HCD). The key difference is that instead of filtering for specific fragments in a third quadrupole, all resulting product ions are detected in parallel by the high-resolution Orbitrap mass analyzer [96] [97]. This yields a full, high-resolution MS/MS spectrum for the targeted peptide. The selection of which fragment ions to use for quantification is performed post-acquisition using software like Skyline, greatly simplifying method development and increasing flexibility [96].
The following diagram illustrates the fundamental differences in the workflows and instrumentation of these two techniques.
Performance Comparison in Verification Studies
The choice between SRM and PRM for a biomarker verification study depends on the specific requirements of the project, including the number of targets, sample complexity, available instrumentation, and need for assay development speed. Both techniques are capable of generating highly accurate quantitative data, but they exhibit distinct performance characteristics [99] [98].
Table 1: Comparative Analysis of SRM and PRM for Biomarker Verification
| Feature | SRM/MRM | PRM |
|---|---|---|
| Instrument Platform | Triple Quadrupole (QQQ) [96] [95] | Quadrupole-Orbitrap / Q-TOF [96] [95] |
| Mass Resolution | Unit (Low) Resolution [96] | High Resolution (≥30,000 FWHM) [96] |
| Data Acquisition | Monitors predefined precursor-fragment transitions [94] | Acquires full MS/MS spectrum for each precursor [96] |
| Quantitative Performance | High accuracy & precision, especially for low-concentration analytes [99] | Comparable linearity, dynamic range, and precision to SRM [98] |
| Selectivity & Specificity | Can be affected by co-eluting interferences [98] | Superior; high resolution eliminates most interferences [96] [97] |
| Method Development | Complex and time-consuming; requires transition optimization [95] | Simplified; no need to predefine fragment ions [95] [93] |
| Retrospective Analysis | Not possible; data limited to predefined transitions [96] | Yes; full MS/MS spectra allow re-interrogation [96] |
| Ideal Use Case | High-throughput, routine quantification of many samples [94] | Verification of tens to hundreds of targets with high specificity [95] [97] |
A key study evaluating these techniques from a core facility perspective confirmed that SRM and PRM show higher quantitative accuracy and precision compared to data-independent acquisition (DIA) approaches, particularly when analyzing low-concentration analytes [99]. Another study directly comparing SRM and PRM for quantifying proteins in high-density lipoprotein (HDL) concluded that the two methods exhibited comparable linearity, dynamic range, and precision [98]. The major practical advantage of PRM is its streamlined method development, as it eliminates the need for tedious optimization of collision energies and fragment ion selection [93].
Experimental Protocols for Biomarker Verification
Generic Sample Preparation Workflow
A critical prerequisite for robust targeted MS verification is consistent and reproducible sample preparation. The following protocol is adapted for serum/plasma, a common source for biomarker studies [98] [97].
- Sample Collection and Aliquot: Collect blood plasma or serum using standardized protocols. Centrifuge to remove cells and aliquot into low-protein-binding tubes. Store at -80°C until use.
- Protein Extraction and Denaturation: Thaw samples on ice. Dilute a volume of serum/plasma containing 10-100 µg of total protein in 100 mM ammonium bicarbonate. Add a denaturant such as 0.2% RapiGest (Waters) to solubilize proteins and disrupt interactions [98].
- Reduction and Alkylation: Add dithiothreitol (DTT) to a final concentration of 5-10 mM and incubate at 37°C for 30-60 minutes to reduce disulfide bonds. Then add iodoacetamide to a final concentration of 15-20 mM and incubate in the dark at room temperature for 30 minutes to alkylate cysteine residues.
- Proteolytic Digestion: Add sequencing-grade trypsin at a 1:20 to 1:50 (w/w) enzyme-to-protein ratio. Incubate at 37°C for 4-16 hours [98]. Quench the reaction by adding formic acid (typically 0.5-1% final concentration) to hydrolyze RapiGest and precipitate the detergent. Centrifuge to remove the precipitate.
- Peptide Desalting/Cleanup: Desalt the resulting peptide mixture using C18 solid-phase extraction (SPE) tips or columns (e.g., Sep-Pak). Elute peptides in a solution of 50-80% acetonitrile with 0.1% formic acid.
- Lyophilization and Reconstitution: Dry the eluted peptides in a vacuum concentrator. Reconstitute the peptide pellet in 0.1% formic acid in water for MS analysis. Determine peptide concentration if necessary (e.g., via BCA assay).
Protocol A: SRM Assay Development and Execution
This protocol details the steps for creating and running a verified SRM assay [94].
- Target Selection and Peptide Selection: From your discovery-phase data, select the biomarker candidate proteins. For each protein, choose 2-3 "proteotypic" peptides (peptides unique to the protein) that are readily observable by MS. Avoid peptides with missed cleavage sites, variable modifications, or problematic residues (e.g., M, C) [97].
- Transition Optimization and Method Building: This is the most labor-intensive step.
- Use software tools like Skyline or SRMColider to predict theoretical transitions for each peptide [94].
- Synthesize heavy isotope-labeled versions (e.g., containing 13C, 15N) of each target peptide. These will serve as internal standards for precise quantification.
- For each unlabeled and labeled peptide, inject them individually and use instrument software (e.g., MRMPilot, Pinpoint) or Skyline to empirically determine the 3-5 most intense fragment ions and their optimal collision energies [95].
- Compile the optimized transitions (precursor m/z > fragment m/z), collision energies, and expected retention times into a scheduled SRM method.
- Data Acquisition on QQQ-MS:
- Instrument: Triple quadrupole mass spectrometer (e.g., Thermo Scientific TQ series).
- Chromatography: Use nano-flow or capillary-flow LC with a C18 column and a 30-90 minute gradient.
- MS Settings: Operate in positive ion mode with a defined cycle time. Use a scheduled SRM approach with a retention time window (e.g., 3-5 minutes) to maximize the number of data points per peak.
- Data Analysis and Quantification:
- Import raw data into Skyline.
- The software will automatically integrate the chromatographic peaks for each transition.
- Manually inspect and curate peak integrations to ensure accuracy.
- For absolute quantification, the ratio of the peak area of the endogenous (light) peptide to the spiked internal standard (heavy) peptide is calculated. A calibration curve using the heavy standard can be used for absolute quantification [94].
Protocol B: PRM Assay Development and Execution
This protocol outlines the typically faster workflow for PRM analysis [96] [97].
- Target Selection and Inclusion List Creation:
- Similar to SRM, select target proteins and their proteotypic peptides.
- Compile an "inclusion list" containing the m/z and charge state of each precursor ion and their scheduled retention time windows. No fragment ion selection is needed at this stage.
- Instrument Setup on Q-Orbitrap-MS:
- Instrument: High-resolution mass spectrometer (e.g., Thermo Scientific Q Exactive HF-X, Orbitrap Fusion Lumos) [97].
- Chromatography: Similar to SRM protocol.
- MS Settings:
- Resolution: Set to 35,000-60,000 at m/z 200.
- Isolation Window: 1.0 - 2.0 m/z for the precursor ion.
- Fragmentation: HCD with normalized collision energy (e.g., 25-30%).
- AGC Target: 3e6 for MS2.
- Maximum Injection Time: 100-200 ms.
- Data Acquisition: Run the samples using the defined PRM method. The instrument will automatically isolate each precursor on the list, fragment it, and record the full MS/MS spectrum in the Orbitrap.
- Data Analysis and Quantification:
- Import the raw data into Skyline.
- Skyline will extract the chromatograms for all possible fragment ions from the high-resolution MS/MS data.
- The user can then select the 3-6 most intense, interference-free fragment ions for each peptide to generate quantitative data.
- Peak area integration and quantification (relative or absolute using heavy standards) is performed as in SRM.
Table 2: Key Research Reagent Solutions for Targeted MS Verification
| Item | Function/Description | Example Use Case |
|---|---|---|
| Heavy Isotope-Labeled Standards | Synthetic peptides with 13C/15N labels; serve as internal standards for precise normalization and absolute quantification [98] [94]. | Spiked into samples pre-digestion to correct for sample prep and ionization variability. |
| Single Labeled Protein Standard | A full-length protein with 15N-labeling; can act as a universal internal standard for relative quantification [98]. | Added to all samples for normalization, as demonstrated for HDL proteomics [98]. |
| Trypsin (Sequencing Grade) | High-purity proteolytic enzyme for specific and complete protein digestion into peptides for MS analysis [98]. | Standardized digestion of protein samples post-reduction and alkylation. |
| RapiGest / Surfactants | Acid-labile surfactants that improve protein solubilization and digestion efficiency, later removed without interference [98]. | Efficient denaturation of complex serum or tissue lysates prior to digestion. |
| C18 Solid-Phase Extraction Tips | Microscale columns for desalting and concentrating peptide mixtures after digestion. | Clean-up and concentration of digested peptide samples prior to LC-MS injection. |
| Skyline Software | A powerful, open-source Windows client for building SRM/PRM methods and analyzing targeted MS data [96] [94]. | Used throughout the workflow: method design, transition optimization, and data quantification. |
Integrated Application in a Biomarker Pipeline
The strategic placement of PRM and SRM within a biomarker discovery pipeline is best illustrated by a real-world example. A 2021 study on advanced lung adenocarcinoma aimed to identify serum biomarkers to predict the efficacy of pemetrexed/platinum chemotherapy [97]. The researchers employed a powerful two-stage mass spectrometry strategy:
- Discovery Phase with Data-Independent Acquisition (DIA): The team used DIA-based quantitative proteomics on a small set of 20 serum samples from patients with different chemotherapy responses. This unbiased approach identified 23 significantly differentially expressed proteins between the good and poor response groups [97].
- Verification Phase with PRM: To validate these candidate biomarkers with high confidence, the researchers then employed targeted PRM on the same sample set. The PRM analysis confirmed the differential expression trends for 10 of the candidates, with glutathione peroxidase 3 (GPX3) showing significant upregulation in the poor response group, consistent with the DIA results [97].
This case study exemplifies the synergy between discovery and verification platforms. The untargeted DIA screen broadened the net to find potential candidates, while the targeted PRM assay provided the specific, quantitative rigor needed to verify the most promising biomarkers before proceeding to larger, more costly validation studies (e.g., using immunoassays).
The following diagram summarizes this integrated workflow within the broader context of a clinical proteomics pipeline.
SRM and PRM are both powerful and complementary techniques for the critical verification stage in the mass spectrometry-based biomarker pipeline. SRM, performed on triple quadrupole instruments, remains a gold standard for highly sensitive and precise quantification, particularly in high-throughput settings. PRM, leveraging high-resolution Orbitrap technology, offers superior specificity, simplified method development, and the unique advantage of retrospective data analysis. The choice between them depends on project-specific needs, but the demonstrated ability of both techniques to generate reproducible and accurate quantitative data makes them indispensable for advancing robust biomarker candidates toward clinical validation.
Benchmarking MS Against Affinity-Based Platforms (Olink, SomaScan)
The pursuit of robust protein biomarkers relies on advanced proteomic technologies capable of precisely quantifying thousands of proteins in complex biological samples. Mass spectrometry (MS) and affinity-based platforms represent the two predominant approaches in high-throughput proteomics, each with distinct methodological foundations and performance characteristics. Mass spectrometry identifies and quantifies proteins by measuring the mass-to-charge ratio of peptide ions following enzymatic digestion and chromatographic separation, enabling untargeted discovery across a wide dynamic range [100] [101]. In contrast, affinity-based platforms including Olink and SomaScan utilize specific binding reagents—antibodies and aptamers, respectively—to detect predefined protein targets with high sensitivity and throughput [102] [103].
Understanding the relative strengths and limitations of these platforms is essential for designing effective biomarker discovery pipelines. MS provides unparalleled flexibility for detecting novel proteins, isoforms, and post-translational modifications (PTMs), while affinity platforms offer superior scalability for large cohort studies [100] [104]. Recent comparative studies have revealed significant differences in protein coverage, measurement correlation, and data quality between these technologies, highlighting the importance of platform selection based on specific research objectives [102] [103] [105]. This application note provides a comprehensive technical benchmark of these platforms to guide researchers in optimizing their proteomic workflows for biomarker identification and validation.
Technical Comparison of Platform Performance
Detection Capabilities and Coverage
Table 1: Proteomic Coverage and Detection Capabilities Across Platforms
| Platform | Technology | Proteome Coverage | Dynamic Range | Sensitivity | PTM Detection |
|---|---|---|---|---|---|
| MS (DIA) | Data-independent acquisition mass spectrometry | Broad, untargeted; 3,000-6,000+ proteins in plasma [104] [105] | Wide (6-7 orders of magnitude) [104] | Moderate to high (with enrichment) [104] | Yes (phosphorylation, glycosylation, etc.) [106] [101] |
| Olink | Proximity Extension Assay (PEA) + PCR | Targeted panels (3K-5K predefined proteins) [102] [105] | Moderate (optimized for clinical ranges) [104] | High for low-abundance proteins [104] [105] | No [101] [104] |
| SomaScan | Aptamer-based (SOMAmer) binding | Targeted panels (7K-11K predefined proteins) [102] [105] | Moderate [104] | Moderate for very low-abundance proteins [104] | No [101] [104] |
The selection of a proteomics platform significantly influences the depth and breadth of protein detection. Mass spectrometry excels in untargeted discovery, capable of identifying over 6,000 plasma proteins with advanced enrichment techniques and nanoparticle-based workflows [100] [105]. A key advantage of MS is its ability to detect post-translational modifications and protein isoforms, providing crucial functional insights that are inaccessible to affinity-based methods [106] [101]. For example, integrated multi-dimensional MS analyses can simultaneously profile total proteomes, phosphoproteomes, and glycoproteomes from the same sample, revealing cell line-specific kinase activities and glycosylation patterns relevant to cancer biology [106].
Affinity-based platforms offer substantial predefined content with Olink Explore HT measuring ~5,400 proteins and SomaScan 11K targeting approximately 10,800 protein assays [105]. However, their targeted nature limits detection to previously characterized proteins, potentially missing novel biomarkers [101]. Despite this limitation, affinity platforms demonstrate exceptional sensitivity for low-abundance proteins in complex samples like plasma, with Olink specifically designed to detect biomarkers present at minimal concentrations [104]. SomaScan provides the most extensive targeted coverage, identifying 9,645 plasma proteins in recent comparisons—the highest among all platforms assessed [105].
Data Quality and Technical Performance
Table 2: Technical Performance Metrics Across Platforms
| Performance Metric | MS (DIA) | Olink | SomaScan |
|---|---|---|---|
| Median Technical CV | ~10-20% [104] | 11.4-26.8% [105] | 5.3-5.8% [105] |
| Data Completeness | Variable (dependent on workflow) | 35.9% (Olink 5K) [105] | 95.8-96.2% [105] |
| Inter-platform Correlation | Reference standard | Median rho = 0.26-0.33 vs. MS [102] [103] | Median rho = 0.26-0.33 vs. MS [102] [103] |
| Reproducibility | High (10+ peptides/protein) [101] | Moderate | High |
Technical precision varies substantially across platforms, with important implications for biomarker reliability. SomaScan demonstrates exceptional analytical precision with the lowest median technical coefficient of variation (CV = 5.3-5.8%) and nearly complete data completeness (95.8-96.2%) across detected proteins [105]. This high reproducibility stems from optimized normalization procedures and robust assay design [103]. Olink platforms show higher technical variability (median CV = 11.4-26.8%), with the Olink 5K panel exhibiting particularly notable missing data (35.9% completeness) [105]. Filtering Olink data above the limit of detection improves CV to 12.4% but eliminates 40% of analytes, substantially reducing practical content [105].
Mass spectrometry precision depends heavily on the specific workflow employed. Label-free approaches typically show moderate reproducibility, while isobaric labeling methods (TMT, iTRAQ) offer enhanced precision through multiplexed design [107]. A key MS advantage is the ability to quantify multiple peptides per protein (averaging >10 peptides/protein), providing built-in technical replication that enhances measurement confidence [101]. Cross-platform correlations are generally modest, with median Spearman correlation coefficients of 0.26-0.33 between MS and affinity platforms for shared proteins [102] [103]. This discrepancy highlights that these technologies often capture different aspects of the proteome, suggesting complementary rather than redundant applications.
Practical Considerations for Implementation
Table 3: Practical Implementation Parameters
| Parameter | MS (DIA) | Olink | SomaScan |
|---|---|---|---|
| Sample Input | Higher (10-100 μg protein for tissues) [104] | Low (1-3 μL plasma/serum) [104] | Low (10-50 μL plasma/serum) [104] |
| Throughput | Moderate (sample prep + LC-MS/MS analysis) [104] | High (1-2 days post-sample prep) [104] | Very high (automation possible) [104] |
| Cost per Sample | Low (instrumentation, reagents) [104] | Moderate to high [104] | High [104] |
| Data Complexity | High (requires advanced bioinformatics) [104] | Low (processed data provided) [104] | Moderate (custom analysis tools) [104] |
Practical implementation factors significantly influence platform selection for biomarker studies. Sample requirements differ substantially, with MS typically requiring more material (10-100μg protein from tissues) compared to minimal inputs for affinity platforms (1-50μL plasma) [104]. This makes affinity methods preferable for biobank studies with limited sample volumes. Throughput considerations also favor affinity platforms, with Olink offering particularly rapid turnaround times (1-2 days post-sample preparation) compared to more time-consuming MS workflows requiring extensive chromatography and data acquisition [104].
Cost structures vary across platforms, with MS featuring lower per-sample reagent costs but substantial initial instrumentation investment [104]. Affinity platforms operate with higher per-sample costs but avoid major capital equipment expenditures. Data complexity represents another key differentiator, as MS generates complex datasets requiring sophisticated bioinformatics expertise, while affinity platforms typically provide processed data that is more readily interpretable [104]. This distinction makes MS ideal for discovery-phase research with bioinformatics support, while affinity platforms may better suit clinical validation studies with limited analytical resources.
Experimental Protocols for Platform Comparison
Sample Preparation Workflows
Sample Processing Workflows for MS and Affinity Platforms
Standardized sample collection protocols are critical for reliable cross-platform comparisons. Plasma samples should be collected using consistent anticoagulants (e.g., citrate or EDTA), processed promptly to avoid protein degradation, and stored at -80°C in low-protein-binding tubes [105]. For biomarker studies involving longitudinal collection, maintaining consistent processing protocols across all timepoints is essential to minimize pre-analytical variability [100].
The mass spectrometry workflow begins with protein enrichment or depletion to address plasma's dynamic range challenge. Effective methods include: (1) Nanoparticle-based enrichment (e.g., Seer Proteograph XT) using surface-modified magnetic nanoparticles to capture proteins across concentration ranges [105]; (2) High-abundance protein depletion (e.g., Biognosys TrueDiscovery) removing abundant proteins like albumin and immunoglobulins [105]; or (3) Protein precipitation (e.g., perchloric acid method) to concentrate proteins while removing interferents [100]. Following enrichment, proteins are denatured, reduced, alkylated, and digested with trypsin to generate peptides for LC-MS/MS analysis [107].
Affinity platform workflows require minimal sample preparation, typically involving sample dilution in platform-specific buffers. For Olink assays, samples are incubated with paired antibody probes that bind target proteins in close proximity, enabling DNA oligonucleotide extension and amplification for detection via next-generation sequencing [103] [104]. SomaScan assays incubate samples with SOMAmers (Slow Off-rate Modified Aptamers) that bind target proteins with high specificity, followed by washing steps to remove unbound material and fluorescent detection of bound complexes [102] [103]. Both affinity platforms incorporate internal controls and normalization procedures to correct for technical variability across assay runs.
Quality Control and Data Normalization
Robust quality control measures are essential for both platform types. For MS workflows, monitoring chromatography stability (retention time shifts, peak intensity), mass accuracy calibration, and internal standard performance ensures data quality [107]. Including quality control pools from representative sample types analyzed at regular intervals throughout the acquisition sequence helps identify technical drift [100]. For affinity platforms, assessing limit of detection (LOD), percent of values below detection thresholds, and replicate concordance identifies problematic assays [102] [105].
Data normalization approaches differ substantially between platforms. MS data typically requires batch correction to account for instrumental drift, often using quality control-based robust LOESS normalization or internal standard approaches [107]. Affinity platforms employ specialized normalization: SomaScan uses adaptive normalization by maximum likelihood (ANML) to adjust for inter-sample variability, while Olink applies internal controls and extension controls to normalize protein measurements [102] [103]. The normalization approach significantly impacts cross-platform correlations, with non-ANML SomaScan data showing higher agreement with Olink measurements [102].
Analytical Framework for Platform Assessment
Statistical Assessment of Platform Performance
Comprehensive platform evaluation requires multiple statistical measures assessing different performance dimensions. Precision should be evaluated through technical replication, calculating coefficients of variation (CV) across repeated measurements of the same samples [105]. Linear range assessment using spike-in experiments with purified proteins at known concentrations establishes quantitative boundaries for each platform [100]. Cross-platform concordance is best evaluated through Spearman correlation coefficients for shared proteins, acknowledging that different technologies may capture distinct protein subsets or forms [102] [103].
Advanced analytical approaches include principal component analysis to identify platform-specific technical artifacts and multivariate regression to quantify associations between protein measurements and clinical variables while controlling for platform effects [105]. For genetic applications, protein quantitative trait locus (pQTL) analysis identifies genetic variants associated with protein levels, with colocalization of pQTLs between platforms providing strong evidence for valid protein measurements [102]. Notably, proteins with colocalizing cis-pQTLs show substantially higher between-platform correlations (median rho = 0.72), indicating more reliable measurement [102].
Biological Validation of Platform Outputs
Technical performance metrics must be complemented with biological validation assessing real-world utility. Pathway enrichment analysis of proteins associated with clinical phenotypes (e.g., age, BMI, disease status) determines whether each platform identifies biologically plausible protein sets [102] [105]. Comparing observed protein-phenotype associations with established biological knowledge provides a critical validity check. For example, SomaScan 11K identified 282 unique age-associated plasma proteins in recent studies, while Olink 3K detected 176 exclusive age markers, with both platforms confirming established aging biomarkers like IGFBP2 and IGFBP3 [105].
Clinical predictive performance represents the ultimate validation, assessing how well protein panels from each platform stratify disease risk or progression. Studies comparing protein additions to conventional risk factors demonstrate that both Olink and SomaScan proteins improve predictive accuracy for conditions like ischaemic heart disease, with Olink increasing C-statistics from 0.845 to 0.862 and SomaScan to 0.863 [102]. MS platforms show particular promise for detecting proteoforms and PTMs with clinical relevance, such as phospho-Tau217 for Alzheimer's disease, which recently received FDA Breakthrough Device Designation based on promising data [108].
Essential Research Reagent Solutions
Table 4: Key Research Reagents and Solutions for Proteomic Platforms
| Reagent Category | Specific Products/Examples | Function in Workflow |
|---|---|---|
| Sample Enrichment/Depletion | Seer Proteograph XT [100] [105] | Nanoparticle-based protein enrichment for enhanced coverage |
| Biognosys TrueDiscovery [105] | High-abundance protein depletion for improved dynamic range | |
| PreOmics ENRICHplus [100] | Sample preparation kit for plasma proteomics | |
| Mass Spectrometry Standards | Biognosys PQ500 Reference Peptides [105] | Internal standards for absolute quantification |
| Tandem Mass Tags (TMT) [107] | Isobaric labeling for multiplexed quantification | |
| iTRAQ Reagents [107] | Isobaric tags for relative and absolute quantitation | |
| Affinity Reagents | Olink Explore Panels (3K, 5K) [102] [105] | Preconfigured antibody panels for targeted proteomics |
| SomaScan Kits (7K, 11K) [102] [105] | Aptamer-based kits for large-scale protein profiling | |
| Chromatography | C18 LC Columns [107] | Reverse-phase separation of peptides prior to MS |
| Ion Mobility Systems (TIMS, FAIMS) [108] | Enhanced separation power for complex samples |
The selection of appropriate research reagents significantly impacts proteomic data quality. For mass spectrometry, sample preparation kits like PreOmics ENRICHplus and Biognosys' P2 Plasma Enrichment method improve detection sensitivity for low-abundance plasma proteins [100] [105]. Internal standard solutions such as the Biognosys PQ500 Reference Peptides enable absolute quantification and better cross-platform harmonization [105]. Isobaric labeling reagents including Tandem Mass Tags (TMT) and iTRAQ allow multiplexed analysis, increasing throughput while maintaining quantitative precision [107].
For affinity-based platforms, reagent quality fundamentally determines data reliability. Olink's proximity extension assays rely on carefully validated antibody pairs that must bind target proteins in close proximity to generate detectable signals [103] [104]. SomaScan employs modified DNA aptamers (SOMAmers) with slow off-rate kinetics that provide specific binding to target proteins despite plasma complexity [102] [103]. Both platforms continue to expand their reagent panels, with Olink now covering ~5,400 proteins and SomaScan targeting nearly 11,000 protein assays in their most extensive configurations [105].
Integrated Workflow for Biomarker Pipeline Implementation
Integrated Biomarker Pipeline Leveraging Multiple Platforms
An effective biomarker development pipeline strategically integrates multiple proteomic platforms across discovery, validation, and confirmation phases. The discovery phase benefits from mass spectrometry's untargeted approach, applying data-independent acquisition (DIA) or tandem mass tag (TMT) methods to profile hundreds to thousands of proteins across moderate-sized cohorts (n=50-100) [100] [108]. This unbiased approach enables detection of novel biomarkers, protein isoforms, and post-translational modifications that might be missed by targeted methods [101]. Advanced MS instrumentation like the Orbitrap Astral mass analyzer now achieves deep proteome coverage (>6,000 plasma proteins) with minimal sample input, dramatically improving discovery potential [100].
The validation phase requires larger cohort sizes (n=500-1000+) where affinity platforms excel due to their high throughput, standardized workflows, and lower computational requirements [104] [105]. Both Olink and SomaScan effectively assess hundreds to thousands of candidate biomarkers across extensive sample sets, with SomaScan particularly advantageous for its extensive content (11,000 proteins) and Olink for its sensitivity to low-abundance analytes [105]. This phase should prioritize proteins showing consistent associations with clinical phenotypes across multiple platforms, as these demonstrate the greatest reliability for further development [103].
The confirmation phase utilizes targeted mass spectrometry approaches like parallel reaction monitoring (PRM) or SureQuant methods for absolute quantification of final biomarker candidates [105] [108]. These targeted MS assays provide exceptional specificity and quantitative accuracy, typically focusing on 10-500 proteins with precise internal standard calibration [107] [105]. The confirmed biomarker panels can then transition to clinical assay development using either validated MS workflows or immunoassay formats, depending on intended clinical implementation context and throughput requirements [107].
In proteomic mass spectrometry research for biomarker discovery, the establishment of robust assay parameters is not merely a procedural formality but a fundamental prerequisite for generating biologically meaningful and translatable data. Assays serve as the critical measurement system that transforms complex protein mixtures into quantitative data, enabling the identification of potential disease biomarkers. The reliability of this data hinges on rigorously validated assay parameters, particularly sensitivity, specificity, and reproducibility. Within a biomarker discovery pipeline, these parameters ensure that candidate biomarkers are not only accurately detected against a complex biological background but also that findings can be consistently replicated across experiments and laboratories, a necessity for advancing candidates into validation and clinical application [28]. Mass spectrometry-based proteomics offers a powerful platform for this endeavor, characterized by its high sensitivity, specificity, mass accuracy, and dynamic range [28]. This application note provides detailed protocols and frameworks for establishing these essential parameters, specifically tailored for researchers and scientists engaged in proteomic biomarker discovery.
Defining Key Assay Validation Parameters
The reliability of any assay within the biomarker pipeline is quantitatively assessed through a set of core validation parameters. A thorough understanding and precise calculation of these metrics are imperative for evaluating assay performance.
Sensitivity refers to the lowest concentration of an analyte that an assay can reliably distinguish from background noise. In the context of biomarker discovery, high sensitivity is crucial for detecting low-abundance proteins that may serve as potent biomarkers but are present in minimal quantities within complex biological samples [109]. It is often determined by measuring the limit of detection (LoD), frequently defined as the mean signal of the blank sample plus three standard deviations.
Specificity is the assay's ability to exclusively measure the intended analyte without cross-reacting with other substances or components in the sample [109]. For mass spectrometry-based proteomics, this is often achieved through multiple reaction monitoring (MRM) or parallel reaction monitoring (PRM) that target proteotypic peptides unique to the protein of interest. High specificity ensures that the signal measured is unequivocally derived from the target biomarker candidate, minimizing false positives [28].
Reproducibility (or Precision) measures the degree of agreement between repeated measurements of the same sample under stipulated conditions. It is a critical indicator of the assay's reliability over time and across different operators, instruments, and days. Poor reproducibility, often stemming from manual pipetting or inconsistent sample preparation, can lead to batch-to-batch inconsistencies and unreliable data, jeopardizing the entire biomarker pipeline [78].
Other essential parameters include Accuracy, which reflects how close the measured value is to the true value; Dynamic Range, the concentration interval over which the assay provides a linear response; and Robustness, the resilience of the assay's performance to small, deliberate variations in method parameters [109].
Table 1: Key Assay Validation Parameters and Their Definitions
| Parameter | Definition | Importance in Biomarker Discovery |
|---|---|---|
| Sensitivity | Lowest concentration of an analyte that can be reliably detected [109]. | Identifies low-abundance protein biomarkers. |
| Specificity | Ability to measure only the intended analyte without interference [109]. | Ensures biomarker signal is unique, reducing false positives. |
| Reproducibility | Closeness of agreement between repeated measurements [78]. | Guarantees consistent results across experiments and labs. |
| Accuracy | Closeness of the measured value to the true value [109]. | Ensures quantitative reliability of biomarker data. |
| Dynamic Range | Concentration range over which the assay response is linear [109]. | Allows quantification of biomarkers across varying expression levels. |
| Robustness | Capacity to remain unaffected by small, deliberate method variations [109]. | Ensures method transferability and reliability in different settings. |
Experimental Protocols for Parameter Establishment
Protocol for Determining Sensitivity (Limit of Detection - LoD)
Principle: This protocol determines the lowest concentration of a target peptide that can be reliably distinguished from a blank sample with a defined level of confidence.
Materials:
- Synthetic target peptide standard (≥ 95% purity)
- Peptide-free matrix (e.g., digested human plasma or serum)
- LC-MS/MS system
- Data analysis software (e.g., Skyline, MaxQuant)
Method:
- Sample Preparation: Prepare a dilution series of the synthetic peptide standard in the peptide-free matrix. The series should encompass a concentration range expected to be near the LoD, along with a minimum of 10 replicate blank samples (matrix without the peptide).
- Data Acquisition: Inject each sample, including the blanks and low-concentration standards, into the LC-MS/MS system using a standardized data-dependent acquisition (DDA) or targeted (MRM/PRM) method.
- Data Analysis:
- For each blank sample, measure the background response (peak area or intensity) at the retention time and mass-to-charge (m/z) of the target peptide.
- Calculate the mean (μblank) and standard deviation (SDblank) of these background responses.
- The LoD is typically calculated as: LoD = μblank + 3 × SDblank. The corresponding concentration is determined from the standard curve.
Protocol for Evaluating Specificity
Principle: This protocol verifies that the measured signal is unique to the target peptide and is not affected by co-eluting interferences or cross-talk from related peptides.
Materials:
- Biological sample containing the target protein
- Sample from a knock-out model or a system where the target protein is genetically silenced (if available)
- LC-MS/MS system
Method:
- Chromatographic Separation: Analyze the biological sample and ensure that the peak for the target peptide is chromatographically resolved from other ions. A symmetric, sharp peak with a consistent retention time indicates good specificity.
- MS/MS Spectrum Match: For DDA experiments, confirm that the acquired MS/MS spectrum of the precursor ion matches the theoretical fragmentation pattern of the target peptide using database search algorithms (e.g., Sequest, Mascot, X!Tandem) [28]. A high-confidence score indicates specificity.
- Interference Check: Analyze the knock-out or silenced control sample. The signal for the target peptide should be absent or significantly diminished, confirming that the assay is not detecting interfering substances.
- In-silico Specificity Check: Use BLAST or similar tools to confirm that the proteotypic peptide sequence used for quantification is unique to the target protein and not present in other proteins within the relevant organism's proteome [28].
Protocol for Assessing Reproducibility (Precision)
Principle: This protocol measures the assay's variation through repeated analysis of the same sample under different conditions.
Materials:
- Quality Control (QC) sample: A pooled biological sample or a sample spiked with a known concentration of the target peptide.
- LC-MS/MS system
Method:
- Experimental Design:
- Intra-assay Precision: Prepare and analyze the QC sample in a minimum of 5 replicates within a single analytical run.
- Inter-assay Precision: Prepare and analyze the QC sample in triplicate over at least three separate analytical runs on different days.
- Data Acquisition and Analysis:
- Quantify the target peptide in each injection.
- For each precision level (intra- and inter-assay), calculate the mean concentration and the standard deviation (SD).
- Calculate the coefficient of variation (CV) as: CV (%) = (SD / Mean) × 100.
- A CV of less than 15-20% is generally considered acceptable for bioanalytical assays, with more stringent criteria (e.g., <10%) required for advanced validation stages.
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and their critical functions in establishing robust assay parameters for mass spectrometry-based biomarker discovery.
Table 2: Essential Research Reagents and Materials for Mass Spectrometry Assays
| Item | Function | Application Note |
|---|---|---|
| High-Affinity Antibodies | For immunocapture to enrich target proteins/peptides, enhancing sensitivity and specificity [109]. | Critical for low-abundance biomarkers; minimizes non-specific binding. |
| Synthetic Isotope-Labeled Peptide Standards | Serve as internal standards for precise and accurate quantification (e.g., in SRM/MRM assays). | Corrects for sample preparation and ionization variability. |
| * Protease (e.g., Trypsin)* | Enzymatically digests proteins into peptides for mass spectrometry analysis. | Essential for bottom-up proteomics; requires high purity to avoid autolysis. |
| LC-MS/MS Grade Solvents | Used for mobile phases in liquid chromatography to ensure minimal background noise and ion suppression. | High purity is vital for consistent retention times and signal intensity. |
| Automated Liquid Handler | Precisely dispenses reagents and samples, minimizing human error and enhancing reproducibility [78]. | Reduces well-to-well variation and conserves precious samples. |
| Bead-Based Clean-Up Kits | Automate the tedious clean-up and purification of samples post-digestion or labeling [78]. | Improves reproducibility, reduces hands-on time, and increases throughput. |
A Coherent Pipeline for Biomarker Discovery
Integrating well-characterized assays into a coherent discovery pipeline is paramount for transitioning from initial discovery to validated candidate biomarkers. The workflow below visualizes this multi-stage process, emphasizing the continuous refinement and validation of assay parameters at each step. This pipeline, adapted from a proven model for microbial identification using Clostridium botulinum, demonstrates how robustness increases with each validation stage, enhanced by the concordance of various database search algorithms for peptide identification [28].
Biomarker Discovery and Validation Workflow
The pipeline's stages are:
- Sample Preparation: Proteins are extracted from complex biological sources and digested into peptides. At this stage, Specificity and Robustness are key, ensured by optimized and consistent digestion and clean-up protocols to minimize non-specific interactions and variability [110].
- Mass Spectrometry Analysis: Peptides are separated by liquid chromatography and analyzed by tandem mass spectrometry. The focus is on Sensitivity and Reproducibility, achieved through optimized instrument parameters and stable performance, often monitored using quality control samples [28].
- Database Searching & Peptide Identification: MS/MS spectra are matched to theoretical spectra in protein databases using search algorithms (e.g., Sequest, Mascot, X!Tandem). Specificity is assessed in-silico by evaluating the confidence of peptide-spectrum matches and using a consensus approach across multiple algorithms to reduce false positives [28].
- Bioinformatic Validation: Candidate biomarkers are rigorously filtered. This includes selecting peptides unique to the target organism or condition (using BLAST against related species) and ensuring they are conserved across replicates. This stage critically evaluates Specificity (cross-species) and Reproducibility across biological replicates, resulting in a shortlist of robust biomarker candidates [28].
The rigorous establishment of sensitivity, specificity, and reproducibility is the cornerstone of any successful proteomic mass spectrometry study aimed at biomarker discovery. By adhering to the detailed protocols and frameworks outlined in this application note—from precise experimental methods and reagent selection to integration into a coherent bioinformatics pipeline—researchers can significantly enhance the quality, reliability, and translational potential of their data. A meticulously validated assay is not merely a tool for measurement but a foundational element that ensures the identified biomarker candidates are genuine, quantifiable, and ultimately worthy of progression through the costly and complex journey of clinical validation.
The journey from discovering a potential biomarker to its routine application in clinical practice is a complex, multi-stage process. A discouragingly small number of protein biomarkers identified through proteomic mass spectrometry achieve FDA approval, creating a significant bottleneck between discovery and clinical use [111]. This bottleneck is largely due to the incredible mismatch between the large numbers of biomarker candidates generated by modern discovery technologies and the paucity of reliable, scalable methods for their validation [111]. Clinical validation sets a dauntingly high bar, requiring that a biomarker not only demonstrates a statistically significant difference between populations but also performs responsibly and economically within a specific clinical scenario, such as diagnosis, prognosis, or prediction of treatment response [112] [111]. The success of this clinical validation is entirely dependent on a rigorous prior stage: analytical validation, which ensures that the measurement method itself is accurate, precise, and reproducible for the intended analyte [113]. This application note details structured protocols and considerations for navigating these critical validation stages to improve the flux of robust protein biomarkers into clinical practice.
Analytical Validation: Establishing Assay Robustness
Analytical validation is the foundation upon which all clinical claims are built. It credentials the assay method itself, proving that it reliably measures the intended biomarker in the specified matrix.
Core Analytical Performance Metrics
A comprehensive analytical validation assesses the key performance characteristics outlined in Table 1. These experiments should be conducted using the final, locked-down assay protocol.
Table 1: Essential Analytical Performance Metrics and Validation Protocols
| Performance Characteristic | Experimental Protocol | Acceptance Criteria |
|---|---|---|
| Accuracy & Precision | - Analyze ≥5 replicates of Quality Control (QC) samples at Low, Mid, and High concentrations over ≥5 separate runs.- Use spiked samples if a purified standard is available.- Calculate inter- and intra-assay CVs and mean percent recovery [113]. | Intra-assay CV < 15%; Inter-assay CV < 20%; Mean recovery of 80-120% [113]. |
| Lower Limit of Quantification (LLOQ) | - Analyze a series of low-concentration samples and determine the lowest level that can be measured with an inter-assay CV < 20% and accuracy of 80-120% [113]. | Signal-to-noise ratio typically > 5; CV and accuracy meet predefined targets. |
| Linearity & Dynamic Range | - Analyze a dilution series of the analyte across the expected physiological range.- Perform linear regression analysis [113]. | R² > 0.99 across the claimed range of quantification. |
| Selectivity & Specificity | - Test for interference by spiking the analyte into different individual matrices (n≥6).- For MS assays, confirm using stable isotope-labeled internal standards and specific product ions [28] [113]. | No significant interference (<20% deviation from expected value). |
| Stability | - Expose samples to relevant stress conditions (freeze-thaw cycles, benchtop temperature, long-term storage).- Compare measured concentrations to freshly prepared controls [112]. | Analyte recovery within 15% of baseline value under defined conditions. |
The Role of Targeted Mass Spectrometry
For protein biomarkers, targeted mass spectrometry methods, particularly Selected Reaction Monitoring (SRM) or multiple reaction monitoring (MRM), have emerged as powerful tools for analytical validation. These techniques provide the specificity and multiplexing capability needed to verify candidate biomarkers in hundreds of clinical samples before investing in expensive immunoassay development or large-scale clinical trials [114] [111]. SRM assays are developed using synthetic peptides that are proteotypic for the protein of interest. The mass spectrometer is configured to specifically detect and quantify these signature peptides, providing a highly specific and quantitative readout of protein abundance [114].
Clinical Validation: Establishing Clinical Utility
Once a biomarker assay is analytically validated, it must be tested in a well-defined clinical cohort to establish its performance for a specific clinical context of use.
Study Design and Sample Cohort Definition
The single most critical factor in successful clinical validation is a rigorous study design driven by a clear clinical need [112]. The clinical objective must be explicitly defined a priori—whether for diagnosis, prognosis, or prediction—as this determines the required patient population and controls.
- Cohort Selection: The cohort must be representative of the target population. It is critical to include not only healthy controls but also patients with closely related diseases or similar symptoms to properly challenge the biomarker's specificity [112]. For a bladder cancer diagnostic, for instance, this might mean comparing urine samples from confirmed cancer patients against those from healthy individuals and patients with other urological conditions like benign prostatic hyperplasia or urinary tract infections.
- Sample Size and Biobanking: Inadequate sample size is a major cause of failed validation studies. A well-powered clinical validation study may require hundreds, or even thousands, of samples [112] [115]. These samples must be collected from a well-managed biobank that employs standardized protocols for sample handling, storage, and data annotation to minimize pre-analytical variability [112]. One statistical model suggests that for ovarian cancer biomarkers, a verification cohort of 50 cases and 50 controls can yield good candidates, but successful clinical validation may require a cohort of 250 cases and 250 controls to have a >90% chance of success [112].
- Blinding and Randomization: The analysis of samples from different clinical groups should be performed in a blinded and randomized fashion to prevent analytical bias.
Performance Evaluation and Statistical Analysis
The performance of a clinically validated biomarker is defined by its ability to correctly classify patients.
- Key Metrics: The primary metrics are sensitivity (the ability to correctly identify those with the disease) and specificity (the ability to correctly identify those without the disease) [112]. These are used to construct a Receiver Operating Characteristic (ROC) curve, and the Area Under the Curve (AUC) provides a single measure of overall discriminatory power.
- Context is Critical: The required performance thresholds are entirely dependent on the clinical context. A screening biomarker applied to millions of healthy people requires extraordinarily high specificity to avoid a large number of false positives, while a diagnostic biomarker used in a symptomatic population can tolerate a different balance [111]. The bar for clinical validation is not just statistical significance, but clinical usefulness and economic feasibility [111].
Integrated Workflows and the Scientist's Toolkit
The Biomarker Validation Pipeline
The following diagram illustrates the complete pathway from biomarker discovery to clinical application, highlighting the critical, iterative nature of analytical and clinical validation.
Biomarker Translation Pathway
Enhancing Robustness with Bioinformatics and Machine Learning
Modern validation pipelines increasingly rely on computational tools to enhance the robustness of biomarker candidates before costly wet-lab validation.
- Database Search Algorithm Concordance: Using multiple database search algorithms (e.g., Sequest, Mascot, X!Tandem) for peptide identification and prioritizing candidates identified by a consensus of these algorithms significantly increases confidence and reduces false positives [28]. One study on Clostridium botulinum showed that while individual algorithms identified 12-34 candidate biomarkers, the robust consensus of all three algorithms yielded only 8 high-confidence candidates [28].
- Machine Learning for Classification: Machine learning (ML) techniques, such as support vector machines and random forests, can be applied to high-dimensional proteomics data to build classification models that differentiate disease states [62] [64]. These models can both validate the diagnostic power of a biomarker panel and identify the most informative features within that panel, refining the biomarkers selected for analytical validation [116].
The workflow below outlines how these computational validation steps are integrated.
Bioinformatics Validation Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials critical for executing the validation protocols described in this note.
Table 2: Key Research Reagent Solutions for Biomarker Validation
| Reagent / Material | Function in Validation Workflow | Key Considerations |
|---|---|---|
| Stable Isotope-Labeled Standards (SIS) | Acts as internal standard for MS-based quantification; corrects for sample prep losses and ion suppression [114]. | Peptide sequence should be proteotypic; label (e.g., 13C, 15N) should not co-elute with natural form. |
| Quality Control (QC) Samples | Monitors assay performance and reproducibility across multiple batches and runs [113]. | Should be matrix-matched; pools of patient samples are ideal. |
| Biobanked Clinical Samples | Provides well-annotated, high-quality samples for analytical and clinical validation studies [112]. | Standardized collection & storage protocols are critical; must have associated clinical data. |
| Digestion Enzymes (e.g., Trypsin) | Enables bottom-up proteomics by cleaving proteins into measurable peptides [117] [28]. | Sequence-grade purity ensures specificity and reproducibility; ratio to protein is key. |
| Chromatography Columns | Separates peptides by hydrophobicity (e.g., C18) to reduce sample complexity prior to MS injection [117]. | Column chemistry, particle size, and length impact resolution, sensitivity, and throughput. |
Navigating the path from a biomarker candidate to a clinically validated tool is fraught with challenges, most notably at the interface between discovery and validation. Success requires a deliberate, two-pronged strategy: first, a rigorous analytical validation that establishes a robust, reproducible, and specific assay, often leveraging targeted mass spectrometry; and second, a well-powered clinical validation that demonstrates clear utility within a specific clinical context of use. By adhering to structured protocols, employing bioinformatics and machine learning to prioritize the most promising candidates, and utilizing high-quality research reagents, researchers can increase the probability that their discoveries will transition from the research bench to the clinical bedside, ultimately fulfilling the promise of personalized medicine.
Application Note: Proteomic Biomarker Discovery in AML and HCC
This application note details the successful implementation of mass spectrometry (MS)-based proteomic pipelines for biomarker discovery in two distinct malignancies: Acute Myeloid Leukemia (AML), a hematological cancer, and Hepatocellular Carcinoma (HCC), a solid tumor. The document outlines the specific methodologies, key findings, and translational implications of these studies, providing a framework for researchers investigating cancer biomarkers.
Acute Myeloid Leukemia (AML) Case Study
AML is a genetically heterogeneous blood cancer characterized by uncontrolled proliferation of myeloid blast cells. Despite standardized risk stratification systems like the European LeukemiaNet (ELN) guidelines, a high relapse rate persists, driving the need for refined prognostic tools [118]. Proteomic profiling offers a direct method to identify executable molecular signatures that can improve risk classification.
Key Findings and Biomarker Signatures
A 2021 study utilized both nontargeted (label-free LC-MS/MS) and targeted (multiplex immunoassays) proteomics on bone marrow and peripheral blood samples from AML patients stratified by ELN risk categories (favorable, intermediate, adverse) [118]. The analysis revealed a range of proteins that were significantly altered between the different genetic risk groups. The study concluded that incorporating validated proteomic biomarker panels could significantly enhance the prognostic classification of AML patients, potentially identifying biological mechanisms driving resistance and relapse [118].
A separate, more recent 2024 multi-omics study analyzed the bone marrow supernatant of relapsed AML patients, integrating proteomic and metabolomic data with genetic characteristics [119]. This investigation identified 996 proteins and 4,831 metabolites. Through unsupervised clustering, they discovered significant correlations between protein expression profiles and high-risk mutations in ASXL1, TP53, and RUNX1. Furthermore, they identified 57 proteins and 190 metabolites that were closely associated with disease relapse, highlighting the role of the bone marrow microenvironment and lipid metabolism in AML progression [119].
Another successful application of a 5D proteomic approach (depletion, ZOOM-IEF, 2-DGE, MALDI-MS, ELISA validation) on plasma samples identified 34 differentially expressed proteins in AML versus healthy controls. Subsequent validation confirmed Serum Amyloid A1 (SAA1) and plasminogen as potential diagnostic plasma biomarkers for AML [120].
Table 1: Key Proteomic Biomarkers Identified in AML
| Biomarker/Category | Biological Sample | Association/Function | Proteomic Method |
|---|---|---|---|
| SAA1 | Plasma | Acute-phase protein; potential diagnostic biomarker | 5D Approach (2-DGE, MALDI-MS) [120] |
| Plasminogen | Plasma | Fibrinolysis; potential diagnostic biomarker | 5D Approach (2-DGE, MALDI-MS) [120] |
| Proteins linked to ASXL1/TP53/RUNX1 | Bone Marrow Supernatant | High-risk genetic profile; disease relapse | LC-MS/MS [119] |
| 57 Relapse-Associated Proteins | Bone Marrow Supernatant | Disease recurrence and prognosis | LC-MS/MS [119] |
| Risk Group-Specific Proteins | Bone Marrow Cells/Serum | ELN risk stratification (Favorable, Intermediate, Adverse) | Label-free MS, Multiplex Immunoassays [118] |
Hepatocellular Carcinoma (HCC) Case Study
HCC is a primary liver cancer and a leading cause of cancer-related deaths globally. Its management is often hampered by late diagnosis and the limited sensitivity and specificity of the current standard biomarker, Alpha-fetoprotein (AFP) [121]. The discovery of novel biomarkers is therefore critical for early detection, personalized treatment, and improved prognosis.
Key Findings and Biomarker Signatures
Advances in high-throughput technologies have accelerated biomarker discovery in HCC. Beyond AFP, several promising biomarkers have emerged:
- Glypican-3 (GPC3): A cell-surface proteoglycan highly expressed in HCC, useful for immunohistochemical diagnosis [121].
- Des-gamma-carboxy prothrombin (DCP): An abnormal prothrombin protein elevated in HCC, particularly in AFP-negative cases [121].
Genomic and proteomic studies have identified mutations and pathways driving HCC, enabling more personalized treatment strategies. Furthermore, liquid biopsies—the analysis of circulating tumor DNA (ctDNA) and circulating tumor cells (CTCs)—represent a non-invasive revolution for monitoring tumor dynamics, detecting minimal residual disease, and assessing therapeutic response [121].
A 2021 study emphasized the importance of robust biomarker discovery from high-throughput transcriptomic data. By applying six different machine learning-based recursive feature elimination (RFE-CV) methods to TCGA data, researchers identified a robust gene signature for HCC. The overlap between gene sets from different classifiers served as highly reliable biomarkers, with the selected features demonstrating clear biological relevance to HCC pathogenesis [122].
Table 2: Key Biomarker Categories in HCC
| Biomarker Category | Examples | Clinical Application | Key Feature |
|---|---|---|---|
| Serological Protein Biomarkers | AFP, GPC3, DCP | Diagnosis, Prognosis | Complements AFP's limitations [121] |
| Genetic Alterations | TERT promoter, TP53, CTNNB1 mutations | Prognosis, Targeted Therapy | Identified via NGS [121] |
| Liquid Biopsy Markers | ctDNA, CTCs | Monitoring, Resistance Detection | Non-invasive, dynamic monitoring [121] |
| Robust Transcriptomic Signature | Genes from RFE-CV overlap | Diagnosis, Classification | Machine-learning driven stability [122] |
Experimental Protocols
Protocol 1: 5D Proteomic Profiling for Plasma Biomarker Discovery (AML Example)
This protocol details a multi-dimensional fractionation strategy to enhance the detection of low-abundance plasma biomarkers, as applied in the AML case study [120].
I. Sample Preparation
- Sample Collection: Collect peripheral blood into K₂-EDTA tubes. Separate plasma by centrifugation at 2,200 × g for 10 minutes at 4°C. Pool individual samples if required and store aliquots at -80°C.
- Abundant Protein Depletion: Use a Multiple Affinity Removal System (MARS) column (e.g., Hu-7) via FPLC to deplete the top 7 abundant proteins (albumin, IgG, IgA, transferrin, antitrypsin, haptoglobin, fibrinogen).
- Protein Precipitation and Clean-up: Concentrate the flow-through fraction using 5 kDa molecular weight cut-off (MWCO) filters. Precipitate proteins using Trichloroacetic acid (TCA)/acetone.
- Reduction and Alkylation: Dissolve the pellet in a buffer containing 8 M Urea and 20 mM Tris. Reduce with 20 mM DTT and alkylate with 50 mM Iodoacetamide (IAM). Quench with 1% DTT.
II. Multi-Dimensional Fractionation and Analysis
- ZOOM-Isoelectric Focusing (ZOOM-IEF): Fractionate the protein sample into 5 distinct pH fractions using a ZOOM-IEF Fractionator.
- Two-Dimensional Gel Electrophoresis (2-DGE): Load each IEF fraction onto IPG strips for isoelectric focusing, followed by separation on SDS-PAGE gels.
- Protein Visualization and Digestion: Stain gels with Coomassie Blue. Excise protein spots of interest and digest in-gel with trypsin.
- Mass Spectrometry Analysis: Analyze digested peptides using Matrix-Assisted Laser Desorption/Ionization Mass Spectrometry (MALDI-MS) for protein identification.
III. Validation
- Validate candidate biomarkers (e.g., SAA1, Plasminogen) in individual patient samples using Enzyme-Linked Immunosorbent Assay (ELISA) [120].
Protocol 2: Integrated Multi-Omic Analysis of Bone Marrow Supernatant (AML Example)
This protocol describes the workflow for the simultaneous analysis of proteins and metabolites from bone marrow supernatant to explore the microenvironment in relapsed AML [119].
I. Sample Preparation and Data Acquisition
- Sample Collection: Centrifuge bone marrow aspirates at 1,500 rpm for 5 minutes at 10°C. Collect and store the supernatant at -80°C.
- Proteomics Sample Prep: Remove albumin and IgG from 40 µL of supernatant using a chromatographic column. Lyse the remaining proteins in SDS buffer, determine concentration via BCA assay, and separate via SDS-PAGE. Digest proteins into peptides, desalt, and analyze by LC-MS/MS.
- Metabolomics Sample Prep: Precipitate proteins from 100 µL of bone marrow supernatant with ice-cold methanol-acetonitrile solution. Vortex, sonicate in an ice-water bath, centrifuge, and collect the supernatant for analysis.
- LC-MS/MS Analysis:
- Proteomics: Use a high-resolution LC-MS/MS system. Search spectra against a protein database (e.g., Swiss-Prot) using software like Spectronaut.
- Metabolomics: Perform untargeted LC-MS on an ACQUITY UPLC HSS T3 column coupled to a QE mass spectrometer. Identify metabolites by matching against databases like HMDB and METLIN.
II. Data Integration and Bioinformatic Analysis
- Perform unsupervised clustering (e.g., hierarchical clustering) on the protein and metabolite abundance data to identify intrinsic molecular subtypes.
- Correlate proteomic/metabolomic clusters with genetic mutation data (e.g., ASXL1, TP53, RUNX1) obtained via Next-Generation Sequencing (NGS).
- Use statistical analyses (t-tests, ANOVA) to identify proteins and metabolites significantly associated with clinical outcomes like relapse-free survival.
- Perform functional enrichment analysis (Gene Ontology, KEGG pathways) on the significant protein lists to interpret biological meaning [119].
Protocol 3: Robust Biomarker Discovery from Transcriptomic Data using Machine Learning (HCC Example)
This protocol outlines a computational pipeline for identifying robust and reproducible biomarker genes from high-throughput RNA-seq data, as demonstrated in HCC [122].
I. Data Preprocessing
- Data Acquisition: Download raw RNA-seq data (e.g., from TCGA LIHC project) containing tumor and matched normal samples.
- Normalization and Batch Effect Removal: Normalize raw count data using a method like the median of ratios in DESeq2. Remove batch effects as a covariate.
- Differential Expression Analysis: Identify a candidate gene pool by selecting genes that pass thresholds (e.g., FDR < 0.01, P value < 0.01, Fold Change > 3).
- Redundancy Reduction: Calculate pairwise Pearson’s correlation coefficients for all genes. If the correlation between two genes is > 0.65, remove the gene with the lower mean absolute value.
II. Wrapper-Based Feature Selection with Multiple Classifiers
- Algorithm Selection: Choose multiple machine learning classifiers (e.g., AdaBoost, K-Nearest Neighbors, Naive Bayes, Neural Network, Random Forest, Support Vector Machine).
- Recursive Feature Elimination-Cross Validation (RFE-CV):
- For each classifier, perform tenfold cross-validation to generate an overall importance ranking for every feature (gene).
- Iteratively remove the least important feature(s) and recalculate the model's classification accuracy at each step.
- For each classifier, select the feature subset that yields the highest classification accuracy with the least number of genes.
III. Identification of Robust Biomarkers
- Find Intersections: Identify the overlapping genes present in the optimal feature subsets selected by all (or most) of the different classifiers.
- Validation: These overlapping genes are proposed as robust biomarkers. Their biological relevance and performance can be further validated using independent datasets and functional analysis [122].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Tools for Biomarker Discovery Pipelines
| Item | Function/Application | Example Use Case |
|---|---|---|
| MARS Column (Hu-7) | Immunoaffinity depletion of high-abundance proteins from plasma/serum. | Enrichment of low-abundance candidate biomarkers in plasma proteomics [120]. |
| ZOOM-IEF Fractionator | Microscale solution-phase isoelectric focusing to fractionate complex protein mixtures by pH. | Increased proteome coverage by reducing sample complexity prior to 2-DGE or LC-MS [120]. |
| LC-MS/MS System | High-resolution tandem mass spectrometry for peptide/protein identification and quantification. | Core technology for untargeted (discovery) and targeted (validation) proteomics [118] [119]. |
| SEQUEST/MASCOT/X!Tandem | Database search algorithms for matching experimental MS/MS spectra to theoretical peptide sequences. | Protein identification from LC-MS/MS raw data [12] [123]. |
| Decoy Database | A database of reversed or randomized protein sequences used to estimate false discovery rate (FDR). | Critical for statistical validation and quality control in peptide/protein identification [123]. |
| RFE-CV (Machine Learning) | A wrapper feature selection method that recursively prunes features based on classifier performance via cross-validation. | Identification of robust, minimal gene signatures from high-dimensional transcriptomic data [122]. |
Workflow and Pathway Visualizations
Proteomic Biomarker Discovery Workflow
Diagram 1: A generalized workflow for mass spectrometry-based proteomic biomarker discovery, covering key stages from sample preparation to final validation.
Integrated Multi-Omic Analysis Pathway
Diagram 2: The integrated multi-omics workflow used in the AML relapse study, demonstrating how proteomic, metabolomic, and genetic data are combined to identify high-risk clusters and biomarkers.
Robust Computational Biomarker Discovery
Diagram 3: A computational pipeline for robust biomarker discovery using multiple machine learning classifiers and recursive feature elimination, culminating in a consensus, robust gene signature.
Conclusion
The pipeline from mass spectrometry data to a validated biomarker is a multi-stage, iterative process that hinges on rigorous experimental design, advanced analytical techniques, and stringent validation. Success is not defined by the number of initial candidates but by the translation of a specific and reliable signature into clinical utility. The future of biomarker discovery lies in integrating proteomics with other omics data, leveraging large-scale population studies, and adopting automated, high-throughput technologies. By adhering to established best practices and continuously incorporating technological innovations, researchers can overcome historical challenges and fully realize the promise of proteomics in precision medicine, leading to improved diagnostics, therapeutics, and patient outcomes.
References
- 1. and their applications - PMC Biomarker definitions [https://pmc.ncbi.nlm.nih.gov/articles/PMC5813875/]
- 2. Tutorial: best practices and considerations for mass-spectrometry-based protein biomarker discovery and validation | Nature Protocols [https://www.nature.com/articles/s41596-021-00566-6]
- 3. - Wikipedia Biomarker [https://en.wikipedia.org/wiki/Biomarker]
- 4. of Types and their applications | Abcam biomarkers [https://www.abcam.com/en-us/knowledge-center/immunology-and-infectious-disease/types-of-biomarkers-and-their-applications]
- 5. 7 Types of Biomarkers [https://www.atlasantibodies.com/knowledge-hub/blog/7-types-of-biomarkers/]
- 6. Mass spectrometry based biomarker discovery, verification, and validation — Quality assurance and control of protein biomarker assays - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5528535/]
- 7. Proteomic Workflows for Biomarker Identification Using Mass Spectrometry — Technical and Statistical Considerations during Initial Discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5302744/]
- 8. A Proteomics Pipeline for Generating Clinical Grade Biomarker Candidates from Data-Independent Acquisition Mass Spectrometry (DIA-MS) Discovery - PubMed [https://pubmed.ncbi.nlm.nih.gov/39432331/]
- 9. Machine learning pipeline to analyze clinical and proteomics data: experiences on a prostate cancer case | BMC Medical Informatics and Decision Making | Full Text [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-024-02491-6]
- 10. Tutorial: best practices and considerations for... | Nature Protocols [https://www.nature.com/articles/s41596-021-00566-6?error=cookies_not_supported&code=448a2cd2-a722-4f25-9b46-0a31e21d112b]
- 11. in Experimental Studies for... Design Proteomic Mass Spectrometry [https://link.springer.com/chapter/10.1007/978-981-97-5045-0_1]
- 12. Bioinformatics Methods for Mass Spectrometry-Based Proteomics Data Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7216093/]
- 13. Advances in proximal for disease fluid ... proteomics biomarker [https://pubmed.ncbi.nlm.nih.gov/21028795/]
- 14. Identification of brain-enriched proteins in the cerebrospinal fluid ... [https://clinicalproteomicsjournal.biomedcentral.com/articles/10.1186/s12014-016-9111-3]
- 15. Validation of lipidomic analysis of human plasma and serum by... [https://link.springer.com/article/10.1007/s00216-020-02473-3]
- 16. Analyzing Cerebrospinal Fluid Proteomes to Characterize Central Nervous System Disorders: A Highly Automated Mass Spectrometry-Based Pipeline for Biomarker Discovery - PubMed [https://pubmed.ncbi.nlm.nih.gov/30852817/]
- 17. (PDF) Mass Spectrometry (LC– MS / MS ) Identified Proteomic... [https://www.academia.edu/143540448/Mass_Spectrometry_LC_MS_MS_Identified_Proteomic_Biosignatures_of_Breast_Cancer_in_Proximal_Fluid]
- 18. ... | Nature Communications Plasma proteomics identify biomarkers [https://www.nature.com/articles/s41467-024-48961-3?error=cookies_not_supported]
- 19. -based Mass as an emerging tool in clinical... spectrometry proteomics [https://clinicalproteomicsjournal.biomedcentral.com/articles/10.1186/s12014-023-09424-x]
- 20. Identification of Clinical Biomarkers for Pre-Analytical Quality Control of Blood Samples - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3629782/]
- 21. Stability of the Human Plasma Proteome to Pre-analytical Variability as Assessed by an Aptamer-Based Approach - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8480202/]
- 22. Evaluating the effects of preanalytical variables on the stability of the human plasma proteome - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4492164/]
- 23. Exploring phlebotomy technique as a pre - analytical factor in... [https://pubmed.ncbi.nlm.nih.gov/26484650/]
- 24. reporting of Standardized - pre variables and analytical ... quality [https://pmc.ncbi.nlm.nih.gov/articles/PMC11863886/]
- 25. Quality Control in the Mass Spectrometry Proteomics Core: A Practical Primer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12051443/]
- 26. Acquisition Mode Showdown: DDA... - MetwareBio Mass Spectrometry [https://www.metwarebio.com/mass-spectrometry-acquisition-modes-dda-vs-dia-vs-mrm-vs-prm/]
- 27. Mass spectrometry based targeted protein quantification: methods and applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2657955/]
- 28. Coherent pipeline for biomarker using discovery ... mass [https://pmc.ncbi.nlm.nih.gov/articles/PMC2939613/]
- 29. Recent developments in mass-spectrometry-based targeted proteomics of clinical cancer biomarkers | Clinical Proteomics | Full Text [https://clinicalproteomicsjournal.biomedcentral.com/articles/10.1186/s12014-024-09452-1]
- 30. Protein and peptide fractionation, enrichment and depletion: tools for the complex proteome - PubMed [https://pubmed.ncbi.nlm.nih.gov/21241016/]
- 31. Depletion of Abundant Plasma Proteins and Limitations of Plasma Proteomics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2948641/]
- 32. ... | Thermo Fisher Scientific - US Proteomics Sample Preparation [https://www.thermofisher.com/us/en/home/clinical/clinical-translational-research/clinical-translational-research-learning-center/translational-research-information/proteomics-research-information/proteomics-sample-preparation-information.html]
- 33. Comparison of three methods for fractionation and enrichment of low molecular weight proteins for SELDI-TOF-MS differential analysis - PubMed [https://pubmed.ncbi.nlm.nih.gov/20685463/]
- 34. Sample Preparation Guide for Mass Spectrometry–Based Proteomics | Spectroscopy Online [https://www.spectroscopyonline.com/view/sample-preparation-guide-mass-spectrometry-based-proteomics]
- 35. Combination of automated sample preparation and micro-flow LC–MS for high-throughput plasma proteomics | Clinical Proteomics | Full Text [https://clinicalproteomicsjournal.biomedcentral.com/articles/10.1186/s12014-022-09390-w]
- 36. for micro-purification, Protocol , pre- enrichment and... fractionation [https://pubmed.ncbi.nlm.nih.gov/17703201/]
- 37. A Quick Guide to Proteomics For Sample ... Preparation Mass [https://www.preomics.com/blog/quick-guide-proteomics-sample-preparation]
- 38. Automated proteomic sample preparation: The key component for high throughput and quantitative mass spectrometry analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10339360/]
- 39. The clinical impact of recent advances in LC- MS for cancer biomarker ... [https://pubmed.ncbi.nlm.nih.gov/26581546/]
- 40. Proteomics approach and techniques in identification of reliable biomarkers for diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7042613/]
- 41. / iTRAQ , Label Free, TMT , DIA in DDA - Creative Proteomic Proteomics [https://www.creative-proteomics.com/subcell/itraqtmt-label-free-dia-dda-in-proteomic.htm]
- 42. An Overview of Mainstream Proteomics - MetwareBio Techniques [https://www.metwarebio.com/mainstream-proteomics-techniques-overview/]
- 43. of Quantitative Mass Spectrometric Methods for Drug... Comparison [https://pmc.ncbi.nlm.nih.gov/articles/PMC10407934/]
- 44. Isobaric quantification with DDA - quantms 1.6.0 documentation [https://docs.quantms.org/en/latest/iso.html]
- 45. List of mass spectrometry software - Wikipedia [https://en.wikipedia.org/wiki/List_of_mass_spectrometry_software]
- 46. - Data : A Milestone and Prospect in Clinical... Independent Acquisition [https://pmc.ncbi.nlm.nih.gov/articles/PMC11380018/]
- 47. Data-dependent vs. Data - independent Analysis Proteomic [https://www.technologynetworks.com/proteomics/lists/data-dependent-vs-data-independent-proteomic-analysis-331712]
- 48. What's the difference between DIA & DDA proteomics ? [https://blog.cellsignal.com/deep-proteome-profiling-with-dia]
- 49. Data-independent acquisition (DIA): an emerging proteomics technology for analysis of drug-metabolizing enzymes and transporters - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8674493/]
- 50. Navigating the Mass -Based Proteomic Spectrometry Using Free... Data [https://www.jove.com/t/68707/navigating-mass-spectrometry-based-proteomic-data-using-free]
- 51. Data Independent Acquisition (DIA) Data Analysis - Creative Proteomics [https://www.creative-proteomics.com/ngpro/data-independent-acquisition-dia-data-analysis.html]
- 52. Proteomic repository data submission, dissemination, and reuse: key messages - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7614296/]
- 53. MS Proteomics Preprocessing: Overview & Tools Data [https://bigomics.ch/blog/how-to-process-raw-mass-spectrometry-data-top-tools-for-proteomics-data/]
- 54. From Data to Discovery: Protein Identification and Quantification in... [https://www.metwarebio.com/protein-identification-quantification-ms-proteomics/]
- 55. Bioinformatics Pipeline Architecture [https://www.meegle.com/en_us/topics/bioinformatics-pipeline/bioinformatics-pipeline-architecture]
- 56. Reproducible, scalable, and shareable analysis pipelines with bioinformatics workflow managers | Nature Methods [https://www.nature.com/articles/s41592-021-01254-9]
- 57. Hands-on: Label-free data analysis using MaxQuant / Label-free data ... [https://training.galaxyproject.org/training-material/topics/proteomics/tutorials/maxquant-label-free/tutorial.html]
- 58. Clinical biomarker by SWATH- discovery based label-free... MS [https://pmc.ncbi.nlm.nih.gov/articles/PMC6545036/]
- 59. Frontiers | Variant biomarker using mass... discovery [https://www.frontiersin.org/journals/aging/articles/10.3389/fragi.2023.1191993/full]
- 60. Heat map - Wikipedia [https://en.wikipedia.org/wiki/Heat_map]
- 61. Heatmaps in Data Visualization: A Comprehensive Introduction - Inforiver [https://inforiver.com/insights/heatmaps-in-data-visualization-a-comprehensive-introduction/]
- 62. Application of machine to learning data: classification and... proteomics [https://pubmed.ncbi.nlm.nih.gov/24116388/]
- 63. Statistical Methods for Proteomic Biomarker Discovery based on Feature Extraction or Functional Modeling Approaches - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3693398/]
- 64. Application of Machine to Learning Data: Classification... Proteomics [https://pmc.ncbi.nlm.nih.gov/articles/PMC3837439/]
- 65. Overcoming the Dynamic in Plasma Proteomics Range Challenge [https://www.preomics.com/blog/overcoming-dynamic-range-challenge-plasma-proteomics]
- 66. Sample Preparation for Biofluids [https://www.biotage.com/biofluids-sample-prep]
- 67. A systematic evaluation of normalization methods in quantitative label-free proteomics - PubMed [https://pubmed.ncbi.nlm.nih.gov/27694351/]
- 68. Recommendations and Best Practices for Standardizing the Pre-Analytical Processing of Blood and Urine Samples in Metabolomics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7344701/]
- 69. Tutorial: best practices and considerations for... | Nature Protocols [https://www.nature.com/articles/s41596-021-00566-6?error=cookies_not_supported&code=8353164d-84b7-4aa5-9b4a-1119fe3814f8]
- 70. Assessing and mitigating in large-scale omics studies batch effects [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-024-03401-9]
- 71. Removing Batch from Longitudinal Gene Expression - Quantile... Effects [https://pubmed.ncbi.nlm.nih.gov/27272489/]
- 72. ProtPipe: A Multifunctional Data Analysis Pipeline for Proteomics and... [https://pubmed.ncbi.nlm.nih.gov/39576693/]
- 73. GitHub - MPUSP/snakemake-ms- proteomics : Pipeline for automatic... [https://github.com/MPUSP/snakemake-ms-proteomics]
- 74. through condition-based Improving ... reproducibility sensitivity [https://pmc.ncbi.nlm.nih.gov/articles/PMC11382186/]
- 75. Crossroads: Impact of Statistical Choices on... Reproducibility [https://pubmed.ncbi.nlm.nih.gov/41009792/]
- 76. Stability and reproducibility of proteomic profiles measured with an... [https://www.nature.com/articles/s41598-018-26640-w?error=cookies_not_supported&code=6a51505b-2cb6-4bcf-8095-a8607440a364]
- 77. Top Tips to Improve and Reproducibility in Solid Phase... Sensitivity [https://www.chromacademy.com/channels/sample-preparation/method-development/top-tips-to-improve-reproducibility-and-sensitivity-in-solid-phase-extraction/]
- 78. Assay Optimization 101: Enhancing Sensitivity , Specificity, and... [https://dispendix.com/blog/assay-optimization-101-enhancing-sensitivity-specificity-and-reproducibility]
- 79. An accessible workflow for high-sensitivity proteomics using parallel accumulation–serial fragmentation (PASEF) | Nature Protocols [https://www.nature.com/articles/s41596-024-01104-w]
- 80. Reproducible mass spectrometry data processing and compound annotation in MZmine 3 | Nature Protocols [https://www.nature.com/articles/s41596-024-00996-y]
- 81. 2.1 Mass spectrometry data handling and (pre-)processing | The MetaRbolomics book [https://rformassspectrometry.github.io/metaRbolomics-book/0201-R_packages_for_metabolomics-Mass_spectrometry_data_handling_and_pre_processing.html]
- 82. in MALDI-TOF serum protein profiles using... Biomarker discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC2647828/]
- 83. 5 Essential Strategies for Effective High - Dimensional Analysis Data [https://www.numberanalytics.com/blog/5-essential-strategies-high-dimensional-data-analysis]
- 84. The Relationship Between High and Dimensionality Overfitting [https://www.geeksforgeeks.org/machine-learning/the-relationship-between-high-dimensionality-and-overfitting/]
- 85. Tackling High - Dimensional : Proven Data Every Techniques ... Data [https://www.linkedin.com/pulse/tackling-high-dimensional-data-proven-techniques-every-bhosale--o2ief]
- 86. Mass Spectrometry Troubleshooting [https://www.numberanalytics.com/blog/mass-spectrometry-troubleshooting-guide]
- 87. - A Guide - GenTech Scientific Troubleshooting Mass Spectrometry [https://gentechscientific.com/a-guide-to-troubleshooting-mass-spectrometry/]
- 88. Pitfalls in Proteomics : Avoiding Problems That Can Occur Before Data... [https://www.chromatographyonline.com/view/pitfalls-in-proteomics-avoiding-problems-that-can-occur-before-data-acquisition-begins]
- 89. How to Avoid Problems in LC–MS | LCGC International [https://www.chromatographyonline.com/view/how-avoid-problems-lc-ms-0]
- 90. Standards and... | Thermo Fisher Scientific - CN Mass Spectrometry [https://www.thermofisher.cn/cn/en/home/technical-resources/technical-reference-library/mass-spectrometry-support-center/mass-spectrometry-reagents-support/ms-standards-calibrants-support/ms-standards-calibrants-support-troubleshooting.html]
- 91. Tips and tricks for successful Mass spec experiments | Proteintech Group [https://www.ptglab.com/news/blog/tips-and-tricks-for-successful-mass-spec-experiments/]
- 92. for Sample analysis using a GeLC-MS/MS... preparation proteomic [https://pmc.ncbi.nlm.nih.gov/articles/PMC4959781/]
- 93. What Is Targeted Quantitative Proteomics - Creative Proteomics [https://www.creative-proteomics.com/resource/what-is-targeted-quantitative-proteomics.htm]
- 94. Selected Reaction Monitoring - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/medicine-and-dentistry/selected-reaction-monitoring]
- 95. Proteomics Protein Quantitation Information | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/clinical/clinical-translational-research/clinical-translational-research-learning-center/translational-research-information/proteomics-research-information/proteomics-protein-quantitation-information.html]
- 96. Parallel Reaction Monitoring ( PRM ) in Mass ... Spectrometry [https://www.metwarebio.com/parallel-reaction-monitoring-prm-mass-spectrometry/]
- 97. Parallel Reaction Monitoring ( PRM ) Service - Creative Proteomics [https://www.creative-proteomics.com/services/parallel-reaction-monitoring-prm.htm]
- 98. Parallel reaction monitoring (PRM) and selected reaction monitoring (SRM) exhibit comparable linearity, dynamic range and precision for targeted quantitative HDL proteomics - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4259393/]
- 99. Targeted proteomics coming of age - SRM , PRM and DIA... [https://pubmed.ncbi.nlm.nih.gov/27130639/]
- 100. Plasma Proteomics: MS vs Affinity-Based Approaches | Technology Networks [https://www.technologynetworks.com/proteomics/articles/plasma-proteomics-with-professor-joshua-coon-399982]
- 101. Advantages of Mass Spectrometry Biomarker Discovery Proteomics [https://biognosys.com/advantages-mass-spectrometry-biomarker-discovery-proteomics/]
- 102. Comparative studies of 2168 plasma proteins measured by two affinity-based platforms in 4000 Chinese adults | Nature Communications [https://www.nature.com/articles/s41467-025-56935-2]
- 103. Large-scale plasma proteomics comparisons through genetics and disease associations | Nature [https://www.nature.com/articles/s41586-023-06563-x]
- 104. Proteomics Platform Showdown: MS-DIA vs. Olink vs. SomaScan - MetwareBio [https://www.metwarebio.com/proteomics-platform-comparison-ms-dia-olink-somascan/]
- 105. Current landscape of plasma proteomics from technical innovations to biological insights and biomarker discovery | Communications Chemistry [https://www.nature.com/articles/s42004-025-01665-1]
- 106. Integrated multi-dimensional comparison of proteomic profiles across 54 cancer cell lines - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483590/]
- 107. LC– MS - Based for Protein Proteomics Quantification for... Biomarker [https://www.chromatographyonline.com/view/lc-ms-based-proteomics-for-protein-biomarker-quantification-for-both-prognosis-and-diagnosis-in-the-clinical-setting]
- 108. landscape of Alzheimer’s disease: emerging technologies... Proteomic [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-025-00874-5]
- 109. Understanding ELISA Validation Parameters : Sensitivity , Specificity ... [https://synapse.patsnap.com/article/understanding-elisa-validation-parameters-sensitivity-specificity-and-beyond]
- 110. Development Techniques | News-Medical Assay [https://www.news-medical.net/life-sciences/Assay-Development-Techniques.aspx]
- 111. The interface between biomarker discovery and clinical validation: The tar pit of the protein biomarker pipeline - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2957839/]
- 112. Clinical proteomic biomarkers: relevant issues on study design & technical considerations in biomarker development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3994249/]
- 113. , Potential Pitfalls, and... | SpringerLink Data Analysis Pipelines [https://link.springer.com/chapter/10.1007/978-981-97-5045-0_7]
- 114. Label-free mass -based spectrometry for proteomics ... biomarker [https://pubmed.ncbi.nlm.nih.gov/22616700/]
- 115. Sample Size Determination for Clinical Proteomics Experiments: Diagnostic, Prognostic and Predictive Biomarker Discovery and Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3635338/]
- 116. Frontiers | Progress and trends on machine learning in proteomics during 1997-2024: a bibliometric analysis [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1594442/full]
- 117. Protein Biomarker Discovery & Validation [https://www.thermofisher.com/uk/en/home/clinical/clinical-translational-research/protein-analysis/protein-biomarker-discovery-validation.html]
- 118. Identification of Protein Biomarker Signatures for Acute ... Myeloid [https://pmc.ncbi.nlm.nih.gov/articles/PMC8628952/]
- 119. and metabolomic exploration in relapse Proteomic ... acute myeloid [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-024-13286-3]
- 120. 5D proteomic approach for the biomarker search in plasma: Acute ... [https://www.nature.com/articles/s41598-017-16699-2?error=cookies_not_supported]
- 121. Biomarker discovery in hepatocellular carcinoma (HCC) for personalized treatment and enhanced prognosis - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1359610124000674]
- 122. Robust biomarker discovery for hepatocellular carcinoma from high-throughput data by multiple feature selection methods | BMC Medical Genomics | Full Text [https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-021-00957-4]
- 123. An automated proteomic data analysis workflow for mass spectrometry - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3226188/]