Sensitivity and Specificity in DNA Methylation Detection: A 2025 Guide for Biomarker Validation and Clinical Translation
This article provides a comprehensive guide for researchers and drug development professionals on evaluating the sensitivity and specificity of DNA methylation detection methods.
Sensitivity and Specificity in DNA Methylation Detection: A 2025 Guide for Biomarker Validation and Clinical Translation
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on evaluating the sensitivity and specificity of DNA methylation detection methods. It covers foundational statistical concepts, performance characteristics of current technologies (including bisulfite sequencing, microarrays, EM-seq, and third-generation sequencing), strategies for troubleshooting and optimizing assays in real-world scenarios, and frameworks for rigorous validation and comparative analysis. With a focus on clinical application, the review also explores the growing role of machine learning in enhancing diagnostic accuracy and the pathway for translating methylation biomarkers into clinically viable tools for cancer diagnosis and monitoring.
Core Principles: Defining Sensitivity and Specificity in Epigenetic Analysis
In medical research and clinical practice, the evaluation of any diagnostic test relies on fundamental statistical metrics that determine its ability to correctly identify subjects with and without the target condition. Diagnostic accuracy provides the foundational framework for understanding test performance, guiding clinical decision-making, and advancing diagnostic technologies. For researchers, scientists, and drug development professionals, mastery of these metrics is essential for developing, validating, and implementing new diagnostic tools, particularly in emerging fields like molecular diagnostics and epigenetic testing.
The core metrics of sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) each provide distinct yet complementary information about test performance. These metrics are derived from a 2x2 contingency table that cross-references test results with true disease status, as determined by a reference standard. Understanding their individual definitions, calculations, interrelationships, and applications is crucial for accurately interpreting test results and assessing their clinical utility. This foundation becomes especially important when evaluating innovative detection methods, such as DNA methylation markers for cancer screening, where test performance must be rigorously characterized before clinical implementation.
Core Definitions and Clinical Interpretations
Foundational Metrics
The following table summarizes the four core diagnostic accuracy metrics, their definitions, and key clinical implications:
| Metric | Definition | Clinical Interpretation | Key Consideration |
|---|---|---|---|
| Sensitivity | Proportion of people with the disease who test positive [1] [2]. | A test's ability to correctly identify individuals who have the condition. A highly sensitive test is good at "ruling out" the disease when negative (SN-Out) [1]. | Independent of disease prevalence [1]. |
| Specificity | Proportion of people without the disease who test negative [1] [2]. | A test's ability to correctly identify individuals who do not have the condition. A highly specific test is good at "ruling in" the disease when positive (SP-In) [1]. | Independent of disease prevalence [1]. |
| Positive Predictive Value (PPV) | Proportion of people with a positive test who actually have the disease [1] [2]. | The probability that a patient with a positive test result truly has the disease. | Heavily influenced by disease prevalence [1] [3]. |
| Negative Predictive Value (NPV) | Proportion of people with a negative test who truly do not have the disease [1] [2]. | The probability that a patient with a negative test result is truly free of the disease. | Heavily influenced by disease prevalence [1] [3]. |
Statistical Formulas and the 2x2 Table
These metrics are calculated from a 2x2 contingency table that compares the test results against a reference standard. The standard table structure is visualized below, which forms the logical basis for all calculations.
The formulas derived from this table are fundamental for quantifying test performance [4] [2]:
- Sensitivity = True Positives (A) / [True Positives (A) + False Negatives (C)]
- Specificity = True Negatives (D) / [True Negatives (D) + False Positives (B)]
- Positive Predictive Value (PPV) = True Positives (A) / [True Positives (A) + False Positives (B)]
- Negative Predictive Value (NPV) = True Negatives (D) / [True Negatives (D) + False Negatives (C)]
Application in Methylation Detection Methods Research
DNA methylation analysis has emerged as a powerful tool for cancer detection and risk stratification. The performance of these epigenetic tests is evaluated using the standard diagnostic accuracy metrics, providing a clear framework for comparing different biomarker panels and methodologies.
Performance of Methylation Markers in Cervical Cancer Screening
Research has validated several DNA methylation markers as triage tests in high-risk human papillomavirus (hrHPV) positive populations for detecting cervical intraepithelial neoplasia grade 2 or worse (CIN2+). The following table summarizes published performance data for different methylation panels, illustrating the trade-offs between sensitivity and specificity.
| Methylation Marker Panel | Target Condition | Sensitivity | Specificity | PPV | NPV | Citation |
|---|---|---|---|---|---|---|
| C13orf18/EPB41L3/JAM3 | CIN2+ | 80% | 66% | 40% | 91% | [5] |
| SOX1/ZSCAN1 | CIN2+ | 63% | 84% | 40% | 93% | [5] |
| FAM19A4/miR124-2 | CIN2+ (vs. Positive Histology) | 50% | 87% | N/R | N/R | [6] |
| EPB41L3/JAM3 | CIN2+ | 68.7% | 96.7% | N/R | N/R | [7] |
N/R: Not explicitly reported in the cited study.
The data demonstrates that different marker panels offer varying diagnostic trade-offs. For instance, the C13orf18/EPB41L3/JAM3 panel offers higher sensitivity (80%) but lower specificity (66%), whereas the SOX1/ZSCAN1 panel offers lower sensitivity (63%) but higher specificity (84%) for detecting CIN2+ [5]. This inverse relationship between sensitivity and specificity is a common phenomenon in diagnostic testing. The high specificity of the EPB41L3/JAM3 panel (96.7%) makes it a promising triage tool to reduce unnecessary referrals and overtreatment in screening programs [7].
Impact of Disease Prevalence on Predictive Values
A critical concept in applying these metrics is that while sensitivity and specificity are considered intrinsic properties of a test, PPV and NPV are highly dependent on disease prevalence in the population being tested [1] [3]. This relationship has major implications for how a test performs across different clinical settings.
The following table illustrates how PPV and NPV change with prevalence for a hypothetical test with 90% sensitivity and 90% specificity:
| Prevalence | Positive Predictive Value (PPV) | Negative Predictive Value (NPV) |
|---|---|---|
| 1% | 8% | >99% |
| 10% | 50% | 99% |
| 20% | 69% | 97% |
| 50% | 90% | 90% |
Adapted from data illustrating the relationship between prevalence and predictive values [1].
As prevalence decreases, PPV decreases because there are more false positives for every true positive, a scenario described as "hunting for a needle in a haystack" [1]. Conversely, NPV increases as prevalence decreases because a negative result is more likely to be a true negative. This explains why a screening test used in a general, low-prevalence population may have a disappointingly low PPV, despite having high sensitivity and specificity. This principle is vividly demonstrated in real-world screening; for example, low-dose CT scans for lung cancer have high sensitivity (93.8%) and specificity (73.4%), but in a high-risk population with a cancer prevalence of 1.1%, the PPV was only 3.8%, meaning most positive results were false positives [3].
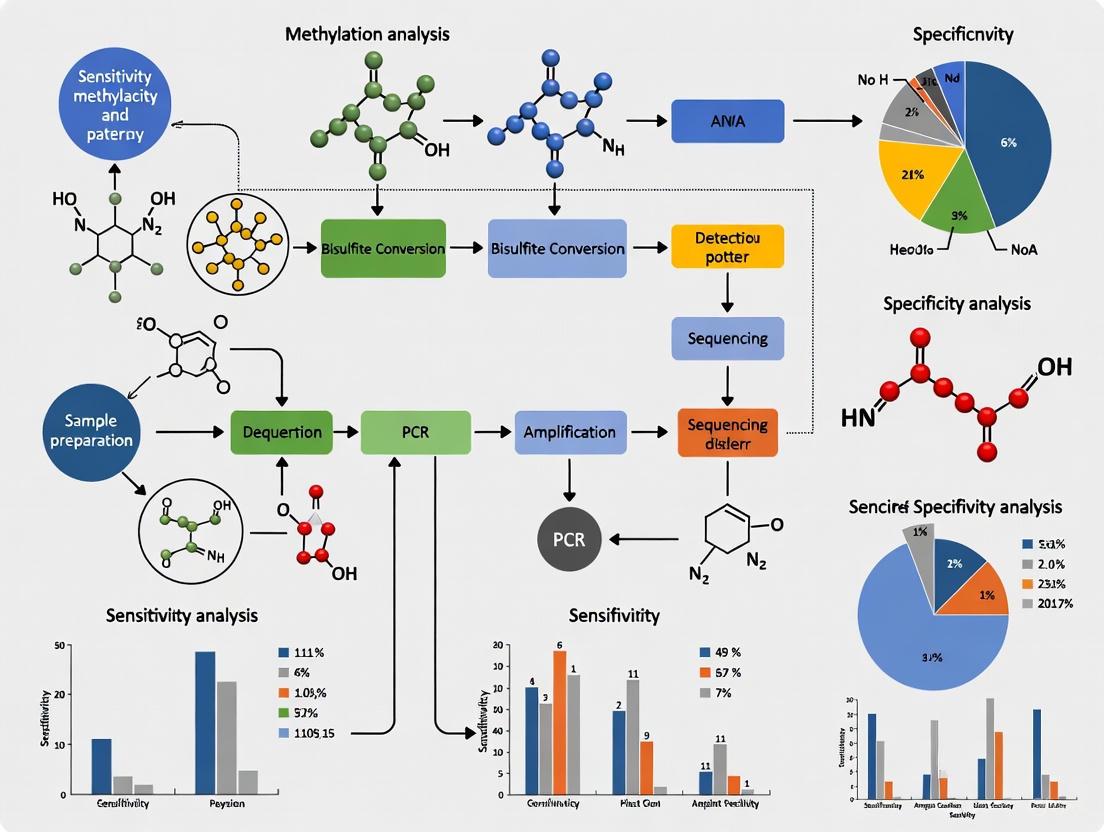
Experimental Protocols for Methylation Marker Validation
The validation of DNA methylation markers for clinical application involves a multi-step process to ensure robustness, reproducibility, and clinical utility. The workflow for such a study, from sample collection to data analysis, is outlined below.
Detailed Methodological Components
Population Selection and Sample Collection: Studies are typically conducted within a defined screening population. For example, a validation study for cervical dysplasia detection collected liquid-based cytology samples from patients before conization or hysterectomy, with subsequent histological confirmation serving as the reference standard [7]. Inclusion and exclusion criteria (e.g., age, HIV status, history of immunosuppression) must be clearly defined.
DNA Isolation and Bisulfite Treatment: DNA is isolated from cytology samples, often using phenol:chloroform:isoamylalcohol extraction and precipitation [5] or commercial kits like the QIAamp DNA Mini Kit [6]. A critical step is sodium bisulfite conversion, which deaminates unmethylated cytosine residues to uracil, while leaving methylated cytosines unchanged. This allows for the subsequent differentiation of methylated and unmethylated DNA sequences via PCR-based methods [5] [6]. The PreCursor-M+ kit protocol, for instance, uses bisulfite-converted DNA as its starting material [6].
Quantitative Methylation Analysis: The most common analytical method is quantitative Methylation-Specific PCR (qMSP). This technique uses primers and probes designed to specifically amplify either the methylated (converted) or unmethylated (unconverted) DNA sequence. The relative level of methylation is determined by comparing the quantity of the target amplicon to a reference gene (e.g., ACTB) to control for DNA input, often reported as a ΔCt value [5] [7]. A sample is classified as methylation-positive if its ΔCt value is below a pre-defined cutoff established in training sets [7].
Validation and Statistical Analysis: Test performance is evaluated by comparing methylation results against the reference standard diagnosis (e.g., CIN2+ confirmed by histology [7]). Sensitivity, specificity, PPV, and NPV are calculated using the standard formulas. The diagnostic accuracy of methylation testing is often directly compared to established methods, such as hrHPV testing, to assess its potential value as a primary screening or triage tool [6] [7].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents, kits, and instruments essential for conducting DNA methylation analysis research, as cited in the literature.
| Item Name/Type | Specific Function in Methylation Analysis | Example Product/Model |
|---|---|---|
| DNA Extraction Kit | Isolation of high-quality genomic DNA from clinical samples (e.g., cervical scrapings, liquid-based cytology). | QIAamp DNA Mini Kit [6] |
| Bisulfite Conversion Kit | Chemical treatment of DNA that converts unmethylated cytosines to uracils, enabling methylation status discrimination. | EZ DNA Methylation Kit (Zymo Research) [5] [6] |
| Quantitative PCR System | Platform for performing real-time PCR to amplify and detect methylated DNA sequences with high sensitivity. | ABI 7300/7500 Real-Time PCR System [7] |
| Methylation-Specific Detection Kit | Contains optimized primers and probes for targeted amplification of specific methylated genes. | PreCursor-M+ Kit (for FAM19A4/miR124-2) [6]; Methylated Human EPB43/JAM3 Gene Detection Kit [7] |
| DNA Quantitation Assay | Accurate measurement of DNA concentration prior to bisulfite conversion and PCR to ensure standardized input. | Qubit dsDNA BR Assay Kit [6] |
| Reference Standard Assay | Provides the definitive diagnosis against which the new test is validated (e.g., histology for cancer). | Histopathological examination [5] [7] |
The metrics of sensitivity, specificity, PPV, and NPV form an indispensable framework for evaluating diagnostic tests. While sensitivity and specificity describe the intrinsic performance of a test, PPV and NPV reveal its practical clinical value in a specific population, heavily influenced by disease prevalence. The application of these metrics in cutting-edge fields like DNA methylation research for cancer detection allows for the objective comparison of novel biomarker panels, guiding the development of more accurate and efficient diagnostic strategies. A thorough understanding of these principles, combined with rigorous experimental validation, is paramount for researchers and drug development professionals aiming to translate promising biomarkers from the laboratory into clinically useful tools that improve patient outcomes.
The Critical Role of a Gold Standard in Methylation Biomarker Validation
In the rapidly evolving field of cancer diagnostics, DNA methylation biomarkers have emerged as powerful tools for early detection, prognosis, and monitoring treatment response. These epigenetic modifications, which involve the addition of a methyl group to cytosine bases in CpG dinucleotides, offer exceptional stability and are frequently altered in cancer cells [8]. The journey from biomarker discovery to clinical implementation, however, is complex and requires rigorous validation against established standards. This guide examines the critical role of gold standard methodologies in validating DNA methylation biomarkers, comparing performance metrics across technologies and sample types to inform researchers and drug development professionals engaged in sensitivity-specificity analysis of methylation detection methods.
Defining the Gold Standard in Methylation Analysis
In biomarker validation, a "gold standard" refers to the benchmark method or reference against which new tests are evaluated. For DNA methylation analysis, this encompasses multiple dimensions including the reference materials, analytical methodologies, and clinical outcomes that establish the ground truth.
The biological gold standard for cancer diagnosis remains the tissue biopsy, which provides direct morphological confirmation of disease alongside molecular data [9]. For methylation-specific studies, bisulfite sequencing is widely regarded as the reference method for base-resolution methylation mapping, with Whole-Genome Bisulfite Sequencing (WGBS) providing the most comprehensive coverage [8] [9]. The bisulfite conversion process chemically deaminates unmethylated cytosines to uracils while leaving methylated cytosines unchanged, allowing for precise mapping of methylation status at single-base resolution [9].
Emerging technologies such as Enzymatic Methyl-Sequencing (EM-seq) offer compelling alternatives by using enzymes rather than bisulfite to detect methylation status, thereby preserving DNA integrity—a critical advantage when working with limited liquid biopsy samples [8]. Third-generation sequencing technologies including nanopore and single-molecule real-time sequencing further expand the methodological landscape by enabling direct detection of methylation without conversion steps [8].
Essential Metrics for Biomarker Validation
Robust validation of methylation biomarkers requires assessment across multiple performance dimensions. The following metrics represent the core framework for evaluating clinical utility:
- Analytical Sensitivity: The lowest concentration of a methylated target (e.g., variant allele fraction) that can be reliably detected, crucial for early cancer detection when ctDNA fractions may be below 1% [8] [9].
- Analytical Specificity: The ability to distinguish true methylation signals from background noise and cross-reactivity with similar sequences.
- Diagnostic Sensitivity: The proportion of true positive cases correctly identified by the biomarker test.
- Diagnostic Specificity: The proportion of true negative cases correctly identified by the biomarker test.
- Reproducibility: Consistency of results across different operators, instruments, and laboratories.
- Area Under the Curve (AUC): Overall measure of diagnostic performance across all classification thresholds.
Comparative Performance of Methylation Detection Methods
The selection of methylation analysis technology significantly impacts performance characteristics, cost, and scalability. The table below summarizes key methodologies and their applications in biomarker validation.
Table 1: Comparison of DNA Methylation Analysis Technologies
| Method | Resolution | Throughput | Advantages | Limitations | Best Applications |
|---|---|---|---|---|---|
| Whole-Genome Bisulfite Sequencing (WGBS) | Single-base | High | Comprehensive genome-wide coverage; discovery of novel biomarkers [8] | High cost; computational complexity; DNA degradation from bisulfite [8] | Biomarker discovery; reference method validation |
| Reduced Representation Bisulfite Sequencing (RRBS) | Single-base (CpG-rich regions) | Medium | Cost-effective; focuses on CpG islands [8] | Limited genome coverage | Targeted discovery; cancer-specific methylation profiling |
| Methylation Microarrays | Pre-defined CpG sites | High | Cost-effective for large cohorts; well-established analysis pipelines [8] | Limited to pre-designed content; cannot discover novel sites | Large-scale clinical validation studies |
| Enzymatic Methyl-Sequencing (EM-seq) | Single-base | High | Better DNA preservation than bisulfite methods [8] | newer method with less established protocols | Liquid biopsy applications with limited input material |
| Digital PCR (dPCR) | Locus-specific | Low | Absolute quantification; high sensitivity for low-abundance targets [8] | Limited to known targets; low multiplexing capability | Clinical validation; monitoring minimal residual disease |
| Methylation-Specific PCR (qMSP) | Locus-specific | High | Simple; cost-effective; high sensitivity [10] | Qualitative/semi-quantitative; prone to false positives without careful optimization | Clinical assay development; high-throughput screening |
Experimental Workflows for Biomarker Validation
A robust validation framework for methylation biomarkers follows a structured pathway from discovery to clinical implementation. The diagram below illustrates this multi-stage process.
Gold Standard Biomarker Panels in Clinical Development
Several methylation biomarker panels have advanced through rigorous validation and demonstrate the performance achievable with comprehensive development. The table below highlights representative examples across cancer types.
Table 2: Clinically Validated Methylation Biomarker Panels
| Cancer Type | Biomarker Panel | Sample Type | Performance | Validation Status |
|---|---|---|---|---|
| Colorectal Cancer | SDC2, SFRP2, SEPT9 [9] | Feces, Blood [9] | Sensitivity: 86.4%\nSpecificity: 90.7% (ColonSecure study) [9] | FDA-approved (Epi proColon) and Breakthrough Devices (Shield) [8] |
| Prostate Cancer | GSTP1, CCND2, APC, RASSF1 [10] | Tissue, Liquid Biopsy [10] | AUC: 0.937 (GSTP1 + CCND2 combination) [10] | Multiple panels in validation; tissue confirmed |
| Breast Cancer | 15-marker ctDNA panel [9] | Blood (ctDNA) [9] | AUC: 0.971 [9] | Discovery and initial validation |
| Bladder Cancer | CFTR, SALL3, TWIST1 [9] | Urine [9] | Superior sensitivity in urine vs. blood [8] | FDA Breakthrough Device designation [8] |
| Esophageal Squamous Cell Carcinoma | 12-CpG panel [9] | Tissue [9] | AUC: 0.966 [9] | TCGA data validation |
| Multiple Cancers | Multi-cancer early detection test [8] | Blood (plasma) [8] | Varies by cancer type and stage | FDA Breakthrough Device (Galleri, OverC) [8] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful methylation biomarker validation requires carefully selected reagents and platforms. The following table details essential components of the methylation researcher's toolkit.
Table 3: Essential Research Reagents and Materials for Methylation Analysis
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Bisulfite Conversion Kit | Chemical conversion of unmethylated cytosines to uracils | Critical step for bisulfite-based methods; optimized kits minimize DNA degradation [9] |
| DNA Methyltransferases (DNMTs) | Enzymes for methylation detection in enzyme-based methods | DNMT1, DNMT3A, DNMT3B for maintenance and de novo methylation studies [10] |
| Methylation-Specific Restriction Enzymes | Cleavage at specific methylation patterns | Used in enrichment-based methods like MeDIP-seq [8] |
| MethylBinding Domain (MBD) Proteins | Enrichment of methylated DNA fragments | Used in MBD-seq and related capture techniques [8] |
| Digital PCR Master Mix | Absolute quantification of methylated alleles | Essential for high-sensitivity detection of low-frequency methylation events in liquid biopsies [8] |
| Bisulfite-Treated Control DNA | Positive and negative controls for assay validation | Commercially available fully methylated and unmethylated DNA standards |
| Next-Generation Sequencing Library Prep Kits | Preparation of bisulfite or enzyme-converted DNA for sequencing | Specialized kits account for reduced sequence complexity post-conversion |
| Cell-Free DNA Collection Tubes | Stabilization of blood samples for liquid biopsy | Preserves ctDNA profile; critical for multi-center clinical trials [8] |
Method Selection Framework for Validation Studies
Choosing the appropriate methodology depends on the specific validation objectives, sample type, and resource constraints. The decision pathway below provides guidance for method selection.
The validation of DNA methylation biomarkers against rigorous gold standards remains fundamental to translating epigenetic discoveries into clinically impactful tools. As detection technologies evolve and liquid biopsy applications expand, maintaining stringent validation frameworks becomes increasingly critical. Researchers must carefully match method selection to validation objectives, from initial discovery using comprehensive sequencing approaches to clinical implementation with targeted, high-sensitivity platforms. The continued refinement of both analytical methods and clinical validation pathways will accelerate the adoption of methylation biomarkers in precision oncology, ultimately improving early cancer detection, monitoring, and patient outcomes.
In the pursuit of diagnostic accuracy, researchers and clinicians have long relied on heuristic tools to quickly interpret test results. Among the most recognized are SnNOut (Sensitive, Negative, Rule OUT) and SpPIn (Specific, Positive, Rule IN), mnemonics that provide a simplified framework for diagnostic reasoning [11]. These rules propose that a highly sensitive test, when negative, can effectively rule out a disease, while a highly specific test, when positive, can rule it in [12]. For decades, these principles have been taught in evidence-based medicine and remain deeply embedded in clinical practice and research methodology.
The application of these diagnostic rules extends beyond traditional clinical settings into advanced research domains, including methylation detection methods and epigenetics research. In molecular diagnostics, accurately interpreting the results of assays that detect methylation patterns—crucial for understanding gene expression regulation in cancer development, neurological disorders, and drug response—requires a sophisticated understanding of test performance characteristics [13]. As researchers develop increasingly refined epigenetic biomarkers, the limitations of simplistic diagnostic heuristics become more apparent, necessitating a more nuanced approach to diagnostic test interpretation that incorporates pretest probability, likelihood ratios, and the specific research context [14] [15].
Fundamental Concepts and Definitions
Sensitivity and Specificity
Sensitivity and specificity are foundational biometric parameters that describe the inherent accuracy of a diagnostic test. Sensitivity (true positive rate) measures a test's ability to correctly identify individuals who have the disease, calculated as the proportion of diseased individuals who test positive [12] [16]. Mathematically, sensitivity = True Positives/(True Positives + False Negatives). A test with 95% sensitivity will detect 95 of 100 truly diseased individuals, missing 5 (false negatives).
Specificity (true negative rate) measures a test's ability to correctly identify individuals without the disease, calculated as the proportion of non-diseased individuals who test negative [12] [16]. Mathematically, specificity = True Negatives/(True Negatives + False Positives). A test with 90% specificity will correctly classify 90 of 100 healthy individuals, while incorrectly classifying 10 healthy individuals as diseased (false positives).
These characteristics are typically represented in a 2x2 contingency table that cross-tabulates test results with true disease status:
Table 1: Standard 2x2 Contingency Table for Diagnostic Test Evaluation
| Disease Present | Disease Absent | |
|---|---|---|
| Test Positive | True Positive (A) | False Positive (B) |
| Test Negative | False Negative (C) | True Negative (D) |
SnNOut and SpPIn Rules
The SnNOut mnemonic encapsulates the principle that when a test with high Sensitivity returns a Negative result, it can rule Out the target condition [11] [12]. This rule is clinically valuable because a highly sensitive test rarely misses individuals with the disease, so a negative result provides confidence that the disease is absent.
The SpPIn mnemonic encapsulates the principle that when a test with high Specificity returns a Positive result, it can rule In the target condition [11] [12]. This is valuable because a highly specific test rarely incorrectly labels healthy individuals as diseased, so a positive result strongly suggests the disease is present.
Table 2: Examples of Tests with SnNOut and SpPIn Properties
| Test | Target Condition | Sensitivity | Specificity | Clinical Rule |
|---|---|---|---|---|
| Ottawa Ankle Rules [12] | Ankle or midfoot fracture | 99% (92-100%) | 39% (34-45%) | SnNOut (negative test rules out fracture) |
| CAGE Questionnaire (≥3 positives) [11] | Alcohol dependence | Not specified | >99% | SpPIn (positive test rules in alcoholism) |
| Loss of retinal vein pulsation [11] [12] | Increased intracranial pressure | 100% (92-100%) | 88% (81-93%) | SnNOut (presence of pulsation rules out increased ICP) |
Figure 1: This decision pathway illustrates the clinical application of SpPIn and SnNOut rules. The process begins with evaluating a test's sensitivity and specificity characteristics, then applying the appropriate heuristic based on the test result. Note that these rules only apply when tests demonstrate appropriately high sensitivity or specificity values.
Critical Limitations and Methodological Challenges
Fundamental Statistical Flaws
Despite their widespread adoption, SpPIn and SnNOut present significant limitations that can lead to diagnostic errors. A primary concern is that neither sensitivity nor specificity should be considered in isolation when evaluating a test's diagnostic utility [14]. These characteristics represent interdependent aspects of test performance, and focusing on one while ignoring the other provides an incomplete picture.
Research demonstrates that a test's utility for ruling in or ruling out disease depends fundamentally on the post-test probability rather than isolated sensitivity or specificity values [14]. The following comparison illustrates this critical limitation:
Table 3: Test Performance Comparison Demonstrating Flaw in SpPIn/SnNOut Logic
| Test | Sensitivity | Specificity | LR+ | LR- | SpPIn Recommendation | SnNOut Recommendation | Actual Best Test For |
|---|---|---|---|---|---|---|---|
| Test A | 30% | 95% | 6.0 | 0.74 | Yes (rules in) | No | Neither |
| Test B | 95% | 30% | 1.4 | 0.17 | No | Yes (rules out) | Neither |
| Test C | 90% | 90% | 9.0 | 0.11 | No | No | Both ruling in and out |
As shown in Table 3, SpPIn would incorrectly identify Test A as best for ruling in disease (due to highest specificity), while SnNOut would incorrectly identify Test B as best for ruling out disease (due to highest sensitivity). In reality, Test C outperforms both for ruling in and ruling out disease because it generates both the highest post-test probability when positive (due to LR+ = 9.0) and the lowest post-test probability when negative (due to LR- = 0.11) [14].
Pretest Probability and Prevalence Effects
The pretest probability (prevalence) of a condition substantially influences the predictive values of diagnostic tests, creating a critical limitation for SpPIn and SnNOut that these heuristics fail to address [15] [17]. Even tests with apparently excellent sensitivity and specificity characteristics can perform poorly when disease prevalence is very low or very high.
A compelling example comes from COVID-19 antibody testing during the pandemic. With a test demonstrating 99% sensitivity and 99% specificity, and a population prevalence of 0.541%, the positive predictive value (PPV) would be only 35% despite the high specificity [17]. This means that only 35% of positive test results would represent true infections, making the test inadequate for "ruling in" prior infection despite the seemingly high specificity that would suggest SpPIn applicability.
The mathematical relationship between prevalence and predictive values can be expressed as:
- Positive Predictive Value (PPV) = (Sensitivity × Prevalence) / [(Sensitivity × Prevalence) + (1 - Specificity) × (1 - Prevalence)]
- Negative Predictive Value (NPV) = [Specificity × (1 - Prevalence)] / [(Specificity × (1 - Prevalence)) + (1 - Sensitivity) × Prevalence]
This demonstrates that as prevalence decreases, PPV decreases (more false positives), and as prevalence increases, NPV decreases (more false negatives) [15].
Problems with Test Dichotomization
Most diagnostic tests in practice are not truly dichotomous but exist on a spectrum of possible results [14]. Physical exam maneuvers often have ordinal outcomes (e.g., "negative," "indeterminate," "positive"), while laboratory tests typically produce continuous numerical values. The process of dichotomizing these continuous or multilevel test results into simple positive/negative categories introduces measurement error and discards valuable diagnostic information.
Research on ultrasound measurement of jugular venous pressure exemplifies this limitation. When dichotomized, the test demonstrated modest sensitivity (73%) and specificity (79%), with likelihood ratios that would not be considered particularly helpful (LR+ = 3.4, LR- = 0.34) [14]. However, when analyzed as six distinct levels of test results, the likelihood ratios ranged from zero to infinity, revealing substantially more diagnostic utility than apparent from the dichotomized approach [14].
In molecular diagnostics, including methylation detection methods, this limitation is particularly relevant. Methylation levels typically exist on a continuous spectrum, and dichotomizing results into "methylated" or "unmethylated" categories may obscure clinically significant patterns and reduce test accuracy [13].
Advanced Diagnostic Interpretation Frameworks
Likelihood Ratios and Bayesian Analysis
Likelihood ratios (LRs) provide a superior framework for diagnostic test interpretation as they incorporate both sensitivity and specificity into a single measure that can be directly applied to modify disease probability [14] [15] [18]. The likelihood ratio for a given test result represents the probability of that result among patients with the disease divided by the probability of the same result among patients without the disease.
The fundamental Bayesian equation for diagnostic test interpretation is:
Pretest Odds × Likelihood Ratio = Posttest Odds
This calculation can be simplified using a nomogram or online calculators, eliminating the need for manual probability-odds conversions [14]. Likelihood ratios are interpreted according to their magnitude:
Table 4: Interpretation of Likelihood Ratios for Diagnostic Test Results
| LR Value | Interpretation | Effect on Posttest Probability |
|---|---|---|
| >10 | Large increase | Conclusive shift |
| 5-10 | Moderate increase | Moderate shift |
| 2-5 | Small increase | Small but sometimes important shift |
| 1-2 | Minimal change | Rarely important |
| 0.5-1 | Minimal change | Rarely important |
| 0.1-0.5 | Small decrease | Small but sometimes important shift |
| 0.1-0.2 | Moderate decrease | Moderate shift |
| <0.1 | Large decrease | Conclusive shift |
Research Methodology and Experimental Protocols
Implementing robust diagnostic accuracy studies requires careful methodological planning to minimize bias and maximize generalizability. Key considerations include:
Optimal Study Design: The prospective cohort study represents the optimal design for diagnostic accuracy research, wherein the test(s) and reference standard undergo prospective blind comparison in a clinically relevant patient sample [16]. This design minimizes verification bias and ensures the results reflect real-world application.
Sample Size and Power Considerations: Most diagnostic accuracy studies are underpowered, compromising the precision of sensitivity and specificity estimates [18]. Appropriate power calculations must be conducted a priori to ensure sufficient participants are enrolled. For example, a study aiming to demonstrate 95% sensitivity with a 90% lower confidence limit would require approximately 298 participants [18].
Reference Standard Application: The reference standard must be applied consistently to all study participants, independent of the diagnostic test results, with blinding maintained between test and reference standard interpreters [16].
Spectrum of Participants: The study population should represent the full spectrum of patients on whom the test will be used in practice, including mild, moderate, and severe cases, to avoid spectrum bias that inflates accuracy measures [12].
Figure 2: Recommended workflow for conducting diagnostic test accuracy studies, emphasizing methodological rigor to minimize bias and maximize the clinical applicability of findings.
Essential Research Reagents and Materials
Table 5: Key Research Reagent Solutions for Diagnostic Test Evaluation
| Reagent/Resource | Function | Application Context |
|---|---|---|
| Reference Standard Test | Provides definitive disease classification | Gold standard comparison for new index tests |
| DNA Methylation Arrays | Genome-wide methylation profiling | Epigenetic association studies [13] |
| Linear Mixed Effect Models | Accounts for familial correlations in data | Genetic and epigenetic studies with related participants [13] |
| QUADAS-2 Tool | Quality assessment of diagnostic accuracy studies | Methodological quality appraisal [18] |
| Statistical Software (R, Python) | Data analysis and accuracy metric calculation | All statistical analyses and visualization |
| Sample Size Calculation Tables | Determines minimum participant numbers | Study design phase to ensure adequate power [18] |
| Online Nomograms/Calculators | Bayesian probability revision | Clinical application of likelihood ratios [14] |
The SnNOut and SpPIn rules, while mnemonically appealing and easily remembered, present significant limitations for modern diagnostic practice and research. These heuristics fail to account for the critical influences of pretest probability, the interdependent nature of sensitivity and specificity, and the continuous nature of most diagnostic tests. In molecular research, including methylation detection methodologies, these limitations are particularly problematic given the subtle and continuous nature of epigenetic markers.
A superior approach incorporates likelihood ratios within a Bayesian framework, enabling quantitative revision of disease probability based on test results while considering both test characteristics and population context [14] [18]. Additionally, researchers should avoid arbitrary dichotomization of continuous test results, instead preserving multiple test thresholds or utilizing the full spectrum of values to maximize diagnostic information [14] [13].
As diagnostic technologies evolve, particularly in epigenetic research where methylation patterns serve as biomarkers for disease detection, prognosis, and therapeutic monitoring, moving beyond simplistic heuristics toward more sophisticated probabilistic reasoning becomes increasingly essential for accurate diagnosis and effective patient management.
DNA methylation, the process of adding a methyl group to a cytosine base in DNA, has emerged as a cornerstone of cancer biomarker research. This epigenetic modification regulates gene expression without altering the underlying DNA sequence and possesses three fundamental properties that make it exceptionally powerful for clinical applications: inherent molecular stability, early appearance during carcinogenesis, and convenient detectability in liquid biopsies. For researchers and drug development professionals, understanding these properties is crucial for developing the next generation of cancer diagnostics and monitoring tools. The stability of the DNA molecule itself, combined with the cancer-specific nature of methylation patterns, provides a robust foundation for assays that can detect malignancies years before clinical symptoms manifest [8] [19]. This review systematically examines the evidence supporting methylation's biomarker utility, compares detection methodologies, and provides practical experimental guidance for leveraging this powerful tool in cancer research.
Key Properties of DNA Methylation as a Biomarker
Exceptional Biological Stability
The stability of DNA methylation biomarkers operates on two distinct levels: molecular and pattern stability. The DNA double helix provides structural stability far superior to single-stranded nucleic acids or proteins, protecting methylated cytosines from degradation during sample collection, storage, and processing [8]. This molecular resilience is particularly valuable for liquid biopsy applications where circulating tumor DNA (ctDNA) fragments are subject to rapid clearance from the bloodstream, with half-lives estimated from minutes to a few hours [8].
Longitudinal studies have demonstrated that while the blood methylome shows considerable dynamism over time, a specific subset of methylation sites exhibits remarkable temporal stability. A comprehensive 2024 analysis of blood DNA methylation across three cohorts revealed that out of thousands of probes analyzed, 239 highly stable probes were identified that maintained consistent methylation patterns over periods exceeding one year, with an intraclass correlation coefficient (ICC) >0.74 and mean absolute difference <0.01 [20]. These stable probes were predominantly influenced by genomic variation, suggesting that genetics provides a stable foundation upon which methylation biomarkers can be built for reliable longitudinal monitoring.
Early Appearance in Carcinogenesis
DNA methylation alterations represent some of the earliest molecular events in cancer development, often preceding clinical diagnosis by several years. The potential for early detection was dramatically demonstrated in the Taizhou Longitudinal Study, where the PanSeer assay detected methylation changes in five common cancer types (stomach, esophageal, colorectal, lung, and liver) up to four years before conventional diagnosis with 95% sensitivity in asymptomatic individuals who later developed cancer [19].
The biological basis for this early appearance lies in the fundamental role DNA methylation plays in tumor initiation. Two complementary patterns emerge early in carcinogenesis: global hypomethylation, which leads to genomic instability and oncogene activation, and focal hypermethylation of CpG islands in promoter regions of tumor suppressor genes, resulting in their transcriptional silencing [21] [22] [23]. These changes occur during the precancerous or early cancer stages [9], making them ideal sentinels for identifying molecular transformations long before they manifest as clinically detectable tumors.
Detectability in Liquid Biopsies
The advent of liquid biopsy platforms has revolutionized cancer detection by enabling non-invasive access to tumor-derived genetic material. DNA methylation biomarkers are particularly well-suited for liquid biopsy applications due to several advantageous properties. Methylation patterns can be detected in extremely low concentrations of circulating tumor DNA, with advanced methods like the PanSeer assay demonstrating detection capability at cancer DNA fractions as low as 0.1% [19].
Different bodily fluids offer varying advantages for methylation-based detection, often related to anatomical proximity to the tumor origin. For example, urine shows superior performance for bladder cancer detection, with one study reporting 87% sensitivity for mutation detection in urine versus only 7% in plasma [8]. Similarly, bile outperforms plasma for biliary tract cancers, stool provides superior detection for colorectal cancer, and cerebrospinal fluid offers enhanced sensitivity for central nervous system malignancies [8]. This principle of "local liquid biopsy" sources often provides higher biomarker concentration and reduced background noise compared to systemic blood samples.
Table 1: Comparison of Liquid Biopsy Sources for Methylation Biomarker Detection
| Liquid Biopsy Source | Advantages | Ideal Cancer Applications | Detection Sensitivity Examples |
|---|---|---|---|
| Blood (Plasma) | Systemic circulation, captures tumors regardless of location | Multi-cancer early detection, monitoring | PanSeer: 88% detection for 5 cancers post-diagnosis [19] |
| Urine | Fully non-invasive, high patient compliance | Bladder, prostate, renal cancers | TERT mutations: 87% sensitivity in urine vs 7% in plasma [8] |
| Sputum | Direct contact with respiratory epithelium | Lung cancer | SHOX2 methylation: 67% sensitivity at 90% specificity [22] |
| Stool | Direct sampling of gastrointestinal tract | Colorectal cancer | Cologuard: 92.3% sensitivity for cancer detection [24] |
| Bile | Anatomical proximity to hepatobiliary system | Cholangiocarcinoma, liver cancer | Superior mutation detection vs plasma [8] |
Methylation Biomarkers Across Cancer Types
Extensive research has identified specific DNA methylation biomarkers with demonstrated clinical utility across numerous cancer types. The table below summarizes well-validated methylation markers and their performance characteristics in different sample types.
Table 2: Validated DNA Methylation Biomarkers Across Different Cancers
| Cancer Type | Methylation Biomarkers | Sample Type | Performance Metrics | References |
|---|---|---|---|---|
| Lung Cancer | SHOX2, RASSF1A, DAPK, MGMT | Plasma, sputum, BALF | SHOX2: 67% sensitivity at 90% specificity; RASSF1A panel: 73% sensitivity, 82% specificity [21] [22] | |
| Colorectal Cancer | SEPT9, SDC2, BMP3, NDRG4 | Blood, stool | mSEPT9: pooled sensitivity 0.69, specificity 0.92; SDC2: sensitivity 0.81, specificity 0.95 [9] [24] | |
| Breast Cancer | TRDJ3, PLXNA4, KLRD1, KLRK1 | PBMC, tissue, blood | 4-marker panel: 93.2% sensitivity, 90.4% specificity [9] | |
| Bladder Cancer | CFTR, SALL3, TWIST1 | Urine | Multiple studies showing high sensitivity in urine samples [9] | |
| Liver Cancer | SEPT9, BMPR1A, PLAC8 | Tissue, blood | Varies by marker and study [9] | |
| Pancreatic Cancer | PRKCB, KLRG2, ADAMTS1, BNC1 | Tissue, blood | Varies by marker and study [9] |
The clinical translation of these biomarkers is already underway, with several methylation-based tests receiving regulatory approval. Examples include Epi proColon and Cologuard for colorectal cancer screening, and Shield and Galleri which have received FDA Breakthrough Device designation [8] [24]. The ongoing development of multi-cancer early detection (MCED) tests represents perhaps the most promising application, with the potential to revolutionize cancer screening paradigms.
Detection Technologies and Methodologies
Comparison of Methylation Analysis Methods
The selection of appropriate detection methodology is critical for successful methylation biomarker research. The table below compares the major categories of DNA methylation analysis techniques, each with distinct advantages and limitations for specific applications.
Table 3: DNA Methylation Detection Technologies and Their Characteristics
| Method Category | Specific Techniques | Resolution | Advantages | Disadvantages | Best Applications |
|---|---|---|---|---|---|
| Bisulfite Conversion-Based | Whole-genome bisulfite sequencing (WGBS), Reduced Representation Bisulfite Sequencing (RRBS), Bisulfite pyrosequencing | Single-base | Gold standard, comprehensive coverage | DNA degradation, complex data analysis | Discovery phase, biomarker identification [9] [23] |
| Restriction Enzyme-Based | Methylation-Sensitive Restriction Enzymes (HpaII, MspI), HELP Assay, MRE-Seq | Site-specific (depends on enzyme) | No bisulfite conversion, preserves DNA integrity | Limited to enzyme recognition sites | Targeted validation, clinical assays [25] [23] |
| Affinity Enrichment-Based | Methylated DNA Immunoprecipitation (MeDIP), MBD-seq | Regional | No conversion, works with degraded DNA | Lower resolution, antibody variability | Genome-wide methylation patterns [23] |
| Microarray-Based | Illumina Infinium MethylationEPIC | Single-base (but predefined sites) | High-throughput, cost-effective for large studies | Limited to predefined CpG sites | Large cohort studies, epidemiological research [20] [23] |
| Third-Generation Sequencing | Nanopore sequencing, SMRT sequencing | Single-base | Direct detection, long reads | Higher error rates, specialized equipment | Emerging technology, comprehensive analysis [9] |
Experimental Workflow for Methylation Biomarker Validation
The following diagram illustrates a generalized workflow for developing and validating methylation biomarkers in liquid biopsies, synthesizing approaches from multiple studies:
Figure 1: Methylation Biomarker Development Workflow
The Scientist's Toolkit: Essential Research Reagents
Successful methylation biomarker research requires specialized reagents and tools. The following table details essential components of the methylation researcher's toolkit:
Table 4: Essential Research Reagents for Methylation Analysis
| Reagent Category | Specific Examples | Function | Key Considerations |
|---|---|---|---|
| Methylation-Sensitive Enzymes | HpaII, MspI (isoschizomer pair) [25] | Differential digestion based on methylation status | HpaII cleaves unmethylated CCGG sites; MspI cleaves regardless of methylation |
| Bisulfite Conversion Kits | Various commercial kits | Chemical conversion of unmethylated C to U | Conversion efficiency critical; newer enzymatic methods reduce DNA damage [24] |
| Methylated DNA Controls | Enzymatically methylated DNA (M.SssI) [25] | Positive controls for methylation assays | Ensures assay specificity and sensitivity |
| Targeted Panels | Ion AmpliSeq Methylation Panel for Cancer Research [26] | Multiplexed targeted methylation analysis | Cost-effective for focused studies; requires low DNA input |
| 5hmC Discrimination Tools | Glucosylation step + MspJI digestion [25] | Distinguishes 5hmC from 5mC | Emerging evidence for 5hmC as distinct biomarker [24] |
| Library Preparation Kits | Singlera method (semi-targeted PCR) [19] | Efficient library construction from limited DNA | Higher molecular recovery rate vs conventional methods |
Case Studies: Methylation Biomarkers in Action
PanSeer Multi-Cancer Early Detection Assay
The PanSeer assay represents a landmark advancement in methylation-based cancer detection. This test utilizes a targeted approach focusing on 595 genomic regions containing 11,787 CpG sites identified from public databases and internal sequencing data as consistently aberrant across multiple cancers [19]. The technical approach employs a semi-targeted PCR method that requires only a single ligation event, enabling high molecular recovery rates critical for detecting the scarce ctDNA in early-stage cancers.
In validation studies using plasma samples from the Taizhou Longitudinal Study, PanSeer demonstrated 88% sensitivity for detecting post-diagnosis patients with five common cancer types (stomach, esophageal, colorectal, lung, and liver) at 96% specificity [19]. Most impressively, the assay detected 95% of cancers in asymptomatic individuals who were later diagnosed within 1-4 years, providing compelling evidence for the early appearance of methylation changes in carcinogenesis.
MRE-Seq for Lung Cancer Detection
The MRE-Seq (Methylation-sensitive Restriction Enzyme digestion followed by Sequencing) protocol exemplifies the restriction enzyme-based approach to methylation analysis in liquid biopsies. This method achieved an AUC of 0.956 with 66.3% sensitivity for lung cancer detection at 99.2% specificity in a validation study [24]. The technique showed consistent performance across stages I-IV, with sensitivities ranging from 44.4% to 78.9%, demonstrating particular utility for early-stage detection where treatment options are most effective.
The following diagram illustrates the conceptual relationship between methylation biomarker properties and their clinical utility:
Figure 2: Methylation Properties Driving Clinical Applications
DNA methylation embodies the ideal characteristics of a cancer biomarker: early appearance during tumorigenesis, molecular stability that withstands analytical processing, and convenient detectability in minimally invasive liquid biopsies. The convergence of these properties, coupled with advancing detection technologies, has positioned methylation biomarkers at the forefront of cancer diagnostics research.
Future directions in this field include the refinement of multi-cancer early detection tests, the development of tissue-of-origin determination algorithms based on methylation patterns, and the integration of methylation biomarkers with other molecular markers (mutations, fragmentomics) to enhance sensitivity and specificity. Additionally, the discrimination between 5-methylcytosine and 5-hydroxymethylcytosine shows promise as a more specific biomarker, particularly for tracking disease progression [24].
For researchers and drug development professionals, methylation biomarkers offer powerful tools not only for early detection but also for monitoring treatment response, detecting minimal residual disease, and understanding resistance mechanisms. As large-scale longitudinal studies continue to validate the clinical utility of these biomarkers, and as detection methods become more sensitive and cost-effective, methylation-based liquid biopsies are poised to transform cancer management across the clinical continuum.
Technology Landscape: Performance Profiles of Modern Methylation Detection Platforms
DNA methylation, the addition of a methyl group to the fifth carbon of a cytosine residue, is a fundamental epigenetic mechanism regulating gene expression, genomic imprinting, and cellular differentiation [27]. Bisulfite conversion-based sequencing methods represent the gold standard for detecting this modification at single-base resolution, a critical capability for understanding its functional consequences [28] [29]. The fundamental principle involves treating DNA with sodium bisulfite, which converts unmethylated cytosines to uracil (read as thymine after PCR amplification), while methylated cytosines remain unchanged [28] [30]. This process creates sequence polymorphisms that allow precise quantification of methylation status at individual cytosine sites through subsequent sequencing [31].
The two primary bisulfite sequencing approaches discussed in this guide—Whole Genome Bisulfite Sequencing (WGBS) and Reduced Representation Bisulfite Sequencing (RRBS)—offer this single-base resolution but differ substantially in genomic coverage, application focus, and cost structure [32] [33]. While WGBS provides a comprehensive methylome map, RRBS employs a strategic enrichment strategy to target functionally relevant regions at reduced cost [34] [35]. Understanding their technical performance characteristics is essential for researchers investigating epigenetic mechanisms in development, disease, and therapeutic intervention.
Experimental Methodologies and Workflows
Whole Genome Bisulfite Sequencing (WGBS) Protocol
The standard WGBS protocol involves fragmenting genomic DNA via sonication or enzymatic digestion, followed by library preparation with bisulfite-converted adapters [30]. Critical steps include:
- DNA Fragmentation: 50-500 ng of high-quality genomic DNA is fragmented to 200-300 bp using Covaris shearing or nebulization.
- Bisulfite Conversion: Fragmented DNA undergoes bisulfite treatment using commercial kits (e.g., Zymo Research EZ DNA Methylation-Gold or Qiagen EpiTect), typically involving 3-16 hour incubations at temperatures ranging from 50°C to 65°C [30]. This conversion step introduces substantial DNA degradation (up to 90% DNA loss) through depyrimidination, necessitating careful optimization [30] [36].
- Library Amplification: Converted DNA is PCR-amplified (10-18 cycles) using bisulfite-converted polymerase systems (e.g., Pfu Turbo Cx or KAPA HiFi Uracil+) [30].
- Sequencing: Libraries are sequenced on Illumina platforms, with recommended coverage of 20-30x for mammalian genomes, requiring approximately 800 million to 1 billion 100bp reads [31].
Protocol variations include pre-bisulfite adapter tagging (which requires higher DNA input) versus post-bisulfite adapter tagging (PBAT) methods that reduce DNA loss but may introduce different biases [30].
Reduced Representation Bisulfite Sequencing (RRBS) Protocol
The RRBS methodology utilizes restriction enzyme digestion to selectively target CpG-rich regions:
- Enzymatic Digestion: Genomic DNA (10-100 ng) is digested with MspI (recognition site: CCGG), a methylation-insensitive restriction enzyme that cuts frequently in CpG-rich regions [34] [35].
- Size Selection: Digested fragments undergo strict size selection (40-220 bp) to enrich for CpG islands and promoter regions [32] [35].
- Bisulfite Conversion: Size-selected fragments undergo standard bisulfite conversion as described for WGBS.
- Library Preparation and Sequencing: Libraries are prepared with standard bisulfite-converted adapters and sequenced on Illumina platforms, typically requiring 10-50 million reads per sample depending on the organism [31].
Recent protocol enhancements recommend paired-end sequencing for RRBS to better distinguish single nucleotide polymorphisms (SNPs) from true methylation events, counter to conventional practice [34].
The graphical workflow below illustrates the key procedural differences between WGBS and RRBS:
Technical Performance Comparison
Genomic Coverage and Regional Specificity
The fundamental distinction between WGBS and RRBS lies in their genomic coverage strategies and the resulting methylation profiles:
Table 1: Genomic Coverage and Regional Specificity Comparison
| Parameter | WGBS | RRBS |
|---|---|---|
| Genomic Coverage | 80-95% of all CpG sites [29] [33] | 1.6-12% of all CpG sites (species-dependent) [33] |
| CpG Island Coverage | >95% [32] | 85-90% [31] |
| CpG Shore Coverage | Comprehensive [32] | Limited [32] |
| Open Sea Regions | 88% of sequencing reads [35] | Minimal coverage [35] |
| Repetitive Elements | 45% of interrogated CpGs in repeats [33] | Proportional to genome-wide coverage [33] |
| Methylation Context | CpG, CHG, and CHH contexts [31] | Primarily CpG context [34] |
WGBS provides truly genome-wide coverage, capturing methylation patterns across all genomic contexts including intergenic regions, repetitive elements, and low-CpG-density "open sea" regions [32] [33]. In contrast, RRBS strategically targets CpG-rich regions, with approximately 34% of reads originating from CpG islands, 12% from shores, and 13% from shelves, representing a 12.8-fold enrichment over WGBS in CpG islands [35]. This targeted approach comes at the cost of comprehensive coverage but provides enhanced depth in functionally significant regulatory regions.
Detection Sensitivity, Specificity, and Quantitative Performance
Both techniques offer single-base resolution, but their detection characteristics differ significantly:
Table 2: Sensitivity, Specificity, and Quantitative Performance
| Performance Metric | WGBS | RRBS |
|---|---|---|
| Single-Base Resolution | Yes [32] | Yes [32] |
| Detection of Intermediate Methylation | Comprehensive capture [34] | Greatly reduced prevalence [34] |
| Mapping Efficiency | 45% lower than BWA meth in comparative studies [34] | Varies by alignment tool [34] |
| False Positive Sources | Incomplete bisulfite conversion, particularly in GC-rich regions [29] [30] | SNP misidentification as methylation events [34] |
| Read Depth Requirements | 20-30x for mammalian genomes [31] | Lower due to targeted nature [31] |
| Methylation Quantification Accuracy | High at sufficient depth (>20x) [31] | High for covered regions [35] |
Notably, RRBS demonstrates a systematic reduction in detecting loci with intermediate methylation levels (those with proportions between fully methylated and unmethylated states), which may have important implications for functional interpretations of epigenetic heterogeneity [34]. WGBS more accurately captures this biological nuance but requires substantially greater sequencing resources.
Technical Reproducibility and Analytical Considerations
Technical variation in bisulfite sequencing arises from multiple sources, with conversion efficiency being a critical factor. Both methods typically achieve >99% conversion efficiency when optimized properly, as measured by spike-in controls [28] [30]. However, the extensive fragmentation from bisulfite treatment (up to 90% DNA degradation) introduces coverage biases, particularly in high-GC regions where base composition becomes unbalanced [30] [36].
Bioinformatic processing significantly influences data quality. Bismark, the most widely used methylation caller, demonstrates 82% concordance for CpG methylation levels compared to alternative pipelines [33]. Alignment tools substantially impact mapping efficiency, with BWA meth providing 45% higher mapping efficiency than Bismark in comparative studies [34]. Depth filtering parameters dramatically affect CpG site recovery, particularly for WGBS, with read depth thresholds between 5-20 reads per site commonly applied, though often without statistical justification [31].
Practical Implementation Considerations
Sample Requirements and Input Flexibility
Table 3: Sample Requirements and Practical Considerations
| Parameter | WGBS | RRBS |
|---|---|---|
| DNA Input Requirements | 0.5-5 μg (pre-BS); 100-200 cells (post-BS) [30] | 10-100 ng [35] |
| DNA Quality | High molecular weight preferred | More tolerant of partial degradation |
| Sample Multiplexing Capacity | Lower due to sequencing depth requirements | Higher due to reduced sequencing per sample |
| Optimal Sample Size | Smaller cohorts (due to cost constraints) [34] | Larger cohorts for population studies [34] |
| Suitability for FFPE Samples | Challenging due to DNA damage [28] | More suitable with protocol modifications [28] |
| Cell-Free DNA Applications | Limited due to cost and input requirements | Specialized adaptations (cfMethyl-Seq) perform well [35] |
WGBS demands substantially higher DNA inputs, particularly for pre-bisulfite adapter tagging protocols, while post-bisulfite approaches like PBAT enable sequencing of low-input samples (100-200 cells) [30]. RRBS is more adaptable to challenging sample types, including formalin-fixed paraffin-embedded (FFPE) tissues and cell-free DNA, with specialized modifications like cfMethyl-Seq developed specifically for liquid biopsy applications [28] [35].
Cost and Resource Analysis
The economic considerations of bisulfite sequencing methods directly impact experimental design:
- Sequencing Costs: WGBS requires 800 million to 1 billion reads for mammalian genomes, while RRBS typically requires 10-50 million reads—a 20-50 fold reduction in sequencing volume [31] [35].
- Library Preparation Costs: WGBS reagents are generally more expensive due to larger reaction volumes and specialized polymerases needed to handle bisulfite-converted templates [30].
- Computational Resources: WGBS demands substantial computational infrastructure for data storage and alignment, with file sizes typically 5-10 times larger than RRBS datasets [34].
- Cost Efficiency: RRBS provides the lowest cost per CpG covered in CpG islands, while WGBS becomes more cost-effective when considering genome-wide coverage [33].
For large-scale epidemiological or ecological studies requiring hundreds of samples, RRBS often represents the only feasible approach due to its substantially lower per-sample cost [34] [31].
Research Reagent Solutions
Table 4: Essential Research Reagents for Bisulfite Sequencing
| Reagent/Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Bisulfite Conversion Kits | Zymo Research EZ DNA Methylation-Gold; Qiagen EpiTect; Sigma-Aldrich Imprint DNA Modification Kit | Convert unmethylated cytosines to uracil; kit performance varies in conversion efficiency and DNA damage [30] |
| Methylation-Insensitive Restriction Enzymes | MspI (for RRBS) | Digests DNA at CCGG sites regardless of methylation status; enables targeted enrichment in RRBS [35] |
| Specialized Polymerases | Pfu Turbo Cx; KAPA HiFi Uracil+; JumpStart | Amplifies bisulfite-converted DNA with reduced bias; critical for maintaining library complexity [30] |
| Library Preparation Kits | NEBNext Ultra II; Swift Accel-NGS Methyl-Seq; TruSeq DNA Methylation | Prepares sequencing libraries from bisulfite-converted DNA; impacts final library complexity and bias [30] |
| Bioinformatic Tools | Bismark; BWA-meth; MethylDackel; BS-Seeker3 | Aligns bisulfite-converted reads and extracts methylation calls; mapping efficiency varies substantially [34] |
| Spike-In Controls | Lambda DNA; PCR products with known methylation status | Monitors bisulfite conversion efficiency; essential for quality control [28] |
Emerging Alternatives and Future Directions
While bisulfite-based methods currently represent the gold standard for DNA methylation analysis, enzymatic conversion approaches are emerging as promising alternatives. Enzymatic Methyl-seq (EM-seq) utilizes TET2 oxidation and APOBEC deamination to identify methylated cytosines without DNA damage [28] [29]. Comparative studies demonstrate EM-seq provides higher mapping efficiency, superior CpG detection (54 million versus 36 million CpGs at 1x coverage), and reduced GC bias compared to WGBS [29] [36]. Similarly, TET-assisted pyridine borane sequencing (TAPS) offers an alternative enzymatic approach but requires custom enzyme production [36].
Third-generation sequencing technologies, particularly Oxford Nanopore Technologies, enable direct methylation detection without conversion by measuring electrical current deviations as DNA passes through nanopores [29]. While currently exhibiting lower agreement with bisulfite methods (82% concordance), these approaches excel in characterizing challenging genomic regions and detecting methylation in long-range contexts [29].
For most applications requiring single-base resolution of DNA methylation, the choice between WGBS and RRBS involves balancing comprehensive coverage against practical constraints. WGBS remains optimal for discovery-oriented studies requiring complete methylome characterization, while RRBS provides a cost-effective alternative for focused investigations of CpG-rich regulatory regions, particularly in large-scale population studies [34] [31].
DNA methylation is a fundamental epigenetic mechanism involving the addition of a methyl group to cytosine bases, primarily at cytosine-phosphate-guanine (CpG) dinucleotides, which plays a crucial role in gene regulation, cellular differentiation, and disease pathogenesis [37] [27]. In the context of sensitivity-specificity analysis for methylation detection methods, researchers must navigate a complex landscape of technological platforms, each offering distinct trade-offs in throughput, cost, and genomic coverage. The Illumina Infinium MethylationEPIC BeadChip microarrays have emerged as a dominant platform for epigenome-wide association studies (EWAS), striking a balance between comprehensive coverage and practical implementation for large-scale studies [38] [39]. These arrays utilize a robust bisulfite conversion-based approach followed by hybridization to locus-specific probes, enabling quantitative methylation assessment at single-CpG-site resolution across thousands of samples [40]. As the field advances, understanding the performance characteristics, limitations, and appropriate application contexts for the different iterations of the EPIC platform—particularly in comparison with emerging sequencing-based methods—becomes essential for optimizing research outcomes and ensuring data quality in both basic research and clinical applications [37] [41].
Table 1: Key Specifications of Illumina MethylationEPIC Array Versions
| Parameter | EPIC v1.0 | EPIC v2.0 |
|---|---|---|
| Total Probes | >850,000 | ~930,000 |
| Coverage of RefSeq Genes | >99% | >99% with enhanced regulatory elements |
| Input DNA Requirement | 250 ng | 250 ng |
| Sample Throughput | 8 samples per array | 8 samples per array |
| Compatible Samples | Blood, FFPE tissue | Blood, FFPE tissue (with improved performance) |
| Genome Build | GRCh37/hg19 | GRCh38/hg38 |
| Regulatory Element Coverage | Standard enhancers | Expanded coverage of enhancers, CTCF-binding sites, open chromatin |
| Unique Features | Focus on CpG islands, promoters | ~200,000 new probes, probe replicates, removed poorly performing probes |
Platform Comparison: Technical Specifications and Performance Metrics
Evolution of EPIC Array Content and Design
The Illumina MethylationEPIC platform has undergone significant refinements from version 1.0 to version 2.0, with substantial implications for research applications. EPIC v2.0 retains approximately 77% of the probes from its predecessor while incorporating over 200,000 new probes specifically designed to expand coverage of regulatory elements, including enhancers, super-enhancers, CTCF-binding sites, and open chromatin regions identified through ATAC-Seq and ChIP-seq experiments in primary tumors [38] [40] [39]. This strategic enhancement addresses a critical gap in v1.0's coverage of functional genomic elements beyond traditional promoter regions. Furthermore, EPIC v2.0 has removed approximately 143,000 poorly performing probes from v1.0, approximately 73% of which were potentially influenced by underlying sequence polymorphisms, thereby improving overall data quality and reliability [39]. Another notable advancement in EPIC v2.0 is the implementation of probe replicates (approximately 5,100 probes with 2-10 replicates each), which enable internal quality assessment and technical validation [39] [42].
Comparative Performance Against Sequencing Methods
When evaluating methylation detection platforms, researchers must consider multiple performance dimensions where microarrays and sequencing technologies demonstrate complementary strengths and limitations. Whole-genome bisulfite sequencing (WGBS) provides the most comprehensive coverage with single-base resolution, capturing approximately 80% of all CpG sites across the genome, but requires substantial computational resources, higher costs, and involves DNA degradation due to harsh bisulfite treatment conditions [37] [29]. Enzymatic methyl-sequencing (EM-seq) has emerged as a promising alternative to WGBS, demonstrating high concordance while minimizing DNA damage through enzymatic conversion, but remains cost-prohibitive for large-scale studies [37] [29]. Oxford Nanopore Technologies (ONT) sequencing enables direct methylation detection without conversion and provides long-read capabilities for haplotype resolution, but shows lower agreement with established methods and requires high DNA input [37] [29].
Table 2: Comparative Analysis of DNA Methylation Detection Platforms
| Method | Resolution | Coverage | DNA Input | Relative Cost | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| EPIC Array | Single CpG site | ~930,000 predefined sites (v2.0) | 250 ng | $$ | High throughput, cost-effective, standardized analysis | Limited to predefined sites, cannot detect novel CpGs |
| WGBS | Single-base | ~80% of genomic CpGs | 1 µg | $$$$ | Comprehensive coverage, detects non-CpG methylation | High cost, DNA degradation, computational intensive |
| EM-seq | Single-base | Comparable to WGBS | Lower than WGBS | $$$$ | Minimal DNA damage, improved library complexity | Higher cost than arrays, bioinformatics complexity |
| ONT | Single-base | Genome-wide, but with coverage biases | ~1 µg (8 kb fragments) | $$$ | Long reads, direct detection, no conversion needed | Lower agreement with established methods, high error rate |
| Targeted BS | Single-base | Custom panels (dozens to hundreds of sites) | 50-100 ng | $ | Cost-effective for validation, high sensitivity for specific targets | Limited scope, panel design required |
Analytical Concordance and Reproducibility
Studies directly comparing methylation profiles across platforms demonstrate strong correlations between EPIC arrays and sequencing-based methods, particularly for well-powered studies. Research examining concordance between Infinium MethylationEPIC arrays and targeted bisulfite sequencing in ovarian cancer tissues and cervical swabs revealed strong sample-wise correlation, especially in tissue samples, though agreement was slightly reduced in cervical swabs likely due to lower DNA quality [43]. This supports the utility of targeted sequencing as a cost-effective validation approach for array-based discoveries. Comparative assessments of multiple genome-wide methylation methods indicate that while EM-seq shows the highest concordance with WGBS, EPIC arrays provide reliable data for the specific CpG sites they target, with each method capturing unique CpG sites and thus offering complementary insights [37]. Importantly, differences between EPIC v1.0 and v2.0, though generally modest, can introduce technical variation in meta-analyses and longitudinal studies, necessitating appropriate batch correction and normalization strategies [38] [39].
Experimental Protocols and Data Generation
Standardized Workflow for EPIC Array Processing
The Infinium MethylationEPIC assay follows a well-established workflow that begins with bisulfite conversion of genomic DNA using kits such as the Zymo Research EZ DNA Methylation Kit, which converts unmethylated cytosines to uracils while leaving methylated cytosines unchanged [29]. The converted DNA is then amplified, fragmented, and hybridized to the BeadChip containing locus-specific probes. After hybridization, the array undergoes single-base extension with fluorescently labeled nucleotides, followed by imaging on iScan or NextSeq 550 Systems [40]. The initial quality assessment typically includes evaluation of detection p-values to identify underperforming samples and probes, with common thresholds excluding samples with average detection p-value > 0.05 across all probes and individual probes with detection p-value > 0.01 in any sample [43] [29]. Data preprocessing generally involves normalization to address technical variation between probe types, with popular approaches including functional normalization [43] and beta-mixture quantile (BMIQ) normalization [42], followed by removal of probes containing common single nucleotide polymorphisms (SNPs) or demonstrating cross-reactivity [43].
Analytical Frameworks for Data Processing
Several specialized computational frameworks have been developed to address the unique characteristics of EPIC array data, particularly for the newer v2.0 platform. The MethylCallR package provides a comprehensive analysis pipeline specifically designed to handle EPICv2 features, including duplicated probes and integration with previous array versions through address-based conversion [42]. This package incorporates quality control metrics, outlier detection using Mahalanobis distance, and statistical power estimation to enhance data reliability. For clinical applications, particularly in tumor classification, established pipelines leverage reference databases and supervised machine learning algorithms to generate methylation-based classifications, though these require careful validation to ensure analytical and clinical validity [41]. The minfi and ChAMP packages remain widely used for initial data processing, normalization, and quality control, offering updated functionality for EPICv2 data [29] [42].
Critical Considerations for Platform Selection
Sensitivity, Specificity, and Coverage Trade-offs
The selection of an appropriate methylation profiling platform requires careful consideration of sensitivity, specificity, and coverage requirements specific to the research context. EPIC arrays provide excellent sensitivity for detecting methylation differences at moderate frequencies (typically >5-10% Δβ) across a predefined but biologically relevant subset of the methylome, making them ideal for hypothesis-generating EWAS in large cohorts [37] [43]. Sequencing-based approaches offer superior sensitivity for detecting rare methylation events or heterogeneous patterns and enable discovery of novel methylation sites outside predefined arrays, but at substantially higher cost per sample [37] [29]. In clinical validation studies, targeted bisulfite sequencing panels demonstrate strong concordance with EPIC array data for specific CpG sites, supporting their use as a cost-effective orthogonal validation method for array-based discoveries, particularly when analyzing many samples for a focused set of loci [43].
Technical and Biological Validation Frameworks
Robust technical validation is essential when implementing methylation profiling platforms, particularly for clinical applications. For EPIC arrays, key validation parameters include reproducibility across technical replicates, sensitivity to input DNA quality and quantity, and performance in specific sample types such as formalin-fixed paraffin-embedded (FFPE) tissues [40] [41]. The EPICv2 platform demonstrates improved performance with FFPE samples through modified protocols and optional restoration kits, expanding utility for retrospective studies utilizing archival tissues [40]. Biological validation should include confirmation of expected biological patterns, such as detection of known tissue-specific differentially methylated regions, X-chromosome inactivation patterns in female samples, and correlation with established demographic variables like age using epigenetic clocks [39] [42]. When comparing data across EPIC versions, analytical approaches such as ComBat normalization or version-specific modeling can mitigate technical variation introduced by platform differences [38] [39].
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Materials for EPIC Array Methylation Profiling
| Reagent/Material | Function | Example Products | Key Considerations |
|---|---|---|---|
| DNA Extraction Kits | Isolation of high-quality genomic DNA | Maxwell RSC Tissue DNA Kit, QIAamp DNA Mini Kit | Yield, purity (260/280 ratio), fragment size |
| Bisulfite Conversion Kits | Chemical conversion of unmethylated cytosines | EZ DNA Methylation Kit (Zymo Research), EpiTect Bisulfite Kit (QIAGEN) | Conversion efficiency, DNA degradation, input requirements |
| MethylationEPIC BeadChip | Multiplexed hybridization array | Infinium MethylationEPIC v2.0 BeadChip | Version selection (v1.0 vs v2.0), sample throughput |
| Array Processing Reagents | Amplification, fragmentation, labeling | Infinium HD Methylation Assay | Kit-sample matching, stability, lot-to-lot consistency |
| Quality Control Assays | Assessment of DNA quality pre- and post-conversion | Bioanalyzer High Sensitivity DNA Kit, Qubit fluorometer | DNA quantification, integrity measurement |
| Analysis Software/Packages | Data processing, normalization, statistical analysis | minfi, ChAMP, MethylCallR, GenomeStudio | Compatibility with EPIC version, normalization methods |
The Illumina MethylationEPIC platform represents a carefully balanced solution for DNA methylation profiling, offering an optimal compromise between throughput, cost, and coverage for many research applications. The evolution from EPIC v1.0 to v2.0 has addressed several limitations through expanded coverage of regulatory elements, removal of problematic probes, and improved annotation to current genome builds [38] [40] [39]. While emerging sequencing technologies like EM-seq and Nanopore sequencing offer distinct advantages in comprehensiveness and resolution, EPIC arrays maintain a strong position in large-scale epidemiological studies, clinical validation cohorts, and applications requiring standardized, cost-effective profiling of thousands of samples [37] [43]. Future directions in methylation profiling will likely see increased integration of multiple platforms, with EPIC arrays serving as discovery tools followed by targeted sequencing for validation and deep characterization, leveraging the complementary strengths of each approach to advance our understanding of epigenetics in health and disease.
Whole-genome DNA methylation analysis is crucial for understanding gene regulation in development and disease. For decades, whole-genome bisulfite sequencing (WGBS) has been the established gold standard, but its harsh chemical treatment causes significant DNA damage, leading to coverage gaps and biases. The development of Enzymatic Methyl-seq (EM-seq) provides a robust, bisulfite-free alternative that leverages enzymatic conversion to preserve DNA integrity, improve coverage uniformity, and enable superior performance with low-input samples. This guide objectively compares the performance of EM-seq against WGBS and emerging alternatives, providing researchers with data-driven insights for method selection.
DNA methylation, primarily as 5-methylcytosine (5mC), is a key epigenetic mark regulating gene expression, genomic imprinting, and cellular differentiation [44]. Aberrant methylation patterns are strongly associated with cancers, metabolic disorders, and autoimmune diseases [45]. Accurate, genome-wide mapping is therefore essential for both basic research and clinical diagnostics.
The fundamental challenge in methylation sequencing is discriminating between modified cytosines (5mC and 5hmC) and unmodified cytosines. Traditional bisulfite methods use harsh chemistry to deaminate unmodified cytosines to uracils, which sequence as thymines, while modified bases remain as cytosines. Enzymatic methods like EM-seq achieve this same goal through gentler, enzyme-driven processes [45] [46].
Technology Comparison: EM-seq vs. WGBS
The following table summarizes the core differences between the established WGBS method and the enzymatic EM-seq approach.
| Feature | Whole-Genome Bisulfite Sequencing (WGBS) | Enzymatic Methyl-seq (EM-seq) |
|---|---|---|
| Core Principle | Chemical conversion using sodium bisulfite to deaminate unmethylated C to U [45] [47] | Two-step enzymatic conversion using TET2 and APOBEC to protect modified C and deaminate unmodified C [45] [46] |
| DNA Integrity | Severe fragmentation and degradation due to extreme pH and temperature [45] [48] | Minimally damaging; preserves DNA integrity and results in longer insert sizes [45] [49] |
| Coverage Bias | High GC bias; under-represents GC-rich regions and skews towards AT-rich sequences [45] [44] | Uniform GC coverage and dinucleotide distribution across the genome [45] [49] |
| Input DNA | Typically requires microgram amounts (e.g., 100 ng - 1 µg) [47] [46] | Low input compatible; works with 10 ng down to 0.1 ng for specific kits [45] [49] |
| CpG Detection | Lower CpG coverage at same sequencing depth; more gaps in coverage [45] | More CpGs detected at greater depth with the same number of sequencing reads [45] [50] |
| 5mC/5hmC Discrimination | Cannot distinguish between 5mC and 5hmC [45] [46] | Cannot distinguish between 5mC and 5hmC in standard workflow [46] |
| Primary Limitations | DNA damage, high GC bias, requires high sequencing depth [45] [47] | Higher reagent cost, complex data analysis, potential for incomplete conversion in low-input samples [47] [48] |
Experimental Protocols and Workflows
Whole-Genome Bisulfite Sequencing (WGBS) Protocol
The conventional WGBS workflow involves several key stages that contribute to DNA damage [45] [47]:
- DNA Fragmentation: Genomic DNA is sheared to the desired size (e.g., 300 bp via Covaris sonication).
- Library Construction: Adapters are ligated to the fragmented DNA using a library prep kit (e.g., NEBNext Ultra II).
- Bisulfite Conversion: The library is treated with sodium bisulfite under high temperature and acidic conditions (e.g., using the Zymo Research EZ DNA Methylation-Gold kit). This step deaminates unmethylated cytosines to uracils.
- PCR Amplification: The converted DNA is amplified with a high-fidelity polymerase. The harsh bisulfite treatment necessitates more PCR cycles to recover sufficient library yield, increasing duplicate rates.
- Sequencing: Libraries are sequenced on platforms like Illumina NovaSeq. Alignment requires special bisulfite-aware tools like
bwa-methagainst a C/T and G/A converted reference genome.
Enzymatic Methyl-seq (EM-seq) Protocol
The EM-seq workflow, as implemented in the NEBNext kit, replaces harsh chemicals with enzymatic steps [45] [49] [46]:
- DNA Fragmentation and Library Prep: DNA is fragmented, and library construction begins with partial adapter ligation using NEBNext Ultra II reagents.
- Enzymatic Conversion: This critical two-step process protects methylation signals while converting unmodified cytosines.
- Step 1 - Oxidation: A cocktail containing the TET2 enzyme and an "Oxidation Enhancer" (containing T4-BGT) is used. TET2 oxidizes 5mC through 5hmC and 5fC to 5caC. The enhancer simultaneously glucosylates 5hmC to 5ghmC, protecting it.
- Step 2 - Deamination: The APOBEC enzyme deaminates unmodified cytosines to uracils. The oxidized 5mC (5caC) and glucosylated 5hmC (5ghmC) are protected and not deaminated.
- Library Completion & Amplification: The remaining adapter is ligated, and libraries are amplified with a specialized polymerase (e.g., Q5U). Fewer PCR cycles are needed due to higher DNA recovery.
- Sequencing & Analysis: Sequencing is performed on platforms like Illumina. The final sequence output is identical to WGBS, allowing the use of standard bisulfite sequencing bioinformatics pipelines.
Performance Data and Experimental Evidence
Direct comparative studies provide quantitative evidence of EM-seq's advantages over WGBS. The table below summarizes key performance metrics from controlled experiments.
| Performance Metric | WGBS | EM-seq | Experimental Context |
|---|---|---|---|
| Library Insert Size | Shorter fragments (~150-250 bp) [45] | Larger inserts; better preserves long fragments [45] [49] | Human NA12878 DNA sheared to 300 bp [49] |
| Library Yield & Complexity | Lower yield, requires more PCR cycles; higher duplication rates [45] | Higher yield with fewer PCR cycles; lower duplication rates [45] [50] | Various input amounts (10-200 ng) of human DNA [45] |
| GC Coverage Profile | Skewed; under-represents GC-rich regions [45] [44] | Flat, uniform distribution [45] [49] | Sequencing on Illumina NovaSeq, analysis with Picard [49] |
| CpG Sites Detected | Fewer CpGs at a given depth [45] | ~15-20% more CpGs at the same sequencing depth [45] | Human NA12878 data analysis [45] |
| Background Conversion Error | Low (~0.5%) but with overestimation bias [48] | Can be higher (>1%), especially with very low-input DNA [48] | Testing with unmethylated lambda DNA [48] |
| Input DNA Flexibility | High-input required; degraded with FFPE/cfDNA [47] | Effective with low-input, cfDNA, and FFPE samples [47] [50] | Studies on clinical cfDNA and chronic lymphocytic leukemia samples [50] |
The Scientist's Toolkit: Key Research Reagents
Successful implementation of EM-seq relies on specific enzymatic and library preparation components.
| Reagent / Kit | Function in Workflow |
|---|---|
| NEBNext Enzymatic Methyl-seq Kit | All-in-one solution for enzymatic conversion and Illumina library construction [49]. |
| TET2 Enzyme | Oxidizes 5mC to 5caC, protecting it from deamination by APOBEC [45] [46]. |
| APOBEC Enzyme | Deaminates unmodified cytosines to uracils, enabling their sequencing as thymines [45] [46]. |
| Oxidation Enhancer | Contains T4-BGT, which glucosylates 5hmC to 5ghmC, protecting it [45]. |
| NEBNext Ultra II Reagents | Used for highly efficient library construction with minimal bias [45] [49]. |
| Q5U DNA Polymerase | A modified high-fidelity polymerase optimized for amplifying uracil-containing templates [49]. |
Emerging Alternatives and Future Directions
While EM-seq is a leading bisulfite-free method, other technologies are evolving the field.
- Ultra-Mild Bisulfite Sequencing (UMBS): A recent innovation that re-engineers bisulfite chemistry to drastically reduce DNA damage while retaining the robustness and low cost of chemical conversion. Studies show it can outperform EM-seq in library yield and complexity with very low-input samples [51] [48].
- Oxford Nanopore Technologies (ONT): A third-generation sequencing platform that directly detects 5mC and 5hmC from native DNA without pre-conversion. Its key advantage is the ability to produce long reads, resolving methylation patterns in complex genomic regions and enabling haplotype-specific analysis [44].
- Multi-STEM MePCR: A novel, highly sensitive, bisulfite-free method for targeted methylation analysis. It integrates a methylation-dependent restriction endonuclease with a multiplex PCR using stem-loop primers, allowing for ultra-sensitive detection of methylation in multiple loci from minimal sample input [52].
The move towards bisulfite-free methods like EM-seq represents a significant advancement in epigenetic research. EM-seq unequivocally outperforms WGBS in preserving DNA integrity, providing uniform genomic coverage, and enabling more efficient CpG detection.
For researchers selecting a method, the choice depends on the project's specific needs:
- Choose EM-seq for whole-genome methylation studies where DNA integrity, coverage uniformity, and cost-effective sequencing (due to higher data utility) are priorities. It is particularly well-suited for precious, low-input, or highly fragmented samples like cfDNA and FFPE.
- Consider improved Bisulfite Methods (UMBS) if working within budget constraints or with very low-input samples where UMBS's high conversion efficiency is critical.
- Explore Long-Read Sequencing (ONT) for projects requiring methylation phasing, analysis of repetitive regions, or distinction between 5mC and 5hmC without additional chemical treatments.
The continued development of both enzymatic and refined chemical methods ensures that researchers have an increasingly powerful toolkit to unravel the complexities of the epigenome in health and disease.
Third-generation sequencing technologies from Oxford Nanopore Technologies (ONT) and Pacific Biosciences (PacBio) have revolutionized epigenomic research by enabling direct detection of DNA base modifications from native DNA, eliminating the need for destructive chemical conversions like bisulfite treatment. Long-read methylation profiling provides a unique advantage by delivering simultaneous information on genetic variation and epigenetic marks across multi-kilobase stretches of DNA, allowing for haplotype-phased epigenomic analysis in complex genomic regions. Whereas short-read bisulfite sequencing struggles with low mapping rates in repetitive regions and cannot resolve haplotype-specific methylation, long-read technologies natively preserve and detect methylation patterns across the entire genome, including previously inaccessible repetitive regions and structural variants. This capability is transforming research in cancer epigenetics, developmental biology, neurobiology, and functional genomics by providing a more complete picture of the epigenome.
Technology Comparison: Core Principles and Methodologies
Oxford Nanopore Technology: Electrical Signal Detection
The core principle of Oxford Nanopore sequencing involves passing native DNA strands through protein nanopores embedded in an electrically resistant polymer membrane. As DNA traverses the nanopore, the disruption of ionic current is measured, creating a unique electrical signal for each nucleotide combination within the pore. Critically, modified bases like 5-methylcytosine (5mC) and 5-hydroxymethylcytosine (5hmC) produce distinct current signatures from their unmodified counterparts, enabling direct detection of epigenetic modifications alongside primary sequence determination. This direct physical measurement requires no PCR amplification, preserving base modifications in their native state. The technology supports real-time data streaming, allowing researchers to monitor methylation patterns as sequencing occurs, and can be implemented across scalable platforms from portable MinION devices to high-throughput PromethION systems [53] [54].
PacBio HiFi Sequencing: Kinetic Signal Detection
PacBio's Single Molecule Real-Time (SMRT) sequencing technology detects methylation through polymerase kinetics rather than direct physical measurement. DNA polymerase molecules are immobilized at the bottom of zero-mode waveguides (ZMWs), where they incorporate fluorescently-labeled nucleotides into growing DNA strands. The key insight is that modified bases like 5mC and 6mA cause characteristic delays in the polymerase incorporation rate, creating distinctive "inter-pulse duration" (IPD) patterns in the sequencing data. These kinetic signatures are detected alongside the highly accurate primary sequence information generated by HiFi sequencing, which uses circular consensus sequencing (CCS) to repeatedly read the same DNA molecule, achieving >99.9% accuracy. This approach allows simultaneous detection of sequence variants and methylation patterns from the same data, with recent advancements enabling detection of 5hmC and hemimethylated 5mC through improved deep learning models [53] [55] [56].
Diagram Title: Core Sequencing Principles for Methylation Detection
Technical Specifications and Performance Metrics
Table 1: Comprehensive Technology Comparison for Methylation Detection
| Parameter | Oxford Nanopore Technologies | PacBio HiFi Sequencing |
|---|---|---|
| Detection Principle | Nanopore current sensing | Polymerase kinetics (IPD analysis) |
| DNA Modification Detection | 5mC, 5hmC, 6mA | 5mC, 6mA, 5hmC (planned) |
| Typical Read Length | 20 kb - >1 Mb (ultra-long reads) | 10-20 kb (HiFi reads) |
| Single-Molecule Accuracy | ~93.8% (R10 chip) [53] | >99.9% (HiFi mode) [53] |
| Methylation Calling Resolution | Single-molecule, single-base | Single-molecule, single-base |
| Typical Throughput | Up to 1.9 Tb/run (PromethION) [53] | 120 Gb/run (Revio) [53] |
| Direct RNA Methylation | Yes (direct RNA sequencing) | No (requires cDNA conversion) |
| Real-time Capability | Yes | No |
| Consensus Accuracy (CpG sites) | ~99.996% (50X coverage) [53] | >99.9% [53] |
| Equipment Cost | Lower (portable options) | Higher (benchtop systems) |
Experimental Design and Methodologies
Sample Preparation and Library Construction
Successful long-read methylation analysis begins with high-quality DNA extraction that preserves DNA integrity and native methylation states. For mammalian genomes, extraction methods that minimize mechanical shearing are essential to maximize read lengths. For ONT, the Ligation Sequencing Kit is most commonly used, requiring DNA end-repair, dA-tailing, and adapter ligation without PCR amplification. For PacBio HiFi sequencing, the SMRTbell library preparation involves creating closed circular templates with hairpin adapters that enable the circular consensus sequencing necessary for HiFi read generation. Both technologies have specialized protocols for low-input samples (down to 1ng for PacBio's AmpliFi protocol), with ONT typically requiring slightly less input DNA. For targeted methylation analysis, ONT offers adaptive sampling, a computational enrichment method that selectively sequences predefined genomic regions without physical isolation, while PacBio relies on whole-genome approaches with computational filtering [53] [55] [57].
Sequencing and Data Processing Workflows
Table 2: Bioinformatics Tools for Methylation Analysis
| Analysis Step | Oxford Nanopore Tools | PacBio HiFi Tools |
|---|---|---|
| Basecalling | Dorado (GPU-accelerated) | Integrated CCS (on-instrument) |
| Quality Control | NanoPack, LongQC | SMRTLink Quality Metrics |
| Read Alignment | Minimap2, Winnowmap2 | pbmm2, Minimap2 |
| Methylation Calling | Megalodon, Dorado modbase | IPD-based kinetic detection |
| DMR Analysis | Methylartist, Nanodisco | Pb-CpG-tool, Methylome Suite |
| Variant Integration | Clair3, Sniffles | DeepVariant, pbsv |
Diagram Title: Methylation Analysis Experimental Workflow
Key Research Reagents and Solutions
Table 3: Essential Research Reagents for Long-Read Methylation Studies
| Reagent/Solution | Function | Technology |
|---|---|---|
| Ligation Sequencing Kit | Library prep with native DNA | Oxford Nanopore |
| SMRTbell Prep Kit | Create circular templates for CCS | PacBio |
| DNA Extraction Kits (HMW) | Preserve long DNA fragments | Both technologies |
| Magnetic Beads (SPRI) | Size selection and cleanup | Both technologies |
| Buffer B1 (ONT) | Motor protein binding | Oxford Nanopore |
| Binding Kit (PacBio) | Polymerase binding to SMRTbells | PacBio |
| Sequencing Kit SQK | Flow cell priming and loading | Oxford Nanopore |
| Sequel II Binding Kit | Sample loading to SMRT Cells | PacBio |
Performance Analysis: Sensitivity and Specificity in Methylation Detection
Detection Accuracy and Coverage Uniformity
Recent comparative studies demonstrate that both technologies effectively detect methylation patterns, but with distinct performance characteristics. A comprehensive study comparing PacBio HiFi sequencing to whole-genome bisulfite sequencing (WGBS) revealed that HiFi sequencing identified approximately 5.6 million more CpG sites than WGBS, particularly in repetitive elements and regions of low WGBS coverage. The study found coverage patterns differed markedly: "PacBio HiFi shows a unimodal and symmetric pattern peaking at 28-30X, indicating relatively uniform coverage. In contrast, both WGBS datasets display right-skewed distributions, with the majority of CpGs covered at low depth (4-10X)" [55]. This uniform coverage translates to more comprehensive methylation profiling, with over 90% of CpGs in the PacBio HiFi dataset achieving ≥10X coverage compared to approximately 65% in WGBS datasets. For Oxford Nanopore, the introduction of the R10 flow cell with its dual-reader head design has significantly improved accuracy in homopolymeric regions, with initial read accuracy improved to 93.8% and consensus sequences reaching Q44 (99.996%) accuracy at 50X coverage [53].
Application-Specific Performance
In cancer research, both platforms have demonstrated strong performance for methylation-based classification. A recent study using Oxford Nanopore sequencing profiled full-length cell-free RNA from blood plasma and uncovered over 270,000 novel transcripts, enabling classification of early-stage oesophageal cancer and precancer with 100% sensitivity and specificity using machine learning models [58]. For PacBio, studies focusing on imprinting disorders have leveraged the technology's phasing capabilities to resolve parent-of-origin effects, with one study identifying 52,786 autosomal CpGs in 5,852 bins showing parent-of-origin effect of methylation, 60% of which had not previously been linked to imprinting [59]. In direct comparative applications, ONT typically excels in scenarios requiring rapid turnaround or detection of diverse modification types, while PacBio demonstrates advantages in applications demanding the highest consensus accuracy or complex haplotype resolution.
Advanced Applications and Case Studies
Epigenetic Mapping in Developmental and Rare Diseases
Long-read methylation profiling has proven particularly valuable for elucidating the epigenetic basis of developmental disorders and rare diseases. A landmark study from Children's Mercy Kansas City used PacBio HiFi sequencing to build the most comprehensive map of human genomic imprinting during development, analyzing 75 samples from 25 trios. The research demonstrated that "HiFi genome sequencing for single-molecular profiling of 5-mC, together with pedigree-based phasing in early developmental tissue, provides critical insight into previously uncharted loci in the human genome" [59]. The study identified two genes (BNC2, DNMT1) as novel candidate imprinting disorder loci, highlighting how long-read methylation analysis can uncover previously underappreciated genes and variants crucial for human development and disease. Similarly, Oxford Nanopore sequencing has been applied to differentiate monozygotic twins in forensic investigations by detecting reproducible DNA methylation differences, particularly in non-CpG contexts, achieving >99.5% alignment efficiency with an average N50 read length of 13 kb [60].
Cancer Epigenetics and Biomarker Discovery
In oncology, both technologies are driving advances in epigenetic biomarker discovery. Researchers using Oxford Nanopore sequencing analyzed cell-free DNA from cerebrospinal fluid of patients with non-small cell lung cancer (NSCLC) brain metastases, revealing distinct fragmentation, methylation, and hydroxymethylation patterns distinctive of disease [60]. The study marked "the first to identify distinct fragmentation profiles of mono-, di-, and tri-nucleosomes in cerebrospinal fluid-derived cfDNA from cancer samples," demonstrating the multi-layered epigenetic information accessible through nanopore sequencing. For PacBio, research in pediatric cancer has demonstrated the clinical utility of comprehensive methylation profiling, with one study reporting that long-read sequencing "offers a single, comprehensive genomic assay for diagnosing genetic disease" with a 10% higher diagnostic yield over all prior testing methods and significantly faster turnaround times [59].
Future Directions and Development Roadmap
Both Oxford Nanopore and PacBio are actively advancing their methylation detection capabilities. PacBio has announced plans to improve methylation detection in HiFi chemistry through licensing advanced DNA methylation detection methods from The Chinese University of Hong Kong. The new Holistic Kinetic Model 2 (HK2) framework integrates convolutional and transformer layers to model kinetic features with higher precision, enabling detection of 5hmC and strand-specific 5mC in standard sequencing runs [56]. This enhancement, delivered via software updates with no changes to sequencing protocols, will position PacBio to detect a broader range of biologically meaningful methylation signatures. Oxford Nanopore continues to enhance its basecalling algorithms and flow cell chemistry, with ongoing improvements to raw read accuracy and modification detection sensitivity. The technology's unique capability for direct RNA modification detection positions it uniquely for exploring the emerging field of epitranscriptomics, with researchers already using it to map RNA 2'-O-methylation (Nm) at single-base resolution, revealing its regulatory roles in cancer and neurodegeneration [61]. As both technologies mature, integration of methylation profiling into routine clinical sequencing appears increasingly feasible, potentially enabling more comprehensive molecular diagnostics that simultaneously assess genetic and epigenetic variation.
In the evolving landscape of molecular diagnostics, targeted assays for nucleic acid detection serve as critical tools for clinical validation across diverse applications including pathogen detection, cancer biomarker analysis, and methylation profiling. Quantitative PCR (qPCR) has long been the gold standard technique for molecular quantification in research and diagnostic laboratories worldwide. However, the emergence of digital PCR (dPCR) presents a powerful alternative that addresses several limitations inherent to qPCR methodology, particularly for high-sensitivity applications. This comprehensive guide objectively compares the technical performance, experimental requirements, and practical applications of these two pivotal technologies to inform researchers, scientists, and drug development professionals in their assay selection process.
The fundamental distinction between these technologies lies in their approach to quantification. While qPCR relies on relative quantification based on standard curves, dPCR provides absolute quantification through sample partitioning and Poisson statistical analysis [62] [63]. This methodological difference translates to significant implications for sensitivity, precision, and tolerance to inhibitors—factors particularly relevant for clinical validation studies requiring high reproducibility and detection of low-abundance targets.
Quantitative PCR (qPCR) Principles
qPCR, also known as real-time PCR, enables the detection and quantification of nucleic acid sequences through fluorescence monitoring during each amplification cycle. The technique employs a reaction mixture containing DNA polymerase, primers, nucleotides, and fluorescent reporters that generate signals proportional to the amount of amplified product [63]. Quantification occurs at the cycle threshold (Cq) where fluorescence exceeds background levels, with target concentration determined by comparison to standard curves of known concentrations [64]. This relative quantification approach provides a broad dynamic range but remains susceptible to variations in amplification efficiency and inhibitor presence [62] [63].
Digital PCR (dPCR) Principles
dPCR represents a fundamental evolution in nucleic acid quantification by enabling absolute counting of target molecules without standard curves. This technology partitions the PCR reaction mixture into thousands to millions of individual nanoreactions, typically using microfluidic chambers (nanoplates) or water-oil emulsion droplets [65] [62]. Following end-point amplification, each partition is analyzed for fluorescence to determine positive (containing target) versus negative (no target) reactions [65] [63]. The absolute target concentration is calculated using Poisson statistical modeling based on the ratio of positive to total partitions [65]. This partitioning approach enhances sensitivity, precision, and robustness against inhibitors [62].
Comparative Workflow Visualization
The diagram below illustrates the key procedural differences between qPCR and dPCR workflows:
Performance Comparison: Quantitative Data Analysis
Analytical Performance Metrics
Extensive comparative studies have quantified the performance differences between qPCR and dPCR across multiple parameters critical for clinical validation. The following table summarizes key analytical metrics derived from empirical studies:
Table 1: Performance Comparison Between qPCR and dPCR
| Performance Parameter | qPCR | dPCR | Experimental Context |
|---|---|---|---|
| Quantification Method | Relative (requires standard curve) [62] [63] | Absolute (no standard curve) [62] [63] | Fundamental measurement principle |
| Dynamic Range | Wider dynamic range [66] [67] | More limited dynamic range [66] [67] | Serial dilutions of target nucleic acids |
| Sensitivity | Lower sensitivity for low-abundance targets [65] [66] | Superior sensitivity, detects rare targets (<0.1%) [65] [62] [66] | Low viral load detection [66] [67]; Periodontal pathogens [65] |
| Precision (CV%) | Higher variability (CV%: 5.0) [68] | Superior precision (CV%: 2.3) [68] | Technical replicates of human genomic DNA [68] |
| Inhibitor Tolerance | Highly susceptible to inhibitors [62] [64] | Higher tolerance to PCR inhibitors [62] [63] | Samples with reverse transcription contaminants [64] |
| Precision for Low Targets | Higher variability at low concentrations [65] [64] | Lower intra-assay variability (median CV%: 4.5%) [65] | Periodontal pathogen detection [65] |
| Multiplexing Capability | Well-established | Improved due to endpoint detection [62] | Simultaneous detection of multiple targets |
Experimental Evidence from Clinical Applications
Recent studies directly comparing both technologies in clinically relevant contexts demonstrate consistent performance patterns. In periodontal pathogen detection, dPCR demonstrated significantly lower intra-assay variability (median CV%: 4.5%) compared to qPCR (p = 0.020) and superior sensitivity, particularly for low bacterial loads of P. gingivalis and A. actinomycetemcomitans [65]. The Bland-Altman plots from this study highlighted good agreement between technologies at medium/high bacterial loads but significant discrepancies at low concentrations (< 3 log10Geq/mL), resulting in qPCR false negatives and a 5-fold underestimation of A. actinomycetemcomitans prevalence in periodontitis patients [65].
In virology applications, a comparison of infectious bronchitis virus (IBV) detection demonstrated that while qPCR offered a wider quantification range, dPCR provided higher sensitivity and precision [66] [67]. Similarly, for gene expression analysis with low-abundant targets, ddPCR technology produced more precise, reproducible, and statistically significant results compared to qPCR, particularly for sample/target combinations with Cq ≥ 29 [64].
Experimental Protocols for Method Comparison
Side-by-Side Comparison Study Design
To objectively evaluate both technologies, researchers can implement a direct comparison protocol using identical sample material split between qPCR and dPCR platforms:
Sample Preparation:
- Nucleic acids are extracted using standardized kits (e.g., QIAamp DNA Mini Kit) [65]
- For clinical samples, include diverse matrices (tissue, plasma, saliva) to assess matrix effects
- Prepare serial dilutions (e.g., 1:2 to 1:100) to evaluate dynamic range and detection limits
Reaction Setup:
- qPCR Protocol: Prepare reactions with 20μL final volume containing 1× master mix, primers (0.4μM each), probe (0.2μM), and template DNA [65]. Run in triplicate with standard curves of known concentrations.
- dPCR Protocol: Use identical reaction mixture composition transferred to nanoplate or droplet generation system. For nanoplate dPCR (e.g., QIAcuity), partitioning creates ~26,000 partitions per well [65].
Thermocycling and Data Analysis:
- qPCR Conditions: Initial denaturation (95°C, 2 min); 45 cycles of denaturation (95°C, 15 sec) and annealing/extension (58°C, 1 min) with fluorescence acquisition [65]
- dPCR Conditions: Similar thermocycling profile but without real-time monitoring, followed by endpoint fluorescence reading of all partitions [65]
- Analysis: Compare quantification results, precision (CV%), and detected prevalence across dilution series
Key Research Reagent Solutions
Successful implementation of qPCR and dPCR assays requires specific reagent systems optimized for each technology:
Table 2: Essential Research Reagents for qPCR and dPCR
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| Nucleic Acid Extraction Kits | QIAamp DNA Mini Kit [65] | Standardized purification of high-quality DNA from clinical samples; critical for assay reproducibility |
| qPCR Master Mixes | TaqMan Gene Expression Master Mix [64] | Optimized enzyme blends with fluorescence compatibility for efficient real-time amplification |
| dPCR Master Mixes | QIAcuity Probe PCR Kit [65] | Formulated for optimal partitioning and endpoint detection in digital platforms |
| Hydrolysis Probes | Double-quenched probes targeting 16S rRNA [65] | Sequence-specific detection with reduced background fluorescence; essential for multiplexing |
| Partitioning Media | QIAcuity Nanoplate 26k [65] | Microfluidic chips generating thousands of nanoreactions for absolute quantification |
| Reference Materials | Human genomic DNA standards [68] | Quantified controls for assay validation and inter-experimental normalization |
Application to Methylation Detection in Clinical Validation
Relevance to Methylation-Specific Analysis
The performance characteristics of dPCR make it particularly suitable for DNA methylation analysis in clinical validation studies. DNA methylation biomarkers are increasingly recognized as valuable indicators for cancer diagnosis, with aberrant methylation patterns occurring in nearly all cancer types during precancerous or early stages [9]. The superior sensitivity and precision of dPCR enables detection of low-frequency methylation events in complex clinical samples, including liquid biopsies where circulating tumor DNA (ctDNA) represents a small fraction of total cell-free DNA [9].
For methylation analysis, both technologies can be adapted with bisulfite conversion pretreatment, which converts unmethylated cytosines to uracils while leaving methylated cytosines unchanged [9]. Following this conversion, targeted assays specifically detect methylation status at specific CpG sites. dPCR's absolute quantification capability provides advantages for determining the precise proportion of methylated alleles in heterogeneous samples, a critical parameter for cancer detection and monitoring.
Emerging Methylation Detection Technologies
Recent advancements in methylation detection include TET-assisted pyridine borane sequencing (TAPS), which offers single-base resolution without the DNA degradation associated with traditional bisulfite sequencing [69] [70]. Additionally, novel methods like single-cell Epi2-seq (scEpi2-seq) enable multi-omic detection of both DNA methylation and histone modifications at single-cell resolution [69]. While these advanced techniques provide comprehensive epigenetic profiling, targeted PCR-based approaches remain the workhorse for clinical validation of specific methylation biomarkers due to their simplicity, cost-effectiveness, and rapid turnaround time.
Selection Guidelines for Clinical Applications
Technology Decision Framework
Choosing between qPCR and dPCR requires careful consideration of analytical requirements and practical constraints:
Select qPCR when:
- The application requires a wide dynamic range [66] [67]
- Target abundance is moderate to high (Cq < 29) [64]
- The laboratory has established standard curves and reference materials
- Budget constraints prioritize cost-effectiveness for high-throughput screening
- Sample quality is consistent with minimal inhibitor concerns [62]
Select dPCR when:
- Detecting low-abundance targets (<0.1% mutant alleles or pathogens) [65] [62]
- Absolute quantification without standard curves is required [63]
- Maximum precision and reproducibility are critical [68]
- Analyzing challenging samples with potential PCR inhibitors [62] [64]
- Validating copy number variations or rare genetic events [62]
Future Perspectives and Integration Trends
The ongoing evolution of both technologies indicates increasing convergence rather than replacement. Future developments aim to enhance multiplexing capabilities, integrate artificial intelligence for data analysis, and transition toward practical point-of-care applications [63] [70]. For clinical validation pipelines, many laboratories implement both technologies strategically—using qPCR for initial screening and dPCR for confirmatory testing of borderline results or low-prevalence targets.
The nanoplate-based dPCR systems represent a significant advancement in workflow efficiency, substantially reducing processing time through simultaneous reading of all sample partitions, front-end automation, and qPCR-like plate setup [62]. This improved throughput makes dPCR increasingly suitable for screening and validation applications without compromising precision, accuracy, and sensitivity.
Liquid biopsy represents a transformative approach in oncology, enabling the minimally invasive detection and monitoring of cancer through the analysis of circulating tumor DNA (ctDNA) and other biomarkers in various bodily fluids [71] [72]. Unlike traditional tissue biopsies, which are invasive and cannot easily be repeated, liquid biopsies provide a dynamic view of the tumor's genetic landscape, allowing for early detection, treatment selection, and monitoring of treatment response and resistance [72]. The analysis of ctDNA—short fragments of tumor-derived DNA circulating in body fluids—has emerged as one of the most promising liquid biopsy applications due to significant advancements in DNA detection technologies [72].
Circulating tumor DNA originates from tumor cells that undergo apoptosis or necrosis and release their DNA fragments into the bloodstream and other biological fluids [73]. In cancer patients, ctDNA typically represents 0.1% to 1.0% of the total cell-free DNA (cfDNA) in circulation [73]. These fragments are relatively short, typically ranging from 20-50 base pairs, and have a short half-life of less than two hours, enabling real-time monitoring of tumor dynamics [73]. The detection of ctDNA requires highly sensitive technologies capable of identifying tumor-specific genetic and epigenetic alterations against a background of normal cfDNA [72].
Table 1: Biofluid Sources for ctDNA Liquid Biopsy
| Biofluid Source | Advantages | Primary Cancer Applications | Limitations |
|---|---|---|---|
| Blood (Plasma/Serum) | High analyte concentration, standardized protocols | Pan-cancer applications (NSCLC, CRC, breast cancer) | Invasive procedure, lower ctDNA fraction in early stages |
| Urine | Completely non-invasive, high patient compliance | Bladder, kidney, prostate cancer | Lower DNA concentration, variable fragment size |
| Cerebrospinal Fluid (CSF) | Direct contact with CNS tumors | Glioblastoma, CNS lymphomas, leptomeningeal disease | Highly invasive collection procedure |
| Saliva | Non-invasive, easy collection | Head and neck, oropharyngeal cancers | Contamination from oral bacteria, lower specificity |
| Pleural Fluid | Local tumor DNA enrichment | Lung cancer, mesotheliomas, metastatic disease | Invasive collection, primarily for symptomatic effusions |
ctDNA Analysis Across Different Biofluids
Blood-Based ctDNA Analysis
Blood remains the most extensively studied and utilized biofluid for ctDNA analysis, with plasma being preferred over serum due to reduced background DNA from leukocyte lysis during clotting [72]. The non-invasive nature of blood collection enables repeated sampling, facilitating dynamic monitoring of treatment response and emerging resistance mutations [71]. In clinical practice, blood-based ctDNA analysis has gained regulatory approval for identifying EGFR mutations in non-small cell lung cancer (NSCLC) when tissue testing is not feasible [72].
The sensitivity of blood-based ctDNA detection varies significantly with cancer stage and tumor burden. In early-stage cancers, the fraction of ctDNA can be exceptionally low (<0.1%), presenting substantial technical challenges [9]. Tumor DNA shedding characteristics also influence detectability, with certain cancer types (e.g., pancreatic, renal) demonstrating lower shedding rates than others (e.g., colorectal, melanoma) [72]. To overcome the challenge of low ctDNA concentration in blood, novel approaches are being explored, including the use of priming agents to transiently reduce endogenous cfDNA clearance, thereby increasing ctDNA detectability [72].
Urine-Based ctDNA Analysis
Urine represents a completely non-invasive biofluid for ctDNA detection, offering exceptional patient compliance and suitability for repeated sampling [9]. For cancers of the urinary system, including bladder and kidney cancer, urine contains direct tumor-derived DNA from exfoliated cancer cells, providing high sensitivity for detection [9] [73]. Specific methylation biomarkers such as CFTR, SALL3, and TWIST1 have demonstrated clinical utility for bladder cancer detection in urine samples [9].
Beyond urological malignancies, urine ctDNA analysis shows promise for systemic cancer detection. Tumor-derived DNA fragments enter urine through glomerular filtration, though the process significantly reduces analyte concentration compared to blood [72]. Technological advancements in urine collection, stabilization, and processing are addressing challenges related to variable urine composition, dilution effects, and DNA degradation, gradually enhancing the reliability of urinary ctDNA analysis [9].
Other Biofluids for ctDNA Analysis
Multiple other biofluids offer targeted approaches for ctDNA detection based on tumor location and accessibility. Cerebrospinal fluid (CSF) provides direct access to CNS-derived ctDNA, with demonstrated clinical utility for diagnosing and monitoring glioblastoma, CNS lymphomas, and leptomeningeal metastases [72]. CSF ctDNA analysis often reveals a higher mutant allele fraction than concurrent plasma samples, reflecting the blood-brain barrier's selective filtration.
Saliva and oral rinses show particular promise for detecting human papillomavirus (HPV)-associated oropharyngeal cancers, with tumor DNA detectable even in early-stage disease [72]. Pleural and peritoneal fluids offer alternative sources for ctDNA analysis in cancers causing malignant effusions, with potentially higher tumor DNA fractions than peripheral blood [72]. Cervical scrapings provide direct access to tumor DNA for cervical cancer detection, with methylation analysis demonstrating high sensitivity and specificity [74].
Methylation Detection Methods in ctDNA Analysis
DNA methylation represents one of the most promising analytical approaches for ctDNA detection, as cancer-specific methylation patterns occur frequently and early in carcinogenesis [9]. Methylation-based assays can detect abnormal hypermethylation of tumor suppressor gene promoters or global hypomethylation events characteristic of cancer cells [9] [73]. These epigenetic alterations offer a stable, chemically distinct mark that can be identified even at low ctDNA fractions.
Diagram 1: Methylation Analysis Workflow (Title: Methylation Analysis Workflow)
Bisulfite Conversion-Based Methods
Bisulfite conversion remains the gold standard technique for DNA methylation analysis. This method involves treating DNA with sodium bisulfite, which deaminates unmethylated cytosines to uracils while leaving methylated cytosines unchanged [74]. Following PCR amplification and sequencing, the original methylation status can be deduced by comparing the sequence to untreated DNA.
Whole Genome Bisulfite Sequencing (WGBS) provides comprehensive, single-base resolution methylation mapping across the entire genome [9]. This approach enables the discovery of novel methylation biomarkers without prior knowledge of specific regions of interest. However, WGBS requires substantial sequencing depth and bioinformatic resources, making it more suitable for discovery phases than routine clinical application [9].
Targeted Bisulfite Sequencing focuses on specific genomic regions with known differential methylation patterns in cancer, allowing for more cost-effective and sensitive detection when analyzing multiple samples [72]. This approach typically achieves higher sequencing depth in regions of interest, enhancing sensitivity for low-abundance ctDNA detection. Methods such as bisulfite padlock probes and similar capture-based techniques enable highly multiplexed analysis of hundreds of regions simultaneously [9].
Bisulfite-Free Methylation Detection
To overcome limitations of bisulfite conversion—which includes DNA degradation and incomplete conversion—alternative approaches have emerged. Enzyme-based methods utilizing methyl-binding proteins or antibodies, such as methylated DNA immunoprecipitation sequencing (MeDIP-Seq), selectively enrich for methylated DNA fragments without chemical modification [72]. These methods preserve DNA integrity but may provide lower resolution than bisulfite-based approaches.
Third-generation sequencing technologies, including Pacific Biosciences (PacBio) and Oxford Nanopore platforms, enable direct detection of methylated bases without pre-treatment [9]. These real-time sequencing methods identify methylation through altered electrical signals (Nanopore) or altered polymerase kinetics (PacBio), preserving native DNA configuration while providing long-read sequencing capabilities [9].
Methylation Haplotype Analysis
A significant innovation in methylation detection is the analysis of methylation haplotypes—patterns of co-methylation across multiple adjacent CpG sites on individual DNA molecules [74]. Traditional methods that calculate average methylation levels across DNA molecules can obscure the distinct patterns characteristic of cancer-derived DNA, particularly when ctDNA represents a small fraction of total DNA [74].
The Highly Methylated Haplotype (HMH) approach identifies DNA molecules with contiguous methylation across multiple CpG sites, a pattern highly specific for cancer-derived DNA [74]. In cervical cancer detection, this method demonstrated 89.9% sensitivity for invasive cancer at high specificity (94-98%), significantly outperforming conventional median methylation (78.0%) and single-CpG (71.6%) approaches [74]. This enhanced performance stems from the method's ability to distinguish the coordinated methylation patterns of tumor DNA from the stochastic methylation patterns of normal DNA.
Table 2: Comparison of Methylation Detection Methods
| Method | Resolution | Sensitivity | Advantages | Limitations |
|---|---|---|---|---|
| Whole Genome Bisulfite Sequencing | Single-base | High (with sufficient depth) | Comprehensive, discovery-based | Expensive, computationally intensive |
| Targeted Bisulfite Sequencing | Single-base | High for targeted regions | Cost-effective, focused on known markers | Limited to predefined regions |
| Methylation-Specific PCR | Locus-specific | Moderate to high | Rapid, low-cost, easily implemented | Limited multiplexing capability |
| Methylation Haplotype Analysis | Single-molecule | Very high | Distinguishes coordinated methylation patterns | Requires deep sequencing, complex analysis |
| Nanopore Sequencing | Single-base | Moderate | No bisulfite conversion, long reads | Higher error rate, specialized equipment |
Advanced Detection Technologies and Multimodal Approaches
PCR-Based Detection Methods
Digital PCR technologies, including digital droplet PCR (ddPCR) and BEAMing (beads, emulsion, amplification, magnetics), enable absolute quantification of mutant DNA molecules without the need for standard curves [72]. These methods partition individual DNA molecules into thousands of separate reactions, allowing for precise counting of mutant alleles based on endpoint fluorescence detection [71]. Digital PCR approaches offer exceptional sensitivity for detecting rare mutations, with limits of detection approaching 0.01% mutant allele frequency—sufficient for many ctDNA applications [72].
The primary limitation of PCR-based methods is their restriction to analyzing known mutations in predefined genomic regions [71]. While this targeted approach works well for monitoring established mutations (e.g., EGFR T790M in NSCLC, KRAS in colorectal cancer), it lacks the discovery capability needed for identifying novel alterations or comprehensive profiling of heterogeneous tumors [72].
Next-Generation Sequencing Approaches
Next-generation sequencing (NGS) platforms provide a comprehensive solution for ctDNA analysis, enabling simultaneous assessment of multiple genetic alterations across many genomic regions [9] [72]. NGS-based methods can be categorized into whole-genome, whole-exome, and targeted sequencing approaches, with the latter being most commonly applied to ctDNA analysis due to cost considerations and depth requirements [72].
Targeted NGS panels for ctDNA analysis focus on genes with known relevance in specific cancer types, typically achieving sequencing depths of 10,000x or higher to detect low-frequency mutations [72]. Advanced error-suppression techniques, including unique molecular identifiers (UMIs), duplex sequencing, and computational background correction, enhance detection sensitivity and specificity by distinguishing true mutations from sequencing artifacts [72].
Fragmentomics and Multimodal Integration
Fragmentomics represents an emerging approach that analyzes the physical characteristics of ctDNA, including fragment size distribution, end motifs, and genomic protection patterns [72]. Multiple studies have demonstrated that ctDNA fragments exhibit distinct size profiles compared to non-malignant cfDNA, with a tendency toward shorter fragments in cancer patients [72] [73]. The DELFI (DNA evaluation of fragments for early interception) method uses genome-wide fragmentation patterns and machine learning to detect cancer, achieving a sensitivity of 91% in one study [72].
Multimodal integration of genomic, epigenomic, and fragmentomic data represents the cutting edge of ctDNA analysis [72]. Research demonstrates that combining mutation detection with epigenetic signatures such as methylation patterns can increase detection sensitivity by 25-36% compared to genomic alterations alone [72]. Machine learning algorithms effectively integrate these diverse data types to improve cancer detection, classification, and monitoring capabilities.
Diagram 2: Multimodal Data Integration (Title: Multimodal Data Integration)
Research Reagent Solutions for ctDNA Analysis
Table 3: Essential Research Reagents for ctDNA Methylation Studies
| Reagent Category | Specific Examples | Function in ctDNA Analysis | Application Notes |
|---|---|---|---|
| Bisulfite Conversion Kits | EZ-96 DNA Methylation MagPrep kit (Zymo Research) | Converts unmethylated cytosines to uracils | Critical step for most methylation detection methods; quality affects downstream results [74] |
| DNA Extraction Kits | QIAamp Circulating Nucleic Acid Kit (Qiagen) | Isolves cell-free DNA from plasma, urine | Specialized kits optimize recovery of short cfDNA fragments [74] |
| Library Preparation | Accel-NGS Methyl-Seq DNA Library Kit (Swift Biosciences) | Prepares bisulfite-converted DNA for sequencing | Maintain complexity of converted libraries while preserving methylation information [9] |
| PCR Reagents | HotStart Taq polymerases, dNTPs | Amplifies target regions | Bisulfite-converted DNA requires optimized polymerases due to reduced sequence complexity [74] |
| Chromogenic Substrates | DAB (3,3'-Diaminobenzidine) | Visual detection in immunohistochemistry | Produces insoluble brown precipitate; used in validation studies [75] |
| Sequencing Kits | Illumina DNA Methylation kits, PacBio SMRTbell kits | Determines methylation status | Platform-specific reagents tailored to methylation analysis [9] [74] |
Liquid biopsy analysis of ctDNA from blood, urine, and other bodily fluids has established itself as a powerful approach for cancer detection, characterization, and monitoring. The choice of biofluid depends on cancer type, anatomical accessibility, and clinical context, with each source offering distinct advantages and limitations. Methylation-based detection methods provide particularly promising avenues for clinical application, with emerging technologies like haplotype analysis significantly enhancing detection sensitivity.
The field continues to evolve toward multimodal integration of genomic, epigenomic, and fragmentomic data, enabled by advanced computational approaches and machine learning. As standardization improves and clinical validation accumulates, ctDNA analysis is poised to transform cancer management across the diagnostic, prognostic, and therapeutic spectrum. Future developments will likely focus on enhancing sensitivity for early detection, reducing costs, and establishing clinical utility through prospective interventional trials.
Overcoming Challenges: Strategies for Enhancing Assay Performance and Reliability
DNA methylation analysis is a cornerstone of epigenetic research, with bisulfite conversion serving as the long-established gold standard method for distinguishing methylated from unmethylated cytosines. This chemical process exploits the differential reactivity of cytosine and 5-methylcytosine with bisulfite salts, thereby creating sequence-level differences that can be detected through subsequent PCR amplification and sequencing. Despite its widespread adoption, conventional bisulfite conversion presents two significant technical challenges that can compromise data integrity: substantial DNA degradation and incomplete conversion efficiency. These limitations become particularly problematic when working with precious or limited samples such as archival tissues, liquid biopsies, or single cells. This guide objectively compares the performance of various conversion approaches and provides researchers with practical strategies to mitigate these prevalent technical pitfalls, enabling more reliable methylation data across diverse experimental contexts.
Comparative Analysis of DNA Conversion Method Performance
The fundamental principle of bisulfite conversion relies on the differential chemical modification of cytosines based on their methylation status. Unmethylated cytosines undergo deamination to uracil through a sulfonation-deamination-desulfonation pathway, while methylated cytosines remain resistant to this conversion. However, this process occurs under harsh acidic conditions at elevated temperatures, creating the ideal environment for DNA backbone cleavage and depyrimidination. Simultaneously, DNA secondary structures, high GC-content regions, and incomplete denaturation can shield cytosines from bisulfite accessibility, leading to incomplete conversion and subsequent overestimation of methylation levels.
Recent technological advancements have introduced both improved bisulfite protocols and enzymatic alternatives that address these limitations with varying efficacy. The table below summarizes the comparative performance of different conversion methods based on recent independent validations:
Table 1: Performance Comparison of DNA Methylation Conversion Methods
| Method | DNA Input Range | Conversion Efficiency | DNA Recovery | Fragmentation Level | Protocol Duration |
|---|---|---|---|---|---|
| Traditional Bisulfite (Zymo EZ DNA) | 0.5-2000 ng [76] | ~99.9% [77] | 130% (overestimated) [76] | High (14.4 ± 1.2) [76] | 12-16 hours [76] |
| Enzymatic Conversion (NEBNext) | 10-200 ng [76] | Similar to bisulfite [76] | 40% (low) [76] | Low-Medium (3.3 ± 0.4) [76] | 4.5-6 hours [76] |
| Ultrafast Bisulfite (UBS-seq) | 1-100 cells [78] | High (reduced background) [78] | Higher than conventional BS [78] | Reduced damage [78] | ~10 minutes [78] |
Enzymatic conversion employs a three-step enzymatic process where TET2 oxidation and APOBEC deamination activities create the same base conversion outcome as bisulfite chemistry but through gentler biochemical means. This approach demonstrates significantly reduced DNA fragmentation, making it particularly advantageous for degraded samples such as FFPE tissues or cell-free DNA [76] [79]. However, current enzymatic methods suffer from substantially lower DNA recovery (approximately 40%) compared to bisulfite approaches, primarily due to the multiple bead-based cleanup steps required [76].
Experimental Data and Methodologies
Quantitative Performance Assessment Using qBiCo
Recent methodological advances have enabled systematic quantification of conversion performance parameters. The qBiCo (quantitative Bisulfite Conversion) assay, a multiplex TaqMan-based qPCR method, provides standardized assessment of three critical quality metrics: conversion efficiency, converted DNA recovery, and DNA fragmentation [76].
Table 2: qBiCo Performance Metrics for Conversion Methods at 10 ng Input
| Quality Parameter | Bisulfite Conversion | Enzymatic Conversion |
|---|---|---|
| Conversion Efficiency | Reproducible from 5 ng [76] | Reproducible from 10 ng [76] |
| Converted DNA Recovery | 130% (overestimation) [76] | 40% (low recovery) [76] |
| Fragmentation Index | 14.4 ± 1.2 (high) [76] | 3.3 ± 0.4 (low-medium) [76] |
Experimental Protocol: qBiCo Validation The qBiCo assay employs a 5-plex qPCR design targeting both single-copy genes and repetitive elements. For conversion efficiency calculation, two assays target the genomic and converted versions of the LINE-1 repetitive element. Converted DNA concentration is measured using an assay targeting the converted version of the single-copy hTERT gene. DNA fragmentation is assessed by comparing amplification of long versus short targets in the converted DNA. In developmental validation studies, this approach has demonstrated reproducible and sensitive assessment of converted DNA samples across various qPCR instruments [76].
Ultrafast Bisulfite Sequencing (UBS-seq)
The recently developed UBS-seq methodology addresses fundamental limitations of conventional bisulfite conversion by employing highly concentrated ammonium bisulfite/sulfite reagents at high reaction temperatures (98°C). This optimized chemistry accelerates the conversion reaction by approximately 13-fold, completing within 10 minutes instead of the conventional 2-3 hours [78].
Experimental Protocol: UBS-seq UBS-seq utilizes a bisulfite recipe (UBS-1) consisting of a 10:1 (v/v) mixture of 70% and 50% ammonium bisulfite. The reaction is performed at 98°C for approximately 10 minutes, dramatically reducing both DNA damage and background noise compared to conventional protocols. This method enables library construction from minute DNA inputs, including cell-free DNA or directly from 1-100 mouse embryonic stem cells, with improved accuracy in 5mC level estimation and higher genome coverage, particularly in high-GC regions and mitochondrial DNA [78].
Diagram 1: Bisulfite Conversion Pathways and Optimization Strategies. This diagram illustrates the competing chemical pathways in bisulfite conversion and how traditional versus ultrafast protocols influence outcomes toward either complete conversion or DNA degradation.
Impact on Downstream Applications
Effects on Methylation Detection Sensitivity
The technical limitations of bisulfite conversion directly impact the sensitivity and specificity of downstream methylation detection methods. Digital PCR platforms, including both nanoplate-based (QIAcuity) and droplet-based (QX-200) systems, have demonstrated strong correlation (r = 0.954) in methylation quantification despite their technological differences [80]. However, bisulfite-induced DNA fragmentation reduces the amplifiable template molecules, particularly affecting the detection of long amplicons or markers in already degraded samples.
In clinical applications such as liquid biopsy, where circulating tumor DNA is fragmented and scarce, reduced conversion efficiency can dramatically impact diagnostic sensitivity. Studies comparing mutation and methylation-based bladder cancer detection in urine samples found that both approaches suffered from false negatives in samples with low tumor content, with high concordance between mutation detection failure and methylation marker absence [81]. This suggests that sample quality and tumor fraction represent fundamental limitations that no conversion method can completely overcome.
Implications for Advanced Analysis Methods
Machine learning approaches for DNA methylation-based classification, particularly in oncology, are sensitive to data quality issues stemming from suboptimal conversion. For central nervous system tumor classification, neural network models demonstrated superior performance (99% accuracy) compared to random forest and k-nearest neighbor models, but all classifiers experienced reduced performance when tumor purity fell below 50% [82] [27]. Incomplete conversion contributes to this purity sensitivity by introducing technical noise that confounds biological signal detection.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Optimized DNA Methylation Analysis
| Reagent/Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Bisulfite Kits | Zymo EZ DNA Methylation-Gold [76], EpiTect Bisulfite Kit [80] | Chemical conversion of unmethylated cytosines; varying in speed, DNA recovery, and fragmentation |
| Enzymatic Conversion | NEBNext Enzymatic Methyl-seq [76] [79] | Gentle enzymatic conversion; superior for degraded samples despite lower DNA recovery |
| Specialized Polymerases | Q5U Hot Start High-Fidelity DNA Polymerase [79] | Amplification of uracil-containing templates after bisulfite conversion |
| Library Preparation | NEBNext Ultra II DNA Library Prep [79] | Optimized for bisulfite-converted DNA; handles low input and GC-rich sequences |
| Quality Control | qBiCo assay [76] | Multiplex qPCR for conversion efficiency, recovery, and fragmentation assessment |
| Rapid Conversion | BisulFlash DNA Modification Kit [77], UBS-seq reagents [78] | Faster protocols (20-45 minutes) reducing DNA damage while maintaining efficiency |
DNA degradation and incomplete conversion represent significant technical challenges in bisulfite-based methylation analysis, with direct consequences for data reliability and experimental outcomes. While traditional bisulfite methods continue to offer high conversion efficiency, newer approaches including enzymatic conversion and ultrafast bisulfite treatments provide compelling alternatives that minimize DNA damage. The optimal choice depends on specific experimental priorities: traditional bisulfite for maximal conversion efficiency, enzymatic methods for fragile samples, and ultrafast protocols for rapid processing with balanced performance. As methylation analysis continues to advance toward increasingly sensitive applications such as liquid biopsy and single-cell epigenomics, further optimization of conversion technologies will be essential for unlocking the full potential of DNA methylation as a biomarker across research and clinical domains.
The analysis of circulating tumor DNA (ctDNA) has emerged as a transformative, non-invasive tool in oncology, enabling capabilities from early cancer detection to monitoring of minimal residual disease (MRD). However, the reliable detection of ctDNA in early-stage cancers presents a formidable scientific challenge due to the extremely low abundance of tumor-derived DNA fragments circulating in blood. In early-stage disease, ctDNA can constitute less than 0.1% of total cell-free DNA (cfDNA), placing it near the detection limit of many conventional assays [83]. This low signal-to-noise ratio is compounded by factors such as variable tumor DNA shedding, short ctDNA half-life (estimated between 16 minutes and several hours), and the inherent background of cfDNA released from healthy hematopoietic cells [84] [85]. Overcoming these limitations requires sophisticated methodological approaches optimized for maximum sensitivity and specificity, particularly through the analysis of cancer-specific DNA methylation patterns, which offer distinct advantages over mutation-based detection for low-input samples [8] [9].
This guide objectively compares the performance of current technological platforms and assays for ctDNA analysis in early-stage cancers, with a focused examination of methylation-based methods. We present structured experimental data, detailed protocols, and analytical frameworks to inform assay selection for research and clinical development.
Technological Platforms and Performance Comparison
Assay Methodologies and Their Detection Limits
The core challenge in early-cancer ctDNA analysis is achieving a low enough Limit of Detection (LoD) to reliably identify the minimal tumor content. Different technologies offer varying balances of sensitivity, throughput, and genomic coverage.
Table 1: Comparison of Key ctDNA Analysis Technologies
| Technology | Primary Application | Reported LoD | Key Advantage | Key Limitation |
|---|---|---|---|---|
| Digital PCR (dPCR) | Targeted mutation detection | ~0.01% | High sensitivity for known variants; cost-effective [85] | Low throughput; limited to a few pre-defined mutations [83] |
| Tumor-Informed NGS (e.g., Signatera, NeXT Personal) | MRD detection & monitoring | 1 part per million (0.0001%) [86] | Ultra-high sensitivity; patient-specific [86] | Requires tumor sequencing; complex workflow; higher cost [87] |
| Tumor-Agnostic NGS Panels (e.g., Guardant Reveal) | Cancer detection & therapy selection | ~0.5% [83] | Broad panel; no tumor tissue needed [86] | Lower sensitivity for early-stage vs. tumor-informed [86] |
| Methylation-Based NGS (e.g., Multi-Cancer Early Detection tests) | Early cancer detection & tissue of origin | Varies; sensitivity for Stage I cancer can be as low as 30.5% in breast cancer [86] | Early emergence in tumorigenesis; stable marker; tissue-of-origin data [8] [9] | Complex bioinformatics; requires large reference databases [8] |
Quantitative Performance in Early-Stage Cancers
Clinical performance varies significantly across cancer types and stages. The following table summarizes real-world sensitivity data for different applications, highlighting the challenge of early-stage detection.
Table 2: Reported Sensitivity of ctDNA Assays in Early-Stage Solid Tumors
| Cancer Type | Assay / Study | Technology Type | Stage | Reported Sensitivity |
|---|---|---|---|---|
| Breast Cancer | Galleri (MCED test) [86] | Methylation-based, tumor-agnostic | Stage I | 2.6% |
| Breast Cancer | Galleri (MCED test) [86] | Methylation-based, tumor-agnostic | Stage IV | >90% |
| Breast Cancer | 15-methylation biomarker panel [9] | Methylation-based, targeted | Early Detection | AUC of 0.971 |
| Colorectal Cancer | ColonSecure [9] | Methylation-based, cfDNA | High-Risk Cohort | 86.4% |
| Colorectal Cancer | DYNAMIC-III [87] | Tumor-informed NGS (SaferSeqS) | Stage III (MRD) | 2-year RFS not improved with escalation |
| Multiple Cancers | Guardant360 CDx [83] | Tumor-agnostic NGS (mutations) | Varied | LoD of ~0.5% |
| Bladder Cancer | Urine TERT mutation [8] | Mutation-based (Urine source) | Varied | 87% (vs. 7% in plasma) |
Methylation-Based Detection: A Superior Paradigm for Low-Input Samples?
For early-stage cancers where ctDNA fraction is minimal, DNA methylation analysis presents several compelling advantages over somatic mutation-based detection.
Biological and Technical Advantages
- Early Abundance and Stability: DNA methylation alterations occur early in tumorigenesis and remain stable throughout tumor evolution. The methylome provides a rich source of cancer-specific signals, with thousands of differentially methylated CpG sites available for detection, increasing the chance of capturing a signal from even a few tumor fragments [8] [9].
- Enhanced Resistance to Degradation: Methylated DNA demonstrates relative enrichment in cfDNA due to nucleosome interactions that protect it from nuclease degradation. This inherent stability is crucial for sample collection, storage, and processing, especially compared to more labile molecules like RNA [8].
- Tissue of Origin Identification: Methylation patterns are highly tissue-specific, allowing not only for cancer detection but also for predicting the anatomical origin of the cancer, a critical feature for multi-cancer early detection tests [8].
Experimental Data and Validated Biomarkers
Research has identified numerous high-performance methylation biomarkers for early cancer detection. For instance, a study focusing on early breast cancer detection identified 15 optimal ctDNA methylation biomarkers that achieved an Area Under the Curve (AUC) of 0.971 in a validation cohort [9]. In colorectal cancer, the SEPT9 methylated assay, commercially available as Epi proColon, is one of the few FDA-approved liquid biopsy tests for screening [8]. The ColonSecure study, which evaluated a methylation-based cfDNA test in a high-risk population, demonstrated a sensitivity of 86.4% and a specificity of 90.7% for detecting colorectal cancer [9].
Table 3: Validated DNA Methylation Biomarkers for Early Cancer Detection
| Cancer Type | Methylation Biomarkers | Sample Type | Clinical Application |
|---|---|---|---|
| Lung Cancer | SHOX2, RASSF1A, PTGER4 [9] | Plasma, Tissue | Diagnostic |
| Colorectal Cancer | SDC2, SFRP2, SEPT9 [9] | Plasma, Stool | Screening, Early Detection |
| Breast Cancer | TRDJ3, PLXNA4, KLRD1, KLRK1 (via PBMCs) [9] | PBMCs, Plasma | Early Detection (93.2% sens, 90.4% spec) |
| Bladder Cancer | CFTR, SALL3, TWIST1 [9] | Urine | Diagnostic |
| Hepatocellular Carcinoma | SEPT9, BMPR1A, PLAC8 [9] | Plasma | Early Detection |
Experimental Protocols for High-Sensitivity ctDNA Analysis
Protocol: Tumor-Informed ctDNA Methylation Analysis for MRD Detection
This protocol is adapted from methodologies used in clinical studies like the DYNAMIC-III trial and assays such as Signatera [87] [86].
Tissue and Blood Collection:
- Collect primary tumor tissue (FFPE or fresh frozen) and matched peripheral blood (e.g., 2x10mL Streck tubes) from the patient.
- For longitudinal MRD monitoring, collect plasma pre-treatment, post-surgery, and during follow-up.
Sample Processing:
- Plasma Isolation: Centrifuge blood within 48 hours at 1600× g for 10 min, followed by a 16,000× g centrifugation for 10 min to isolate plasma.
- cfDNA Extraction: Extract cfDNA from 4-10 mL of plasma using a commercial kit (e.g., QIAamp Circulating Nucleic Acid Kit). Quantify using a fluorometer (e.g., Qubit dsDNA HS Assay).
- Tumor DNA Extraction: Extract genomic DNA from tumor tissue and matched white blood cells (for germline control).
Library Preparation & Sequencing:
- Whole Genome Sequencing (WGS) of Tumor: Sequence tumor and germline DNA to a coverage of ~80-100x to identify patient-specific somatic mutations (SNVs, indels).
- Custom Panel Design: Synthesize a patient-specific panel targeting 10-20 clonal mutations.
- Targeted Sequencing of Plasma cfDNA: Prepare NGS libraries from plasma cfDNA using adapter ligation with Unique Molecular Identifiers (UMIs). Enrich for the custom panel and sequence to ultra-high depth (>50,000x raw coverage).
Bioinformatic Analysis:
- Variant Calling: Use a pipeline (e.g., SaferSeqS) that leverages UMIs to generate error-corrected consensus sequences, filtering out PCR and sequencing artifacts [87].
- MRD Calling: A sample is declared ctDNA-positive if ≥2 patient-specific mutations are detected with statistical significance above background noise.
Protocol: Tumor-Agnostic Methylation Analysis for Cancer Detection
This protocol is based on the principles of multi-cancer early detection tests like Galleri and CancerSEEK [8] [86].
Blood Collection and cfDNA Extraction: As in Protocol 4.1.
Bisulfite Conversion and Library Preparation:
- Treat extracted cfDNA with sodium bisulfite, which converts unmethylated cytosines to uracils (read as thymines in sequencing), while methylated cytosines remain unchanged.
- Prepare sequencing libraries from the bisulfite-converted DNA. Enzymatic conversion methods (EM-seq) are emerging as alternatives that better preserve DNA integrity [8].
Methylome Sequencing:
- Use whole-genome bisulfite sequencing (WGBS) or a targeted approach focusing on a pre-defined panel of differentially methylated regions (DMRs) known to distinguish multiple cancer types from normal blood.
Bioinformatic Deconvolution and Classification:
- Map bisulfite-converted reads to a reference genome and calculate methylation scores for each CpG site in the panel.
- Input the methylation data into a machine learning classifier (e.g., a random forest or neural network) trained on large reference databases of cancer and normal methylation profiles.
- The classifier outputs two primary results: (1) a cancer signal (positive/negative), and (2) a predicted tissue of origin.
Visualization of Workflows and Signaling Pathways
ctDNA Methylation Analysis Workflow
Key Technical Hurdles in Low-Input ctDNA Analysis
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for ctDNA Methylation Analysis
| Reagent / Material | Function | Example Products / Methods |
|---|---|---|
| Cell-Free DNA Blood Collection Tubes | Stabilizes nucleated blood cells to prevent genomic DNA contamination and preserve cfDNA profile during transport. | Streck Cell-Free DNA BCT, Roche Cell-Free DNA Collection Tubes |
| cfDNA Extraction Kits | Isolate and purify short-fragment cfDNA from plasma with high efficiency and low contamination. | QIAamp Circulating Nucleic Acid Kit (Qiagen), MagMAX Cell-Free DNA Isolation Kit (Thermo Fisher) |
| Bisulfite Conversion Kits | Chemically converts unmethylated cytosine to uracil for subsequent methylation analysis. | EZ DNA Methylation-Gold Kit (Zymo Research), EpiTect Fast DNA Bisulfite Kit (Qiagen) |
| Enzymatic Methyl-Conversion Kits | Alternative to bisulfite; converts unmethylated cytosine without DNA degradation. | EM-Seq Kit (NEB) |
| Unique Molecular Identifiers (UMIs) | Short random barcodes ligated to DNA fragments pre-amplification to track original molecules and correct for PCR/sequencing errors. | Integrated into commercial library prep kits (e.g., Twist NGS Methylation System) |
| Targeted Methylation Panels | Pre-designed probes to enrich for cancer-specific methylated regions for deep sequencing. | Illumina TSCA Methylation Panel, Agilent SureSelect Methyl-Seq |
| Methylation-Aware NGS Aligners | Bioinformatics tools to accurately map bisulfite-converted reads to a reference genome. | Bismark, BS-Seeker2 |
| Methylation Classifiers | Machine learning models trained to distinguish cancer from normal and predict tissue of origin. | Random Forest, Support Vector Machines (SVMs), Convolutional Neural Networks (CNNs) [9] |
The optimization of ctDNA analysis for early-stage cancers remains a frontier in precision oncology. While significant technical hurdles persist, particularly concerning the low absolute quantity of ctDNA, emerging technologies are steadily improving sensitivity. Methylation-based analysis stands out for its ability to leverage abundant, stable, and tissue-informative epigenetic marks, making it a powerful tool for multi-cancer early detection and MRD monitoring. Tumor-informed NGS assays currently offer the highest sensitivity for MRD but are more complex and costly. The choice between technologies is therefore dictated by the specific research or clinical application. Future progress will hinge on standardizing protocols, improving bioinformatic error correction, and validating these assays in large-scale prospective trials to firmly establish their clinical utility and integration into routine cancer management.
The selection of an appropriate biomarker and sample matrix is a critical foundational step in the development of cancer diagnostics and therapeutic monitoring strategies. Within the realm of molecular diagnostics, DNA methylation has emerged as a particularly promising class of biomarkers due to its stability, cancer-specific patterns, and occurrence early in tumorigenesis [8] [9]. The clinical utility of these biomarkers, however, is profoundly influenced by the biological source from which they are isolated—whether from tumor tissue, blood plasma, or urine.
This guide provides an objective comparison of these three sample matrices, focusing on their performance characteristics within the context of DNA methylation biomarker research. We present synthesized experimental data and detailed methodologies to assist researchers, scientists, and drug development professionals in making evidence-based decisions for their specific application requirements, framed within the broader thesis of advancing sensitivity and specificity in methylation detection research.
Performance Comparison of Sample Matrices
The choice of sample matrix directly impacts the sensitivity, specificity, and overall clinical applicability of DNA methylation biomarkers. The table below summarizes the key performance characteristics and optimal use cases for tissue, plasma, and urine samples.
Table 1: Comparative Analysis of Sample Matrices for DNA Methylation Biomarker Detection
| Parameter | Tissue | Plasma | Urine |
|---|---|---|---|
| Invasiveness | High (surgical biopsy) | Minimally invasive (blood draw) | Non-invasive (voided urine) |
| Tumor DNA Yield | High (direct from source) | Low (0.01% - 10% of total cfDNA) [8] | Variable (high for urological cancers) [8] |
| Representativeness | Limited by tumor heterogeneity | Represents total tumor burden | Excellent for urological cancers; direct contact with tumors [88] [89] |
| Key Strengths | Gold standard; enables comprehensive profiling | Broad applicability across cancer types; good for monitoring | Superior for urological cancers; high patient compliance [8] [90] |
| Major Limitations | Invasive; cannot be repeated frequently | Low ctDNA fraction in early-stage disease; high background | Performance varies by cancer type [8] [9] |
| Exemplary Methylation Biomarkers | Pan-cancer panels (e.g., SHOX2, RASSF1A for lung) [9] | SEPT9 for colorectal cancer [9] | TWIST1, SALL3 for bladder cancer; GSTP1 for prostate cancer [10] [9] |
Analysis of Comparative Performance
Diagnostic Sensitivity and Specificity: The sensitivity of a methylation-based test is highly dependent on the concentration of tumor-derived DNA in the sample matrix. For urological cancers like bladder cancer, urine consistently demonstrates superior sensitivity because tumors shed cells and DNA directly into the urine. For instance, one study detected TERT mutations in 87% of urine samples compared to only 7% in matched plasma samples from bladder cancer patients [8]. For non-urological cancers, plasma is generally more sensitive than urine, though the absolute sensitivity is closely tied to tumor stage and location.
Applicability Across Cancer Types: Plasma-based liquid biopsies hold a significant advantage for cancers that do not have a direct connection to an excretable body fluid. They serve as a reservoir for tumor DNA shed from malignancies throughout the body, making them suitable for multi-cancer early detection tests [8]. Tissue remains the unrivaled source for initial tumor profiling and in-depth molecular characterization to guide therapy selection.
Experimental Protocols for Methylation Analysis
To ensure the reproducibility of methylation biomarker research, a clear understanding of core experimental workflows is essential. The following section outlines standardized protocols for analyzing DNA methylation across different sample types.
Urine Sample Collection and Processing Protocol
The pre-analytical handling of urine is crucial for obtaining high-quality DNA.
- Sample Collection: Collect approximately 50 mL of first-morning void urine from patients prior to cystoscopy or surgery [88]. This ensures a sufficient yield of cellular material and cell-free DNA.
- Preservation: Use a commercial urine preservation kit (e.g., Bladder CARE) if immediate processing is not possible. Stable urine samples can be preserved at room temperature for up to one month with such kits [88].
- Processing: Centrifuge the urine within 24-72 hours of collection to separate the sediment (pellet) from the supernatant.
- Storage: Resuspend the urine sediment in phosphate-buffered saline and store the DNA at -20°C or -80°C for long-term preservation [88].
- DNA Extraction: Isolve and purify DNA from the urine sediment or supernatant using commercial kits designed for low-concentration samples, such as the QIAamp DNA Blood Mini Kit (Qiagen) or the Quick-DNA Urine Kit (Zymo Research) [88].
DNA Processing and Bisulfite Conversion Workflow
After DNA extraction, the following steps are critical for most downstream methylation analyses.
- DNA Quantification and Standardization: Precisely quantify the extracted DNA using a fluorometric method and standardize the input amount for each sample to ensure uniform analysis.
- Bisulfite Conversion: Treat the DNA with sodium bisulfite using a commercial kit. This reaction deaminates unmethylated cytosines to uracils, while methylated cytosines remain unchanged [88].
- Purification: Purify the bisulfite-converted DNA to remove salts and reagents, resulting in template DNA ready for analysis.
- Methylation Detection: Analyze the converted DNA using a targeted method such as Methylation-Specific PCR (qMSP), digital PCR, or bisulfite sequencing [88] [10].
The following diagram illustrates the core workflow from sample collection to methylation detection.
Figure 1: Core Workflow for DNA Methylation Analysis.
Advanced Detection Technologies
Emerging technologies are enhancing the precision and efficiency of methylation detection.
- Digital PCR (dPCR): Partitions the sample into thousands of individual reactions, allowing for the absolute quantification of methylated DNA molecules with high sensitivity, ideal for low-abundance targets in liquid biopsies [88] [9].
- Next-Generation Sequencing (NGS): Methods like whole-genome bisulfite sequencing (WGBS) and reduced-representation bisulfite sequencing (RRBS) provide unbiased, genome-wide methylation profiling at single-base resolution, powerful for novel biomarker discovery [8] [9].
- CRISPR-Based Technologies: Newly developed detection systems that offer high specificity and the potential for rapid, point-of-care diagnostic applications [88].
- Third-Generation Sequencing: Technologies such as nanopore sequencing enable direct detection of methylation without the need for bisulfite conversion, thereby preserving DNA integrity [8].
The Scientist's Toolkit: Essential Research Reagents
Successful execution of methylation biomarker studies requires a suite of reliable reagents and platforms. The following table details key solutions and their functions.
Table 2: Key Research Reagent Solutions for DNA Methylation Analysis
| Reagent / Kit | Function | Application Context |
|---|---|---|
| QIAamp DNA Blood Mini Kit (Qiagen) | Extraction of high-quality DNA from various sample types, including blood and urine sediments. | Standardized DNA isolation for downstream bisulfite conversion and PCR analysis [88]. |
| Quick-DNA Urine Kit (Zymo Research) | Optimized for efficient DNA extraction from low-concentration urine samples. | Critical for obtaining sufficient template from urine-based liquid biopsies [88]. |
| EpiTect Bisulfite Kits (Qiagen) | Chemical conversion of unmethylated cytosine to uracil while preserving methylated cytosine. | Essential sample prep for most PCR and sequencing-based methylation detection methods [88]. |
| Methylation-Specific PCR (qMSP) | Quantitative PCR using primers that distinguish methylated from unmethylated sequences after bisulfite conversion. | Highly sensitive, targeted validation of specific methylation biomarkers [10] [89]. |
| SomaScan & Olink Platforms | High-throughput multiplex immunoassays for quantifying thousands of proteins in plasma or urine. | Proteomic-wide discovery for identifying novel protein biomarkers or validating findings from genomic studies [91]. |
Decision Framework and Concluding Remarks
Selecting the optimal biomarker and matrix is not a one-size-fits-all process but a strategic decision based on the clinical or research question. The following decision pathway provides a logical framework for this selection.
Figure 2: Decision Pathway for Sample Matrix Selection.
In conclusion, the quest for optimal sensitivity and specificity in methylation detection research is inextricably linked to the judicious selection of the biomarker and its source matrix. Tissue remains the gold standard for comprehensive tumor characterization. Plasma offers a broadly applicable, minimally invasive window for monitoring and detecting a wide array of cancers. Urine presents a non-invasive alternative with exceptional performance for cancers of the urinary tract. Future advancements will likely involve the refinement of multi-analyte panels and the integration of artificial intelligence to interpret complex data from these complementary sources, ultimately paving the way for more personalized and effective cancer management.
The analysis of circulating tumor DNA (ctDNA) present in liquid biopsies has revolutionized oncology by offering a non-invasive window into tumor genetics. However, a significant technical hurdle impedes its full potential: the characteristically low fraction of ctDNA within the total cell-free DNA (cfDNA) background. In patients with early-stage tumors or minimal residual disease (MRD), tumor-derived DNA can constitute a vanishingly small proportion, often less than 0.1% of the total circulating DNA, which is predominantly derived from healthy hematopoietic cells [92] [93]. This low signal-to-noise ratio creates a formidable challenge for detection technologies, which must discriminate true tumor-specific signals—be they genetic mutations or epigenetic alterations—from a massive background of wild-type DNA, as well as from technical artifacts introduced during sequencing [94]. The imperative to mitigate this background noise has driven the development of increasingly sophisticated pre-analytical and analytical techniques, pushing the limits of detection sensitivity and specificity to new frontiers.
Comparative Analysis of Leading Detection Methodologies
The evolution of ctDNA detection technologies has been marked by a continuous effort to enhance sensitivity and specificity while managing cost and throughput. The following table provides a structured comparison of the primary methods used to tackle the challenge of low ctDNA fraction.
Table 1: Comparison of ctDNA Detection Methodologies for Low-Fraction Scenarios
| Technology | Key Principle | Limit of Detection | Advantages | Limitations |
|---|---|---|---|---|
| Droplet Digital PCR (ddPCR) [92] [95] | Partitioning of samples into thousands of droplets for endpoint PCR; absolute quantification. | ~0.01% | High sensitivity for known mutations; absolute quantification without standards; rapid turnaround. | Low multiplexing capability; restricted to known, pre-defined mutations. |
| Targeted Next-Generation Sequencing (NGS) [92] [94] | Hybrid capture or amplicon-based enrichment of target regions; uses Unique Molecular Identifiers (UMIs). | ~0.01% - 0.1% | High multiplexing capability; ability to detect known and novel variants in targeted regions; UMI-enabled error correction. | PCR amplification biases; GC-content bias [96]; complex bioinformatics. |
| Methylation-Specific Sequencing [9] [74] | Bisulfite conversion or enzymatic treatment to discriminate methylated cytosines; sequencing of converted DNA. | Varies with method and marker | High cancer-specificity; early emergence in tumorigenesis; stable epigenetic signal. | Bisulfite conversion degrades DNA [96] [8]; complex data analysis; requires biomarker discovery. |
| Oxford Nanopore Technologies (ONT) [96] [97] | Real-time sequencing via changes in electrical current as DNA strands pass through protein nanopores. | Under evaluation; promising for structural variants and methylation | Long reads for phased haplotyping; direct detection of epigenetic modifications without bisulfite conversion; real-time analysis. | Currently higher raw error rate than NGS; bioinformatic complexity; ongoing validation for low-frequency variants. |
Emerging Approaches: Fragmentomics and Haplotyping
Beyond simply identifying mutations or methylation, novel approaches analyze the broader characteristics of ctDNA molecules. Fragmentomics leverages the fact that ctDNA fragments exhibit distinct size distributions and end-motif patterns compared to non-tumor cfDNA [96]. This "molecular footprint" can be used to enrich the tumor signal bioinformatically, boosting detection sensitivity without physical separation.
Another powerful emerging strategy is methylation haplotyping. Traditional methylation analysis often averages the methylation status across many DNA molecules, which can obscure the signal from rare ctDNA fragments. In contrast, haplotyping analyzes the co-methylation patterns across multiple CpG sites on a single DNA molecule. Cancer-derived DNA molecules tend to contain haplotypes where all or most CpGs in a region are fully methylated—a pattern rare in normal DNA. A 2025 study on cervical cancer demonstrated that a Highly Methylated Haplotype (HMH) score achieved 89.9% sensitivity for invasive cancer at high specificity, significantly outperforming median methylation (78.0%) and single-CpG (71.6%) methods [74]. This single-molecule resolution provides a powerful tool for distinguishing the true ctDNA signal from background noise.
Detailed Experimental Protocols for Noise Reduction
To ensure reproducible and sensitive ctDNA detection, standardized protocols from sample collection to data analysis are paramount. The following workflow outlines a comprehensive methodology for a targeted NGS approach with UMIs, which is a cornerstone of modern liquid biopsy analysis.
Pre-Analytical Phase: Minimizing Pre-Test Noise
Blood Collection & Plasma Separation [92]:
- Procedure: Collect blood using butterfly needles to avoid hemolysis. Draw a minimum of 2×10 mL of blood into specialized blood collection tubes (BCTs) containing cell-stabilizing preservatives (e.g., Streck cfDNA BCTs, PAXgene Blood ccfDNA tubes). These tubes prevent leukocyte lysis and the release of wild-type genomic DNA, stabilizing the sample for up to 7 days at room temperature.
- Centrifugation: Process tubes within 2-6 hours if using conventional EDTA tubes. Perform a two-step centrifugation: first at 380–3,000 g for 10 minutes at room temperature to isolate plasma, followed by a second, high-speed centrifugation at 12,000–20,000 g for 10 minutes at 4°C to remove residual cells and debris.
- Storage: Aliquot the purified plasma and store at -80°C to preserve cfDNA integrity. Avoid repeated freeze-thaw cycles.
cfDNA Extraction & Quantification [92]:
- Chemistry: Use silica membrane-based solid-phase extraction kits (e.g., QIAamp Circulating Nucleic Acid Kit) which have been shown to yield more ctDNA than magnetic bead-based methods.
- Quantification: Precisely quantify the extracted cfDNA using fluorometric methods (e.g., Qubit) to ensure sufficient input for downstream library preparation, which is critical for maintaining assay sensitivity.
Analytical Phase: Enhancing Signal During Processing
Library Preparation & UMI Ligation [94]:
- Construct sequencing libraries from the extracted cfDNA. A critical step is the ligation of Unique Molecular Identifiers (UMIs) to each original DNA molecule during the library preparation. These short, random DNA barcodes uniquely tag each original cfDNA fragment before any PCR amplification.
- This step allows for bioinformatic correction of PCR amplification biases and errors, as all copies derived from a single original molecule can be grouped into a "read family" for consensus sequencing.
Target Enrichment [94]:
- For targeted NGS, use hybrid-capture probes or amplicon-based panels to enrich for genomic regions of interest (e.g., known cancer driver genes). This focuses sequencing power on relevant loci, increasing the depth of coverage and the ability to detect low-frequency variants.
- Panels targeting several dozen to hundreds of genes are commonly used to balance comprehensiveness with cost and sensitivity.
High-Depth Sequencing:
- Sequence the enriched libraries on a high-throughput NGS platform. To robustly detect variants at frequencies as low as 0.1%, a mean sequencing depth of >10,000x is typically required, with even higher depths needed for ultra-sensitive MRD detection [94].
Post-Analytical Phase: Computational Noise Filtration
- Bioinformatic Analysis & Error Correction [94]:
- Demultiplexing & Alignment: Demultiplex sequenced reads and align them to the reference genome.
- UMI Consensus Calling: Group reads that share the same UMI into families. Generate a consensus sequence for each family, which effectively cancels out random PCR and sequencing errors that occurred in individual reads.
- Variant Calling: Call variants from the consensus reads. Only variants that are present in the consensus of multiple reads from the same original molecule are considered high-confidence, true positive calls. This process dramatically reduces false positives arising from technical artifacts.
The Scientist's Toolkit: Essential Research Reagents & Kits
Successful implementation of the protocols above relies on a suite of specialized reagents and kits. The following table details key solutions for constructing a robust liquid biopsy workflow.
Table 2: Research Reagent Solutions for ctDNA Analysis
| Product Category | Example Products | Key Function |
|---|---|---|
| Cell-Stabilizing Blood Collection Tubes | Streck cfDNA BCT, Qiagen PAXgene Blood ccfDNA Tube [92] | Prevents white blood cell lysis during transport/storage, preserving the wild-type DNA background and preventing dilution of the ctDNA signal. |
| cfDNA Extraction Kits | QIAamp Circulating Nucleic Acid Kit (Qiagen), Cobas ccfDNA Sample Preparation Kit [92] | Efficiently isolates short, fragmented cfDNA from large-volume plasma samples while removing PCR inhibitors. |
| Library Prep & UMI Kits | Kits from providers like IDT, Swift Biosciences, etc. | Prepares cfDNA for sequencing with high efficiency and incorporates UMIs for downstream error correction. |
| Target Enrichment Panels | Hybrid-capture or amplicon panels (e.g., Illumina, IDT, Agilent) | Enriches for a pre-defined set of cancer-related genes, allowing for deep, cost-effective sequencing of target regions. |
| Bisulfite Conversion Kits | EZ-96 DNA Methylation MagPrep kit (Zymo Research) [74] | Chemically converts unmethylated cytosines to uracils, allowing for subsequent PCR or sequencing-based discrimination of methylated alleles. |
The mitigation of background noise in liquid biopsies is a multi-faceted problem requiring an integrated approach from sample collection to computational biology. While current gold-standard methods like UMI-assisted targeted NGS provide robust sensitivity down to ~0.01% variant allele frequency, the field continues to advance. The future lies in multimodal approaches that combine the strengths of different technologies. For instance, the real-time, long-read capabilities of Oxford Nanopore sequencing allow for the simultaneous detection of genetic, epigenetic, and fragmentomic features in a single assay [96] [97]. This "all-in-one" approach can consolidate signals that are individually weak but collectively strong, thereby improving overall classification accuracy. Furthermore, machine learning models are increasingly being applied to integrate these complex multi-omics datasets to further distinguish the subtle signatures of cancer from the background, promising a new era of sensitivity and specificity in non-invasive cancer detection and monitoring [9].
The Role of AI and Machine Learning in Improving Sensitivity and Specificity from Complex Data
The integration of artificial intelligence (AI) and machine learning (ML) with molecular diagnostics is revolutionizing the analysis of complex biological data, particularly in the field of DNA methylation research. These computational approaches are dramatically enhancing the sensitivity and specificity of diagnostic and prognostic models for diseases ranging from cancer to neurological disorders. By identifying subtle, multidimensional patterns in large-scale epigenetic data that elude conventional statistical methods, ML models facilitate earlier disease detection, more precise classification, and improved patient stratification. This guide objectively compares the performance of various AI/ML methodologies applied to methylation data, detailing their experimental protocols, benchmarking their outcomes, and providing a toolkit for researchers embarking on similar analytical workflows.
DNA methylation is a stable epigenetic modification that regulates gene expression by adding a methyl group to cytosine bases, primarily at CpG dinucleotides, without changing the underlying DNA sequence [27] [98]. In healthy cells, these patterns are tightly regulated, but diseases like cancer are characterized by aberrant methylation—global hypomethylation and site-specific hypermethylation of promoter regions, often leading to the silencing of tumor suppressor genes [98]. Because these alterations are stable, tissue-specific, and occur early in disease pathogenesis, DNA methylation serves as an excellent biomarker [8] [98].
The analysis of methylation data presents significant challenges due to its high-dimensional nature; platforms like the Illumina Infinium MethylationEPIC array can simultaneously interrogate over 850,000 CpG sites [99]. Machine learning, a subset of AI, excels at identifying complex, nonlinear interactions within such large datasets. ML algorithms, from traditional models like random forests to advanced deep learning networks, can be trained to discern disease-specific methylation "signatures" from a background of normal variation and noise, thereby improving the sensitivity (ability to detect true positives) and specificity (ability to avoid false positives) of diagnostic tests [27] [98].
Performance Comparison of ML Methodologies
Different ML algorithms offer distinct advantages and trade-offs in processing methylation data. The tables below summarize the performance of various approaches across multiple studies and disease contexts.
Table 1: Comparative Performance of Machine Learning Models in Methylation-Based Studies
| Disease Context | Machine Learning Model(s) | Key Performance Metrics | Reference |
|---|---|---|---|
| Pediatric Acute Myeloid Leukemia (Relapse Prediction) | Boruta, LASSO, LightGBM, MCFS | Identified 111 vital methylation features strongly correlated with AML recurrence; models enabled high-accuracy classification of diagnosis vs. relapse. [99] | |
| Psychological Resilience Prediction | Random Forest, SVM, Logistic Regression, XGBoost | AUC of 0.77–0.82 for distinguishing low vs. high resilience using combined DNA methylation and neuroimaging biomarkers. [100] | |
| Multi-Cancer Early Detection (MCED) | Targeted Methylation Sequencing + Custom ML | High specificity and accurate tissue-of-origin prediction for over 50 cancer types (e.g., GRAIL's Galleri test). [98] | |
| Major Depressive Disorder (Placebo Response) | Multilayer Perceptron ANN, Gradient Boosting, LASSO | ANN achieved the highest accuracy for predicting individual non-specific treatment response, enhancing signal detection in clinical trials. [101] |
Table 2: Benchmarking Model Performance in a Public Health Context (NHANES Data) This study compared ML models with a traditional logistic model that incorporated complex survey design for predicting osteoarthritis [102].
| Model | Balanced Accuracy | Sensitivity | Specificity | Brier Score (Lower is Better) |
|---|---|---|---|---|
| Support Vector Machine (SVM) | 0.72-0.76 | 0.79-0.83 | Lower than Sensitivity | 0.1005-0.3245 |
| Deep Neural Network (DNN) | 0.72-0.76 | 0.79-0.83 | Lower than Sensitivity | 0.1005-0.3245 |
| Random Forest | 0.72-0.76 | Lower than Specificity | 0.86-0.96 | 0.1005-0.3245 |
| LASSO Regression | 0.72-0.76 | Lower than Sensitivity | Lower than Sensitivity | 0.1005-0.3245 |
| Logistic Model (with sampling weights) | Benchmark | Benchmark | Benchmark | Benchmark |
Key Insights from Comparative Data
- Ensemble and Tree-Based Models: Methods like Random Forest and Gradient Boosting Machines (e.g., LightGBM) are frequently top performers in classification tasks, such as predicting cancer recurrence, due to their ability to handle high-dimensional data and capture complex feature interactions [99] [103].
- Deep Learning for Complex Patterns: Deep neural networks (DNNs) and other deep learning architectures excel in scenarios with extremely complex, non-linear patterns, such as analyzing raw sequencing data from liquid biopsies for multi-cancer early detection [27] [98].
- Addressing Data Imbalance: In studies with imbalanced outcomes, the choice of model and resampling technique significantly impacts sensitivity and specificity. For example, in the NHANES analysis, Random Forest achieved high specificity, while SVM and DNNs achieved high sensitivity, demonstrating a trade-off that researchers must optimize based on clinical need [102].
Experimental Protocols and Workflows
A robust ML workflow for methylation analysis involves sequential steps from data acquisition to model deployment. The following diagram and description outline a generalized protocol.
Detailed Protocol for a Methylation-Based Study
The following protocol is synthesized from several studies, including a pediatric AML investigation that serves as a strong exemplar [99].
Step 1: Data Acquisition and Preprocessing
- Technology Selection: Choose an appropriate methylation profiling platform. The Illumina Infinium MethylationEPIC BeadChip is widely used for its cost-effectiveness and coverage of over 850,000 CpG sites [27] [99]. For discovery-phase research, whole-genome bisulfite sequencing (WGBS) provides single-base resolution.
- Quality Control (QC): Filter out probes with a high proportion of missing values (e.g., >15%) and perform imputation using algorithms like k-nearest neighbors (k-NN) to handle remaining missing values [99].
- Normalization and Batch Correction: Apply normalization methods (e.g., BMIQ, SWAN) to adjust for technical variation. Critically, address batch effects using methods like ComBat to harmonize data from different processing batches or platforms [27].
Step 2: Feature Selection
Given the extreme dimensionality of methylation data (hundreds of thousands of features), feature selection is essential to reduce noise and prevent overfitting.
- Initial Filtering: Use a wrapper method like Boruta to identify all relevant CpG probes by comparing feature importance to a shadow dataset [99] [100].
- Feature Ranking: Apply multiple algorithms with different principles to the filtered feature set to rank their importance. Common approaches include:
- Final Feature Subset Identification: Use Incremental Feature Selection (IFS) to determine the optimal number of top-ranked features that yield the best model performance [99].
Step 3: Model Training, Validation, and Interpretation
- Algorithm Selection and Training: Train multiple ML models (e.g., Random Forest, SVM, XGBoost, ANN) on the training set using the selected feature subset.
- Validation: Employ a rigorous k-fold cross-validation (e.g., 10-fold) within the training set to tune hyperparameters and avoid overfitting. Finally, evaluate the finalized model on a completely held-out test set that was not used during training or validation [101] [99].
- Interpretation: Use explainable AI (XAI) tools like SHapley Additive exPlanations (SHAP) to interpret model predictions, identify the most influential CpG sites, and provide biological plausibility to the model [103].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful execution of an AI-driven methylation study requires a suite of bioinformatic tools and computational resources.
Table 3: Key Research Reagent Solutions for AI-Methylation Analysis
| Tool/Resource | Function | Application Example |
|---|---|---|
| Illumina Infinium MethylationEPIC BeadChip | Genome-wide DNA methylation profiling at >850,000 CpG sites. | Primary data generation for EWAS in large cohorts. [27] [99] |
| R/Bioconductor (impute, minfi) | Open-source environment for statistical computing and preprocessing of methylation data. | Data normalization, quality control, and missing value imputation. [99] [104] |
| Boruta | Wrapper feature selection algorithm around Random Forest. | Identify all relevant CpG sites from the entire probe set. [99] [100] |
| Scikit-learn (Python) | Library providing efficient implementations of major ML algorithms. | Model training, validation, and hyperparameter tuning. [99] |
| SHAP (SHapley Additive exPlanations) | Game theory-based framework for explaining output of ML models. | Interpreting "black-box" models by quantifying feature contribution to predictions. [103] |
| Reference-Based Deconvolution (e.g., Houseman method) | Algorithm to estimate cell-type proportions in bulk tissue samples. | Account for cellular heterogeneity, a major confounder in methylation studies. [104] |
The synergy between AI/ML and DNA methylation analysis is setting a new standard for diagnostic and prognostic precision in biomedical research. As evidenced by the comparative data and protocols outlined, the choice of ML methodology directly impacts the sensitivity and specificity of models designed to extract meaningful signals from complex epigenetic data. While challenges remain—including the need for larger, diverse cohorts and improved model interpretability—the trajectory is clear. The continued refinement of these computational frameworks, coupled with standardized experimental workflows and robust toolkits, promises to accelerate the translation of epigenetic discoveries into clinically actionable insights, ultimately paving the way for more personalized and effective medical interventions.
Benchmarking and Translation: A Data-Driven Comparison for Clinical Deployment
DNA methylation, a fundamental epigenetic mechanism regulating gene expression and cellular differentiation, is pivotal in understanding biological processes and disease mechanisms such as cancer [44]. Accurate genome-wide profiling is essential for advancing epigenetic research, yet method selection presents a significant challenge due to the trade-offs between resolution, coverage, DNA integrity, and cost. This guide provides an objective, data-driven comparison of four prominent technologies: the established gold standard Whole-Genome Bisulfite Sequencing (WGBS), the targeted Illumina MethylationEPIC (EPIC) microarray, the emerging Enzymatic Methyl-seq (EM-seq), and the long-read Oxford Nanopore Technologies (ONT) sequencing [44] [105]. A recent systematic evaluation highlights that despite substantial overlap in CpG detection, each method uniquely captures specific genomic regions, underscoring their complementary nature [44]. This analysis, framed within sensitivity and specificity research, equips researchers and drug development professionals with the experimental data necessary to select the optimal method for their specific study design.
Technology at a Glance: Core Principles and Workflows
The four methods operate on distinct principles for detecting 5-methylcytosine (5mC), leading to significant differences in their workflows, data output, and analytical requirements.
Table 1: Core characteristics and requirements of the four DNA methylation profiling methods.
| Feature | WGBS | EM-seq | EPIC Array | ONT Sequencing |
|---|---|---|---|---|
| Core Principle | Chemical conversion (Bisulfite) | Enzymatic conversion | Hybridization to probes | Direct electronic sensing |
| DNA Input | ~100 ng - 1 µg [47] [106] | 10 ng - 200 ng [47] [107] | 500 ng [44] | ~1 µg [44] |
| Resolution | Single-base | Single-base | Single-base (but targeted) | Single-base |
| Genomic Coverage | ~80% of CpGs [44] | Near-complete [108] | ~935,000 pre-defined CpGs [44] | Genome-wide, including repetitive regions [109] |
| DNA Damage | High (fragmentation & degradation) [44] [107] | Low (preserves integrity) [47] [107] | Moderate (requires bisulfite conversion) [44] | None (sequences native DNA) [109] |
| Key Distinguishing Factor | Gold standard, but harsh chemistry | Milder conversion, superior for low-input/long reads | Cost-effective for large cohorts | Long reads, detects modifications simultaneously |
Visualizing Core Methodological Workflows
The following diagrams illustrate the fundamental workflows for the two whole-genome sequencing methods and the principle of direct detection.
Experimental Performance and Benchmarking Data
A 2025 systematic comparison assessed WGBS, EPIC, EM-seq, and ONT using three human genome samples (tissue, cell line, and whole blood), providing robust data on their performance [44] [105].
Performance Metrics and Practical Considerations
Table 2: Experimental performance data and practical metrics from comparative studies.
| Performance Metric | WGBS | EM-seq | EPIC Array | ONT Sequencing |
|---|---|---|---|---|
| CpG Detection (vs. WGBS) | Benchmark | Highest concordance [44] | Limited to ~935k sites [44] | Captures unique loci [44] |
| Coverage Uniformity | Biased, especially in GC-rich regions [107] | More uniform and consistent [44] | N/A (Targeted) | Effective in challenging regions [44] |
| Mapping Rate | Reduced due to fragmentation [110] | High (DNA integrity preserved) [47] | N/A | Standard alignment [110] |
| Agreement with WGBS | - | High [44] | High for covered sites [44] | Lower, but complementary [44] |
| Handling of 5hmC | Cannot distinguish from 5mC [44] | Can be protected and distinguished [44] [110] | Cannot distinguish from 5mC [44] | Can distinguish 5mC and 5hmC [111] |
| Multiplexing & Throughput | High (Illumina platform) | High (Illumina platform) | Very High | Fully scalable, real-time [109] |
Key Experimental Protocols in Benchmarking Studies
The following experimental details are critical for interpreting the comparative data and replicating such studies.
- Sample Preparation and DNA Sources: The 2025 benchmark study used three human genomic DNA samples derived from colorectal cancer tissue (fresh-frozen), a breast cancer cell line (MCF7), and whole blood from a healthy volunteer [44]. DNA was extracted using commercial kits, with purity and quantity assessed via NanoDrop and Qubit fluorometer [44].
- Library Construction and Sequencing:
- WGBS: DNA was fragmented and subjected to bisulfite conversion under conditions that promote C-to-U conversion but cause DNA degradation [44] [107].
- EM-seq: Libraries were prepared using kits (e.g., NEBNext Enzymatic Methyl-seq Kit). The protocol involves TET2 oxidation of 5mC/5hmC and APOBEC deamination of unmodified cytosines, avoiding DNA degradation [108] [107]. This allows for larger insert sizes (~370-550 bp) compared to WGBS [107].
- EPIC Array: 500 ng of DNA was bisulfite-converted and hybridized to the Infinium MethylationEPIC v1.0 BeadChip [44].
- ONT Sequencing: High molecular weight DNA is sequenced directly without conversion. The technology utilizes a motor protein to ratchet DNA through a biological nanopore, with modifications detected as characteristic current changes [109] [111].
- Data Processing and Analysis:
- Bisulfite/Enzymatic Data (WGBS/EM-seq): Reads are typically aligned using tools like Bismark, and methylation levels are calculated as beta values = methylatedcalls / (methylatedcalls + unmethylated_calls) [108].
- EPIC Array Data: Raw intensities from IDAT files are processed with packages like
minfiin R, followed by normalization to generate beta values [44]. - ONT Data: Basecalling, including modification detection, is performed using specialized algorithms that interpret the raw current signals ('squiggles') [111].
The Scientist's Toolkit: Essential Research Reagents
Successful execution of these methods relies on key commercial reagents and kits.
Table 3: Key research reagents and solutions for DNA methylation profiling.
| Reagent / Kit Name | Function | Associated Method(s) |
|---|---|---|
| NEBNext Enzymatic Methyl-seq Kit | Library prep with enzymatic conversion for 5mC/5hmC detection | EM-seq [108] [107] |
| EZ DNA Methylation Kit (Zymo Research) | Bisulfite conversion of genomic DNA | WGBS, EPIC Array [44] |
| Infinium MethylationEPIC BeadChip | Microarray for targeted methylation profiling of ~935k CpGs | EPIC Array [44] |
| MinION / PromethION Flow Cells | Disposable units containing nanopores for sequencing | ONT Sequencing [109] |
| AllPrep DNA/RNA FFPE Kit (Qiagen) | Co-extraction of DNA and RNA from challenging FFPE samples | All methods (Sample prep) [108] |
| Bismark | Alignment tool and methylation extractor for bisulfite/enzymatic data | WGBS, EM-seq [108] |
Application-Based Technology Selection
Choosing the right method depends heavily on the specific research question, sample type, and available resources.
- For Comprehensive Discovery and Novel Biomarker Identification: EM-seq is increasingly favored over WGBS for whole-genome analysis due to its superior coverage and preservation of DNA integrity, which is crucial for accurate biology [44] [107]. ONT is unparalleled for resolving methylation in repetitive regions, phasing haplotypes, and detecting multiple base modifications simultaneously [44] [111].
- For Large-Scale Epidemiological or Clinical Cohorts: The EPIC array remains the most cost-effective solution for profiling hundreds or thousands of samples where a predefined set of CpG sites is sufficient [44].
- For Low-Input and Fragmented Samples: EM-seq demonstrates clear advantages in low-input scenarios (down to 10 ng) and with fragmented DNA, such as from circulating tumor DNA (ctDNA) or formalin-fixed paraffin-embedded (FFPE) tissues, because it avoids the additional damage of bisulfite treatment [47] [108] [106].
- For Integrated Genetic and Epigenetic Analysis: ONT sequencing and newer six-letter sequencing methods (which build on enzymatic conversion principles) are the only technologies that can natively call genetic variants (SNPs) and epigenetic modifications in a single workflow, eliminating the need for separate experiments [110].
This guide underscores that no single DNA methylation profiling method is universally superior. The established WGBS benchmark is challenged by its inherent DNA damage. EM-seq emerges as a robust alternative for whole-genome studies, offering high data quality and compatibility with low-input samples. The EPIC array is optimal for targeted, high-throughput studies, while ONT sequencing provides unique long-read capabilities and direct detection of base modifications. The choice ultimately hinges on the specific trade-offs between genomic coverage, sample integrity, resolution, and budget, with the trend moving towards milder, multi-omics approaches that provide a more complete picture of the epigenetic landscape.
DNA methylation, the process of adding a methyl group to cytosine bases in CpG dinucleotides, is a fundamental epigenetic mechanism that regulates gene expression without altering the underlying DNA sequence [44] [9]. This modification plays crucial roles in genomic imprinting, X-chromosome inactivation, embryonic development, and cellular differentiation, with aberrant methylation patterns strongly implicated in various diseases, particularly cancer [44] [8]. The accurate assessment of DNA methylation patterns is thus essential for understanding biological processes and disease mechanisms, driving the development of numerous detection technologies.
This guide provides an objective comparison of current DNA methylation detection methods, focusing on four prominent platforms: whole-genome bisulfite sequencing (WGBS), Illumina MethylationEPIC BeadChip (EPIC), enzymatic methyl-sequencing (EM-seq), and Oxford Nanopore Technologies (ONT) sequencing. We systematically evaluate these technologies based on coverage, resolution, concordance, and cost-effectiveness, providing researchers with experimental data and protocols to inform their method selection for specific research applications.
Four major technologies dominate current DNA methylation profiling, each with distinct chemistries and detection principles. WGBS relies on bisulfite conversion to distinguish methylated from unmethylated cytosines, providing single-base resolution but causing substantial DNA degradation [44]. The EPIC microarray uses a similar bisulfite conversion principle but probes a predefined set of CpG sites across the genome, offering a cost-effective solution for large cohort studies [44] [112]. EM-seq represents an enzymatic alternative to bisulfite conversion, using TET2 and APOBEC enzymes to preserve DNA integrity while maintaining high accuracy [44] [113]. ONT sequencing directly detects methylated bases in native DNA through changes in electrical current as DNA passes through protein nanopores, enabling long-read sequencing and access to challenging genomic regions [44].
Table 1: Technical Specifications of Major DNA Methylation Detection Methods
| Technology | Chemical Principle | Read Type | DNA Input | Primary Applications |
|---|---|---|---|---|
| WGBS | Bisulfite conversion | Short-read | 50-100 ng [44] | Comprehensive methylome mapping, novel discovery |
| EPIC Array | Bisulfite conversion | Microarray | 500 ng [44] | Large cohort studies, clinical screening |
| EM-seq | Enzymatic conversion | Short-read | Lower than WGBS [44] | High-integrity methylation profiling, low-input samples |
| ONT Sequencing | Direct detection | Long-read | ~1 µg [44] | Structural variant analysis, challenging genomic regions |
Table 2: Performance Metrics Across DNA Methylation Detection Technologies
| Technology | Genomic Coverage | Resolution | Concordance with WGBS | Cost-Effectiveness |
|---|---|---|---|---|
| WGBS | ~80% of CpGs [44] | Single-base | Reference standard | Lower (high sequencing costs) |
| EPIC Array | ~935,000 predefined CpGs [44] | Single-site | High for covered sites [112] | Higher for large studies |
| EM-seq | Comparable to WGBS [44] | Single-base | Highest (R²=0.99) [44] [113] | Moderate (reduced library prep bias) |
| ONT Sequencing | Genome-wide | Single-base | Lower but captures unique loci [44] | Improving with new flow cells |
Experimental Data and Concordance Analysis
A systematic comparative evaluation assessed the performance of WGBS, EPIC, EM-seq, and ONT sequencing across three human genome samples derived from tissue, cell lines, and whole blood [44]. The study employed rigorous statistical analyses to determine concordance between methods, including Pearson correlation coefficients and absolute difference measurements in methylation β-values.
EM-seq demonstrated the highest concordance with WGBS, indicating strong reliability due to their similar sequencing chemistry [44]. In a separate validation study comparing an optimized Targeted Methylation Sequencing protocol (based on EM-seq) to WGBS, the agreement was exceptionally high (R² = 0.99) [113]. ONT sequencing showed lower overall agreement with both WGBS and EM-seq but uniquely captured certain genomic loci and enabled methylation detection in challenging regions like heterochromatic areas and repetitive elements [44].
For microarray technologies, a systematic comparison of 450K and EPIC arrays in 108 placental samples revealed high per-sample correlation (median Pearson correlation coefficient of 0.985), though individual CpG site correlations varied substantially [112]. The study identified 26,340 probes with absolute methylation differences >10% between platforms, highlighting the need for careful probe selection when combining datasets from different array versions [112].
Table 3: Concordance Metrics Between Methylation Detection Platforms
| Comparison | Sample Type | Correlation Metric | Result | Notes |
|---|---|---|---|---|
| EM-seq vs WGBS | Human tissue, cell line, blood | Genome-wide concordance | Highest agreement [44] | Similar coverage with less bias |
| EM-seq vs WGBS | Human and non-human primate | R² | 0.99 [113] | Optimized TMS protocol |
| ONT vs WGBS | Human tissue, cell line, blood | Genome-wide concordance | Lower agreement [44] | Captures unique loci |
| 450K vs EPIC | Placental samples | Per-sample correlation | Median r=0.985 [112] | 26,340 probes with >10% difference |
| TMS vs EPIC | Human samples | R² | 0.97 [113] | Targeted vs array approach |
Methodologies for Comparative Analysis
Sample Preparation and DNA Extraction
In the comparative evaluation of WGBS, EPIC, EM-seq, and ONT, researchers used three human sample types: colorectal cancer tissue (fresh frozen), MCF7 breast cancer cell line, and whole blood from a healthy volunteer [44]. DNA extraction employed the Nanobind Tissue Big DNA Kit (Circulomics) for tissue, the DNeasy Blood & Tissue Kit (Qiagen) for cell lines, and a salting-out method for whole blood [44]. DNA purity was assessed via NanoDrop (260/280 and 260/230 ratios), and quantification used an Invitrogen Qubit 3.0 fluorometer [44].
Platform-Specific Protocols
EPIC Array Processing: For the Illumina MethylationEPIC array, 500ng of DNA underwent bisulfite treatment using the EZ DNA Methylation Kit (Zymo Research) following manufacturer recommendations for Infinium assays [44]. Processed samples were hybridized to the BeadChip array using a 26μL hybridization volume. Data processing and normalization employed the minfi package (v1.48.0) in R, with β-values calculated using the beta-mixture quantile normalization method [44].
WGBS and EM-seq Library Preparation: Both WGBS and EM-seq libraries were prepared according to manufacturer specifications with appropriate quality control steps. The EM-seq protocol utilized the TET2 enzyme for oxidation of 5-methylcytosine to 5-carboxylcytosine and T4 β-glucosyltransferase to protect 5-hydroxymethylcytosine, followed by APOBEC deamination of unmodified cytosines [44]. This enzymatic approach preserves DNA integrity compared to the harsh bisulfite treatment in WGBS, which causes DNA fragmentation and can lead to incomplete conversion [44].
ONT Sequencing: For Oxford Nanopore sequencing, native DNA was prepared without bisulfite conversion. The method relies on direct electrical detection of modified bases as DNA passes through protein nanopores, with methylation status determined by deviations in electrical signals [44]. The protocol required approximately 1μg of 8kb fragments, reflecting the higher DNA input requirements for this technology [44].
Targeted Methylation Sequencing Optimization
The optimized Targeted Methylation Sequencing protocol incorporated several modifications to increase throughput and reduce costs: increased multiplexing, decreased DNA input, and use of enzymatic rather than mechanical fragmentation [113]. This protocol captures approximately 4 million CpG sites and has demonstrated strong agreement with both EPIC arrays (R² = 0.97) and WGBS (R² = 0.99) [113].
Diagram 1: Experimental workflow for comparative analysis of DNA methylation technologies
Research Reagent Solutions
Table 4: Essential Research Reagents for DNA Methylation Analysis
| Reagent/Kit | Function | Application |
|---|---|---|
| Zymo EZ DNA Methylation Kit | Bisulfite conversion of DNA | EPIC array, WGBS |
| Nanobind Tissue Big DNA Kit | High-molecular-weight DNA extraction | ONT sequencing |
| DNeasy Blood & Tissue Kit | Standard DNA extraction | Multiple platforms |
| TET2/APOBEC Enzyme Mix | Enzymatic conversion of cytosine modifications | EM-seq |
| Infinium MethylationEPIC v1.0 BeadChip | Microarray-based methylation profiling | EPIC array |
| Minfi R Package | Preprocessing and normalization of array data | Data analysis |
Cost-Effectiveness and Clinical Applications
The cost-effectiveness of DNA methylation technologies varies significantly based on project scope, with each method offering distinct advantages for specific applications. EPIC arrays provide the most cost-effective solution for large-scale epidemiological studies requiring rapid profiling of many samples at predefined sites [44] [112]. While WGBS offers comprehensive genome-wide coverage, its higher sequencing costs make it less suitable for population-scale studies [44]. EM-seq and targeted approaches like TMS strike a balance between coverage and cost, particularly for studies requiring high data quality and reduced input requirements [113].
In clinical diagnostics, particularly for cancer, DNA methylation biomarkers have shown significant promise due to their early emergence in tumorigenesis and stability in circulating cell-free DNA [9] [8]. The SPOGIT blood-based test for gastrointestinal cancers demonstrates the clinical potential of methylation biomarkers, achieving 88.1% sensitivity and 91.2% specificity in a multicenter validation cohort [114]. Similarly, methylation-based classifiers for central nervous system tumors have shown diagnostic accuracy exceeding 95% using array-based technologies [82].
Liquid biopsy applications present unique considerations for technology selection. The low abundance of circulating tumor DNA, particularly in early-stage cancers, requires highly sensitive methods [9] [8]. Targeted approaches like bisulfite PCR and digital PCR offer the sensitivity needed for clinical detection of rare methylation events in blood samples [8]. The choice of liquid biopsy source (blood, urine, CSF) also significantly impacts detection performance, with local sources often providing higher biomarker concentrations for cancers in proximity to these fluids [8].
The optimal choice of DNA methylation detection technology depends on the specific research questions, sample types, and resource constraints. WGBS remains the gold standard for comprehensive methylome analysis but at higher costs. EPIC arrays offer cost-effectiveness for large studies targeting known CpG sites. EM-seq emerges as a robust alternative to WGBS, providing similar coverage with improved DNA preservation. ONT sequencing enables unique applications in long-range methylation profiling and challenging genomic regions despite lower concordance with other methods.
Future developments in methylation profiling will likely focus on reducing costs while maintaining accuracy, improving analytical sensitivity for liquid biopsy applications, and enhancing computational methods for data integration from multiple platforms. The continued refinement of these technologies will expand their implementation in both basic research and clinical diagnostics, ultimately advancing our understanding of epigenetic regulation in health and disease.
Multi-cancer early detection (MCED) tests represent a paradigm shift in oncology, moving from single-cancer screening to a approach that can detect multiple cancers from a single blood draw. For researchers and drug development professionals, understanding the real-world performance of these tests—particularly their sensitivity and specificity—is crucial for evaluating their clinical potential and methodological robustness. This guide provides a comparative analysis of leading MCED technologies, focusing on their performance metrics, underlying methodologies, and the biochemical tools that power this innovative field. Performance data summarized in the table below reveal a consistent pattern of high specificity (≥90%) across major tests, with sensitivity figures that demonstrate particular strength in detecting cancers that currently lack standard screening options.
Table 1: Comparative Performance of Leading MCED Tests in Clinical and Real-World Studies
| Test Name (Company) | Core Technology | Reported Sensitivity (Overall) | Reported Specificity | Key Cancer Types Detected | Study Type & Population |
|---|---|---|---|---|---|
| Galleri (GRAIL) [115] [116] | Targeted Methylation Sequencing | 40.4% (All cancers), 73.7% (for 12 high-signal cancers) [115] | 99.6% [115] | >50 types; ~75% without recommended screenings [115] | PATHFINDER 2 Interventional Study (N=23,161) [115]; Real-World (N=111,080) [116] |
| OncoSeek [117] | AI + 7 Protein Tumor Markers | 58.4% (All cohorts combined) [117] | 92.0% (All cohorts combined) [117] | 14 common types (e.g., Pancreas: 79.1%, Lung: 66.1%, Colorectum: 51.8%) [117] | Multi-centre Validation (7 cohorts, N=15,122) [117] |
| Carcimun [118] | Conformational Plasma Protein Changes | 90.6% [118] | 98.2% [118] | Various solid tumors (e.g., GI Cancers, Lung) [118] | Prospective, Single-Blinded Study (N=172) |
Experimental Protocols & Methodologies
Targeted Methylation Sequencing (Galleri)
The Galleri test is a prominent example of a methylation-based MCED. Its experimental workflow, validated in large-scale studies like PATHFINDER 2, involves the following key steps [115] [116]:
- Sample Collection and Processing: A peripheral blood sample is collected from eligible individuals (typically adults aged 50+ with elevated cancer risk). Cell-free DNA (cfDNA) is isolated from the plasma component.
- Targeted Methylation Sequencing: The extracted cfDNA undergoes next-generation sequencing (NGS) focused on a pre-defined panel of genomic regions with high potential for cancer-associated methylation patterns. This targeted approach allows for efficient and deep sequencing.
- Bioinformatic Analysis & Machine Learning: The sequencing data is processed using machine learning classifiers trained on large reference datasets (like the Circulating Cell-Free Genome Atlas study). These algorithms analyze the methylation patterns to perform two critical functions:
- Cancer Signal Detection: Determine the presence or absence of a cancer-associated signal.
- Cancer Signal Origin (CSO) Prediction: For a positive signal, predict the tissue or organ where the cancer originated.
- Outcome Analysis: In interventional studies like PATHFINDER 2, participants with a "Cancer Signal Detected" result undergo diagnostic workups based on the predicted CSO. Performance metrics, including sensitivity, specificity, and positive predictive value (PPV), are then calculated based on confirmed diagnoses.
This methodology demonstrated in a real-world analysis of over 111,000 tests a cancer signal detection rate of 0.91% and a CSO prediction accuracy of 87%, facilitating a median time to diagnosis of 39.5 days [116].
Multi-Modal Biomarker Integration (OncoSeek)
The OncoSeek test employs a different, cost-effective strategy that integrates multiple types of biomarker data [117]:
- Biomarker Assay: The concentrations of seven selected protein tumor markers (PTMs) are measured in a blood sample using immunoassay platforms (e.g., Roche Cobas e411/e601 or Bio-Rad Bio-Plex 200).
- Data Integration with Clinical Features: The measured PTM levels are combined with individual clinical data, such as the patient's age and gender.
- AI-Powered Risk Stratification: An artificial intelligence (AI) model processes the multi-modal input (PTMs + clinical data) to calculate a probability score for the presence of cancer. This approach is designed to be more accessible, especially for low- and middle-income countries.
- Tissue of Origin (TOO) Prediction: For samples classified as positive, the model also provides a prediction for the tissue of origin.
This protocol was validated across seven independent cohorts from three countries, demonstrating consistent performance with an area under the curve (AUC) of 0.829, confirming its robustness across diverse populations and platforms [117].
Signaling Pathways & Experimental Workflows
The following diagram illustrates the core workflow shared by many MCED tests, highlighting the critical steps from sample acquisition to clinical reporting.
Diagram 1: Generalized MCED Test Workflow. The process begins with a blood draw, followed by plasma separation and biomarker extraction. Analysis branches into different technological paths (e.g., methylation sequencing or protein quantification), the outputs of which are integrated by bioinformatic and AI models to generate a clinical report.
The Scientist's Toolkit: Research Reagent Solutions
The development and execution of MCED tests rely on a suite of specialized reagents and tools. The table below details key components essential for research in this field.
Table 2: Essential Research Reagents and Kits for MCED Development
| Research Tool | Primary Function | Key Characteristics & Applications |
|---|---|---|
| Bisulfite Conversion Kits | Chemical conversion of unmethylated cytosine to uracil for downstream sequencing or PCR. | Foundation of WGBS and RRBS; can cause DNA degradation leading to sequencing bias [44] [119]. |
| Enzymatic Methyl-seq (EM-seq) | Enzyme-based conversion as an alternative to bisulfite treatment for detecting 5mC and 5hmC [120]. | Preserves DNA integrity, offers more uniform GC coverage, and is compatible with low DNA input (as low as 10 ng) [44] [120]. |
| Methylation-Sensitive Restriction Enzymes | Digest DNA in a methylation-dependent manner for enrichment or analysis. | Useful for targeted methylation studies; methylation status determination is limited to enzyme recognition sites [120]. |
| Methylated DNA Immunoprecipitation (MeDIP) Kits | Enrich methylated DNA fragments using 5mC-specific antibodies for sequencing or array analysis. | Does not provide single-base resolution; data can be skewed towards highly methylated regions [119] [120]. |
| Infinium MethylationEPIC BeadChip | Array-based profiling of over 935,000 CpG sites across the genome [44]. | Cost-effective for large cohort studies; coverage is limited to pre-designed CpG sites [44] [119]. |
| Targeted Methylation Panels | Custom or pre-designed panels for deep sequencing of cancer-relevant genomic regions. | Maximizes sequencing depth and cost-efficiency for validating biomarker panels; used in tests like Galleri [115] [119]. |
Critical Analysis of MCED Performance
The performance data reveals several key insights for researchers. First, the high specificity (≥90%) common to most tests is a deliberate design priority to minimize false positives and prevent overburdening healthcare systems with unnecessary diagnostic workups [116] [117]. Second, while overall sensitivity is moderate for some tests, they show strength in detecting cancers that currently lack recommended screening, such as pancreatic and biliary tract cancers [115] [117]. This addresses a significant unmet clinical need. Third, the accurate prediction of the tissue of origin (87-92%) is a critical feature that facilitates a more efficient and directed diagnostic pathway for clinicians [115] [116].
The choice of underlying technology also involves important trade-offs. Methylation-based methods (e.g., Galleri) can achieve high sensitivity and specificity due to the stability and cancer-specificity of DNA methylation patterns [8] [119]. However, these often require sophisticated NGS infrastructure and complex bioinformatics. In contrast, protein-based assays (e.g., OncoSeek) offer a more accessible and cost-effective platform but may face challenges in achieving high sensitivity for all cancer types, particularly at very early stages [117] [121]. The integration of machine learning is now a cornerstone of MCED development, enabling the synthesis of complex, multi-modal data to improve both detection and origin prediction [117] [119]. As the field evolves, the focus will be on enhancing sensitivity for early-stage disease, validating performance in diverse populations, and seamlessly integrating these tests into existing clinical screening paradigms.
The transition of DNA methylation biomarkers from research settings to routine clinical practice represents a significant advancement in precision oncology. These biomarkers, which detect chemical modifications to DNA that regulate gene expression without altering the DNA sequence itself, have emerged as powerful tools for cancer detection, monitoring, and prognosis [8]. The inherent stability of DNA methylation patterns, which are often altered in early tumorigenesis and remain consistent throughout cancer progression, makes them particularly valuable as clinical biomarkers [8]. This review examines two successfully translated methylation biomarker technologies: the SEPT9 assay for colorectal cancer (CRC) screening and the Shield multi-cancer detection (MCD) test, analyzing their performance characteristics, methodological foundations, and positions within the evolving landscape of cancer diagnostics.
SEPT9 Methylation Biomarker for Colorectal Cancer
Performance and Clinical Utility
The SEPT9 (Septin 9) gene methylation assay was the first blood-based test approved by the FDA for colorectal cancer screening [122]. Its development was based on the key finding that the CpG island 3 at the promoter region of the SEPT9 gene V2 transcript is hypermethylated in colorectal cancer, and this methylated DNA is released into the peripheral blood from necrotic and apoptotic cancer cells [122].
Table 1: Diagnostic Performance of SEPT9 in Colorectal Cancer Detection
| Study | Sample Size | Sensitivity (%) | Specificity (%) | AUC | Notes |
|---|---|---|---|---|---|
| 2022 Chinese Cohort [123] | 616 CRC patients, 122 controls | 72.94 | 81.97 | 0.826 | Superior to CEA and CA19-9 |
| Meta-analysis (2017) [122] | 2,613 CRC cases, 6,030 controls | 48.2-95.6 (variable by algorithm) | 79.1-99.1 (variable by algorithm) | - | Performance depends on algorithm used |
| Indian Cohort (2023) [124] | 45 CRC patients | 6.66 (complete methylation) | - | - | Highlights population-specific variations |
A 2022 study conducted with Chinese patients demonstrated that mSEPT9 achieved significantly higher sensitivity (72.94%) and area under the curve (AUC) value (0.826) compared to traditional serum protein markers CEA (43.96% sensitivity, 0.789 AUC) and CA19-9 (14.99% sensitivity, 0.590 AUC) [123]. The combination of mSEPT9 with CEA and CA19-9 further improved diagnostic performance to 78.43% sensitivity, 86.07% specificity, and 0.878 AUC [123].
The test's performance is significantly influenced by the algorithm used for interpreting results. A comprehensive meta-analysis revealed that different algorithms offer distinct performance characteristics: the 1/3 algorithm (one positive result out of three PCR replicates) provides the highest sensitivity (78%) with lower specificity (84%), while the 2/3 algorithm (two positive results out of three PCR replicates) offers the best balance with 73% sensitivity and 96% specificity [122]. This algorithm-dependent performance allows clinicians to select testing parameters based on clinical context, whether for broad screening (favoring sensitivity) or diagnostic confirmation (favoring specificity).
Beyond diagnosis, SEPT9 methylation status shows significant correlation with clinicopathological features, including TNM stage, T stage, N stage, tumor size, vascular invasion, and nerve invasion [123]. Notably, studies have demonstrated a 100% correlation between positive mSEPT9 test results and recurrence or metastasis in patients after therapeutic intervention, suggesting its utility as a noninvasive marker for monitoring treatment response and disease recurrence [123].
Experimental Protocol for SEPT9 Detection
The standard methodology for detecting methylated SEPT9 in clinical samples involves a multi-step process centered on bisulfite conversion and methylation-specific polymerase chain reaction (PCR).
Sample Preparation and Bisulfite Conversion:
- Plasma Isolation: 10 mL of venous blood is collected in K2EDTA tubes and processed via double centrifugation at 1,400 × g for 12 minutes to obtain platelet-free plasma [123].
- DNA Extraction: Cell-free DNA is extracted from plasma samples using commercial kits [123].
- Bisulfite Conversion: Extracted DNA is treated with bisulfite, which converts unmethylated cytosine residues to uracil, while methylated cytosines remain unchanged [123]. This critical step enables subsequent discrimination between methylated and unmethylated DNA sequences.
Detection and Analysis:
- Methylation-Specific PCR: The bisulfite-converted DNA is amplified using real-time PCR with methylation-specific primers and probes. PCR-blocking oligonucleotides are used to further enhance specificity by suppressing amplification of unmethylated sequences [123].
- Thermocycling Conditions: The typical protocol includes activation at 94°C for 20 minutes; 45 cycles of 62°C for 5 seconds, 55.5°C for 35 seconds, and 93°C for 30 seconds; and final cooling at 40°C for 5 seconds [123].
- Result Interpretation: A valid test requires the internal control gene (β-actin, ACTB) to have a cycle threshold (Ct) ≤32.1. For SEPT9, a Ct value ≤41.0 is considered positive, while undetermined Ct or Ct >41.0 is considered negative [123]. Different algorithms (1/3, 2/3) can be applied when multiple PCR replicates are run.
Figure 1: SEPT9 Methylation Detection Workflow. The process involves sample collection, DNA extraction, bisulfite conversion, and methylation-specific detection. The yellow-highlighted steps are critical for methylation status determination.
Shield Multi-Cancer Detection Test
Performance and Clinical Applications
The Shield test, developed by Guardant Health, represents the evolution of methylation biomarkers from single-cancer to multi-cancer early detection (MCED). This blood-based test utilizes cell-free DNA methylation patterns to simultaneously screen for multiple cancer types and has received FDA Breakthrough Device designation [125] [126].
Table 2: Performance of the Shield Multi-Cancer Detection Test
| Cancer Type | Sensitivity (%) | Primary or Secondary CSO Accuracy (%) |
|---|---|---|
| Overall (10 tumor types) | 60 | 89 |
| Six Most Aggressive Cancers* | 74 | - |
| Esophageal-Gastric | 96 | 92 |
| Hepatocellular | 94 | 73 |
| Colorectal | 83 | 94 |
| Lung | 67 | 97 |
| Ovarian | 70 | 93 |
| Pancreas | 68 | 80 |
| Bladder | 62 | 75 |
| Breast | 45 | 92 |
| Prostate | 21 | 83 |
*Includes esophageal-gastric, hepatocellular, lung, ovarian, and pancreas cancers [125]
Data presented at the 2025 American Association for Cancer Research (AACR) annual meeting demonstrated that the Shield MCD test achieved 98.5% specificity with 60% overall sensitivity across ten tumor types [125]. Notably, sensitivity increased to 74% across the six most aggressive cancers (defined by shortest survival rates), highlighting its potential for detecting malignancies with significant mortality impact [125]. The test also demonstrated 89% accuracy for predicting the cancer signal of origin (CSO), which is critical for guiding subsequent diagnostic workups [125].
The Shield test's selection by the National Cancer Institute for inclusion in its upcoming Vanguard Study, which will evaluate emerging MCD technologies, further validates its potential role in population-level cancer screening [125]. This is particularly significant for cancers like pancreatic and ovarian, which currently lack effective screening methods and are often diagnosed at advanced stages [121].
Technical Methodology
The Shield test employs a targeted methylation sequencing approach that differs methodology from the PCR-based SEPT9 assay:
Sample Processing and Library Preparation:
- Cell-free DNA Isolation: Cell-free DNA is extracted from plasma samples obtained through standard blood draws.
- Library Construction: DNA libraries are prepared for sequencing, incorporating adapters compatible with next-generation sequencing platforms.
- Targeted Methylation Analysis: Unlike whole-genome bisulfite sequencing, Shield uses a targeted approach focusing on specific genomic regions with known cancer-specific methylation patterns.
Analysis and Interpretation:
- Sequencing: Libraries are sequenced using high-throughput platforms, generating millions of reads covering the targeted methylation sites.
- Bioinformatic Analysis: Advanced algorithms analyze methylation patterns across the targeted regions to detect the presence of cancer-derived signals.
- Machine Learning Classification: Sophisticated classification models, trained on large datasets of cancer and normal samples, integrate methylation data to determine cancer presence and predict tissue of origin [125] [121].
The test's ability to integrate multiple biomarker types, potentially including genomic mutations and DNA fragmentation patterns alongside methylation data, contributes to its robust performance across multiple cancer types [121].
Figure 2: Shield Test Methodology. The Shield test utilizes targeted methylation sequencing and machine learning classification to provide both cancer detection and tissue of origin prediction. The green-highlighted steps represent key technological differentiators.
Comparative Analysis and Research Implications
Performance and Application Comparison
Table 3: Comparative Analysis of SEPT9 and Shield Tests
| Parameter | SEPT9 Assay | Shield Test |
|---|---|---|
| Intended Use | Colorectal cancer screening and monitoring | Multi-cancer early detection (10+ types) |
| Technology Platform | Bisulfite conversion + methylation-specific PCR | Targeted methylation sequencing + machine learning |
| Sample Type | Plasma | Plasma |
| Overall Sensitivity | 48.2-95.6% (algorithm-dependent) [122] | 60% (across 10 cancers) [125] |
| Overall Specificity | 79.1-99.1% (algorithm-dependent) [122] | 98.5% [125] |
| Key Strength | Established CRC-specific biomarker, cost-effective for single cancer | Broad cancer coverage, cancer signal of origin prediction |
| Clinical Context | CRC screening in at-risk populations, recurrence monitoring | Asymptomatic screening for multiple cancers |
| Regulatory Status | FDA-approved for CRC screening [122] | FDA Breakthrough Device Designation [126] |
The comparison reveals complementary profiles: SEPT9 offers a focused solution for colorectal cancer with well-established performance characteristics and lower complexity, while Shield provides a comprehensive approach for multi-cancer detection, leveraging advanced sequencing and computational methods. The selection between these technologies depends on clinical context, with SEPT9 being appropriate for targeted CRC screening and Shield offering a broader screening approach for multiple cancer types.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for Methylation Biomarker Studies
| Reagent/Category | Specific Examples | Research Function |
|---|---|---|
| Sample Collection | K2EDTA tubes [123], cell-free DNA collection tubes | Preserves sample integrity, prevents coagulation and genomic DNA contamination |
| Nucleic Acid Extraction | MagMAX Cell-Free DNA Isolation Kit [127], QIAamp Mini columns [124] | Isolves high-quality cell-free DNA from plasma/serum with minimal contamination |
| Bisulfite Conversion | EZ DNA Methylation kits, CT Conversion Reagent [124] | Chemically converts unmethylated cytosines to uracils for methylation status discrimination |
| Target Amplification | EpiTaq polymerase (bisulfite-treated DNA) [124], Hieff NGS Ultima Pro DNA Library Prep Kit [127] | Amplifies target sequences with fidelity while maintaining methylation information |
| Methylation Detection | Methylation-specific primers/probes [123], TET-assisted pyridine borane sequencing reagents [127] | Enables specific detection and quantification of methylated vs. unmethylated loci |
| Enzymes for Conversion | TET2 oxidase enzyme [127], proteinase K [124] | Facilitates bisulfite-free conversion methods and sample digestion |
| Sequencing Platforms | ABI7500 fluorescent PCR instrument [123], Gene+seq2000 sequencer [127] | Provides the instrumentation for quantitative PCR and next-generation sequencing |
The successful translation of SEPT9 and Shield methylation biomarkers from research concepts to clinical tools demonstrates the significant potential of DNA methylation analysis in oncology. These case studies highlight distinct translation pathways: targeted PCR-based assays for specific cancer types and comprehensive sequencing-based approaches for multi-cancer detection. Both technologies face shared challenges, including optimization of sensitivity and specificity, standardization across populations, and integration into healthcare systems [8] [121].
Future development in this field will likely focus on refining multi-cancer early detection tests, validating biomarkers in diverse populations, and establishing clinical guidelines for the appropriate use of these technologies. As the field advances, the integration of methylation biomarkers with other molecular data types promises to further enhance the precision and utility of cancer detection and monitoring strategies. The ongoing Vanguard Study evaluating Shield and other MCD tests will provide critical evidence regarding the real-world implementation and impact of these innovative diagnostic platforms [125].
The translation of DNA methylation biomarkers from research discoveries to clinically validated diagnostic tools requires rigorous validation frameworks that ensure reliability, reproducibility, and clinical utility. DNA methylation, an epigenetic modification involving the addition of a methyl group to cytosine residues at CpG dinucleotides, regulates gene expression without altering the underlying DNA sequence [9]. In cancer, aberrant methylation patterns emerge early in tumorigenesis and remain stable throughout tumor evolution, making them ideal biomarkers for early detection, prognosis, and monitoring [8]. However, the journey from initial discovery to clinical implementation presents significant challenges, with only a few methylation-based tests successfully transitioning to routine clinical use despite extensive research publications [8].
The validation framework for DNA methylation biomarkers spans multiple critical phases, including analytical validation to assess technical performance, clinical validation to establish diagnostic accuracy, and independent verification to confirm real-world utility. This process must account for sample type variability, technological platforms, and biological heterogeneity while maintaining stringent standards for sensitivity and specificity. The stability of DNA methylation patterns, combined with the inherent stability of the DNA double helix, provides advantageous properties for biomarker development compared to more labile molecules such as RNA [8]. Nevertheless, successful clinical translation requires carefully designed workflows that address pre-analytical variables, analytical performance, and clinical relevance across diverse patient populations.
Performance Comparison of Methylation Detection Technologies
The selection of appropriate analytical methods is fundamental to robust methylation biomarker validation. Various technologies offer distinct advantages and limitations in sensitivity, specificity, throughput, and clinical applicability. Understanding these trade-offs enables researchers to select optimal platforms for each validation stage.
Table 1: Comparative Analysis of Major Methylation Detection Platforms
| Technology | Sensitivity | Specificity | Throughput | Key Applications | Limitations |
|---|---|---|---|---|---|
| Digital PCR (dPCR) | 98.03%-99.08% [80] | 99.62%-100% [80] | Medium | Target validation, liquid biopsy analysis [80] [8] | Limited multiplexing, target-specific |
| Next-Generation Sequencing (WGBS/RRBS) | Varies by coverage | Single-base resolution [9] [119] | High | Biomarker discovery, genome-wide profiling [9] [119] | Higher cost, computational demands |
| Methylation Microarrays | High for targeted sites | High for designed probes [119] | High | Population studies, diagnostic signatures [119] | Limited to predefined CpG sites |
| Third-Generation Sequencing | Enables haplotype resolution | Direct detection without bisulfite [119] | Medium-High | Structural variation, allele-specific methylation [119] | Higher error rates, specialized equipment |
Table 2: Platform-Specific Performance Metrics in Validation Studies
| Platform | Sample Type | Validation Cohort | Key Performance Metrics | Reference |
|---|---|---|---|---|
| QIAcuity dPCR | FFPE breast cancer tissues (n=141) | CDH13 promoter methylation | Sensitivity: 99.08%, Specificity: 99.62% [80] | [80] |
| QX200 ddPCR | FFPE breast cancer tissues (n=141) | CDH13 promoter methylation | Sensitivity: 98.03%, Specificity: 100% [80] | [80] |
| Integrated RNA/DNA Exome | 2230 clinical tumor samples | Multi-platform orthogonal validation | Actionable alterations in 98% of cases [128] | [128] |
| Targeted Methylation Sequencing | Plasma ctDNA | Multi-cancer early detection | High specificity, improved sensitivity for early-stage cancers [119] | [119] |
Digital PCR platforms, including both nanoplate-based and droplet-based systems, demonstrate particularly strong performance for targeted methylation validation. A direct comparison of the QIAcuity dPCR System (Qiagen) and QX200 Droplet Digital PCR System (Bio-Rad) for CDH13 gene methylation detection in 141 breast cancer tissue samples revealed excellent correlation (r = 0.954) between both methods despite their different technological approaches [80]. This high concordance suggests that selection between these platforms may depend on practical considerations such as workflow time and complexity, instrument requirements, and specific experimental needs rather than fundamental performance differences [80].
Experimental Protocols for Robust Validation
Analytical Validation Framework
Robust analytical validation begins with standardized laboratory procedures and appropriate reference materials. The validation of an integrated RNA and DNA exome sequencing approach provides a comprehensive framework for establishing technical reliability [128]. This protocol emphasizes three critical validation steps: (1) analytical validation using custom reference samples containing known mutations; (2) orthogonal testing in patient samples; and (3) assessment of clinical utility in real-world cases [128].
For DNA methylation analysis specifically, the workflow typically begins with sample preparation and bisulfite conversion. The comparative dPCR study exemplifies a standardized protocol: genomic DNA is isolated from formalin-fixed, paraffin-embedded (FFPE) tissues using commercial kits (DNeasy Blood and Tissue Kit, Qiagen), with DNA quantification via fluorometric methods (Qubit 3.0) [80]. One microgram of isolated DNA undergoes bisulfite modification using dedicated kits (EpiTect Bisulfite Kit, Qiagen) following manufacturer protocols [80]. For dPCR analysis, reaction mixtures are prepared with platform-specific master mixes, optimized primer and probe concentrations, and DNA template, then partitioned for amplification and fluorescence detection [80].
Orthogonal Verification Methods
Orthogonal verification using different methodological principles is essential for rigorous biomarker validation. The integrated RNA/DNA sequencing approach employed multiple verification steps, including comparison to established clinical assays and cross-platform validation [128]. For methylation-specific analyses, bisulfite pyrosequencing, methylation-sensitive restriction enzyme digestion, or different sequencing platforms can provide orthogonal confirmation of initial findings.
Liquid biopsy validation presents particular challenges due to low circulating tumor DNA (ctDNA) fractions, especially in early-stage cancers. The EXTECTOR study demonstrated a protocol for urine-based bladder cancer detection achieving 87% sensitivity for TERT promoter mutations, significantly outperforming plasma-based detection (7% sensitivity) [8]. This highlights how appropriate sample source selection critically impacts assay performance during validation.
Visualization of Validation Workflows
Figure 1: Comprehensive Biomarker Validation Workflow from Discovery to Implementation
Method-Specific Experimental Protocols
Digital PCR Methylation Analysis Protocol
The direct comparison between nanoplate-based and droplet-based dPCR systems provides a detailed protocol for methylation-specific digital PCR [80]. For the QIAcuity Digital PCR System, reactions are prepared in 12μL volumes containing 3μL of 4× Probe PCR master mix, 0.96μL of each primer, 0.48μL of each probe (FAM-labeled for methylated sequences, HEX-labeled for unmethylated sequences), 2.5μL of bisulfite-converted DNA template, and RNase-free water [80]. The mixture is pipetted into 24-well nanoplates (8,500 partitions per well) and processed with the following thermal cycling conditions: initial heat activation at 95°C for 2 minutes, followed by 40 cycles of denaturation at 95°C for 15 seconds and combined annealing/extension at 57°C for 1 minute [80].
For the QX200 Droplet Digital PCR System, reaction mixtures contain 10μL of Supermix for Probes, 0.45μL of each primer, 0.45μL of each probe, 2.5μL of DNA template, adjusted to 20μL with RNase-free water [80]. Approximately 20,000 droplets per sample are generated using the QX200 Droplet Generator, followed by endpoint PCR with the following conditions: initial denaturation at 95°C for 10 minutes, 40 cycles of denaturation at 94°C for 30 seconds and annealing/extension at 57°C for 1 minute, followed by enzyme deactivation [80].
Both systems require appropriate threshold setting and quality control measures. The QIAcuity study established manual thresholds at a value of 45, with acceptance criteria requiring over 7,000 valid partitions and at least 100 positive partitions [80]. Methylation levels are expressed as the ratio of FAM-positive partitions (methylated) to the sum of all positive partitions detected in both channels [80].
Integrated Multi-Omics Validation Protocol
The combined RNA and DNA exome sequencing approach exemplifies a comprehensive validation framework for complex biomarkers [128]. For DNA sequencing, libraries are prepared from 10-200ng of extracted DNA using exome capture kits (SureSelect XTHS2 DNA), with hybridization capture using the SureSelect Human All Exon V7 exome probe [128]. For RNA sequencing, library construction utilizes either the TruSeq stranded mRNA kit (for fresh frozen tissue) or the SureSelect XTHS2 RNA kit (for FFPE tissue) [128]. Sequencing is performed on Illumina NovaSeq 6000 platforms with stringent quality control metrics (Q30 > 90%, PF > 80%) [128].
Bioinformatic processing includes alignment to the hg38 reference genome using BWA for DNA and STAR for RNA sequencing data [128]. Variant calling employs multiple algorithms: Strelka for somatic SNVs and INDELs, Manta for small INDEL candidates, and Pisces for variants from RNA-seq data [128]. This multi-algorithm approach enhances detection sensitivity while maintaining specificity through subsequent filtration steps.
Research Reagent Solutions for Methylation Validation
Table 3: Essential Research Reagents for Methylation Detection Assays
| Reagent Category | Specific Products | Function in Validation | Key Considerations |
|---|---|---|---|
| Nucleic Acid Isolation | DNeasy Blood & Tissue Kit (Qiagen), AllPrep DNA/RNA FFPE Kit (Qiagen) [80] [128] | Preserves nucleic acid integrity, especially from challenging samples like FFPE | DNA yield, fragment size distribution, purity metrics (A260/280) |
| Bisulfite Conversion | EpiTect Bisulfite Kit (Qiagen) [80] | Converts unmethylated cytosines to uracils, enabling methylation discrimination | Conversion efficiency, DNA fragmentation, yield recovery |
| PCR Master Mixes | QIAcuity 4× Probe PCR Master Mix, Supermix for Probes (Bio-Rad) [80] | Provides optimized enzyme blends for amplification | Compatibility with probe chemistry, inhibitor resistance |
| Library Preparation | SureSelect XTHS2 (Agilent), TruSeq stranded mRNA (Illumina) [128] | Prepares sequencing libraries from input DNA/RNA | Input requirements, capture efficiency, complexity |
| Quality Control | Qubit assays, TapeStation, Bioanalyzer [128] | Quantifies and qualifies nucleic acids throughout workflow | Sensitivity, accuracy, compatibility with sample type |
Advanced Technologies in Methylation Validation
Machine Learning-Enhanced Validation
Machine learning approaches are increasingly integrated into methylation biomarker validation, addressing complex pattern recognition challenges beyond conventional statistical methods. Conventional supervised methods, including support vector machines, random forests, and gradient boosting, have been employed for classification, prognosis, and feature selection across tens to hundreds of thousands of CpG sites [119]. More recently, transformer-based foundation models pretrained on extensive methylation datasets show promise for improved generalizability across diverse populations [119].
These advanced computational methods enable the development of methylation-based classifiers that standardize diagnoses across multiple cancer subtypes. For central nervous system tumors, such a classifier altered histopathologic diagnosis in approximately 12% of prospective cases while providing online portals facilitating routine pathology application [119]. Similarly, genome-wide episignature analysis in rare diseases utilizes machine learning to correlate patient blood methylation profiles with disease-specific signatures, demonstrating clinical utility in genetics workflows [119].
Emerging Sequencing Technologies
Third-generation sequencing platforms offer innovative approaches for methylation validation by enabling direct detection of base modifications without bisulfite conversion. Oxford Nanopore Technologies provides long-read sequencing capability that supports real-time analysis without PCR amplification and allows simultaneous profiling of CpG methylation and chromatin accessibility [119]. The nanoNOMe method exemplifies this approach, facilitating allele-specific epigenetic studies on native long DNA strands [119].
Single-cell DNA methylation profiling has emerged as a transformative approach for addressing cellular heterogeneity in validation cohorts. Techniques such as single-cell bisulfite sequencing (scBS-seq) and single-cell reduced representation bisulfite sequencing (scRRBS) enable high-resolution insights into DNA methylation heterogeneity, particularly valuable in complex diseases like cancer where they reveal epigenetic variations driving intra-tissue heterogeneity and treatment resistance [119].
Robust validation of DNA methylation biomarkers requires a comprehensive, multi-stage approach that addresses analytical performance, clinical utility, and independent verification. The framework presented here emphasizes rigorous experimental design, appropriate technology selection, and systematic progression from discovery to implementation. As methylation-based diagnostics continue to evolve, adherence to these validation principles will ensure the translation of promising biomarkers into clinically impactful tools that enhance patient care across diverse disease contexts.
The integration of advanced technologies, including machine learning, long-read sequencing, and single-cell approaches, offers exciting opportunities to enhance validation stringency while addressing the complexities of biological systems. By implementing these guidelines, researchers can accelerate the development of reliable, clinically implementable methylation biomarkers that fulfill their promise in personalized medicine.
Conclusion
The accurate assessment of sensitivity and specificity is paramount for translating DNA methylation research into reliable clinical diagnostics. As this review outlines, method selection must be guided by the specific clinical question, weighing factors such as required resolution, sample type, and cost. While established methods like WGBS and microarrays remain pillars, enzymatic and third-generation sequencing methods are emerging as powerful alternatives that overcome key limitations. The future of the field lies in the integration of these advanced technologies with sophisticated machine learning models to unlock higher diagnostic precision from complex methylation data. Ultimately, a rigorous, validation-focused approach is the critical bridge from promising biomarker discovery to impactful clinical tools that can improve patient outcomes through early detection and monitoring.
References
- 1. Statistics | Sensitivity, Specificity, PPV and NPV [https://geekymedics.com/sensitivity-specificity-ppv-and-npv/]
- 2. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 3. Understanding PPV and NPV in Healthcare Testing [https://harbinger-health.com/2024/09/26/understanding-ppv-and-npv-in-healthcare-testing-crucial-tools-for-diagnostic-accuracy/]
- 4. Sensitivity, Specificity, and Predictive Values: Foundations, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5701930/]
- 5. DNA methylation markers as a triage test for identification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6587981/]
- 6. Diagnostic Accuracy of DNA-Methylation in Detection ... [https://www.mdpi.com/2072-6694/16/11/1986]
- 7. Cytological DNA methylation for cervical cancer screening [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1181982/full]
- 8. a roadmap for DNA methylation biomarkers in liquid biopsies [https://www.nature.com/articles/s41388-025-03624-5]
- 9. Advancements in DNA methylation technologies and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12309559/]
- 10. The Years 2015–2025 as a Prospective Decade for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467249/]
- 11. SpPin and SnNout [https://www.cebm.ox.ac.uk/resources/ebm-tools/sppin-and-snnout]
- 12. Ruling a diagnosis in or out with “SpPIn” and “SnNOut” [https://pmc.ncbi.nlm.nih.gov/articles/PMC487735/]
- 13. Application of novel and existing methods to identify genes ... [https://bmcgenomdata.biomedcentral.com/articles/10.1186/s12863-018-0647-2]
- 14. SpPin and SnNout Are Not Enough. It's Time to Fully Embrace ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10361927/]
- 15. Questioning the "SPIN and SNOUT" rule in clinical testing [https://pubmed.ncbi.nlm.nih.gov/30891312/]
- 16. Test Diagnostics [https://www.physio-pedia.com/Test_Diagnostics]
- 17. Teaching Diagnostic Test Accuracy: Limitations of SpPIn- ... [https://www.jblearning.com/blog/jbl/2020/06/08/teaching-diagnostic-test-accuracy-with-sppin-snnout?srsltid=AfmBOorWGj-s1cfLrFTtt-jpavPpt56LhrwGMmna1Nz3XP59n10_Hk39]
- 18. Beyond SpPIN and SnNOUT: Considerations with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2704350/]
- 19. Non-invasive early detection of cancer four years before ... [https://www.nature.com/articles/s41467-020-17316-z]
- 20. Stability of Blood DNA Methylation Across Two Timepoints in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11592101/]
- 21. Use of DNA methylation patterns for early detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11964873/]
- 22. The advances of DNA methylation in the liquid biopsy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12259442/]
- 23. An Overview of DNA Methylation Analysis Methods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3624772/]
- 24. Liquid biopsy: unveiling methylation biomarkers for early ... [https://biomodal.com/blog/liquid-biopsy-unveiling-methylation-biomarkers-for-early-cancer-diagnosis/]
- 25. Methylation Sensitive and Methylation Dependent ... [https://www.neb.com/en-us/products/epigenetics/methylation-analysis/methylation-restriction-enzymes-epigenetics?srsltid=AfmBOorNQtD3YFbK0Sik6jp4C5VX5qRD8DVBs938Gbq6s67pPGRlDkIQ]
- 26. DNA Methylation: An Emerging Biomarker for Cancer ... [https://www.thermofisher.com/blog/behindthebench/dna-methylation-an-emerging-biomarker-for-cancer-research/]
- 27. DNA methylation and machine learning - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512482/]
- 28. Comprehensive comparison of enzymatic and bisulfite DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495756/]
- 29. Comparison of current methods for genome-wide DNA ... [https://epigeneticsandchromatin.biomedcentral.com/articles/10.1186/s13072-025-00616-3]
- 30. Comparison of whole-genome bisulfite sequencing library ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5856372/]
- 31. Characterizing the properties of bisulfite sequencing data ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-021-07721-z]
- 32. MeDIP-seq vs. RRBS vs. WGBS [https://www.cd-genomics.com/resource-medip-seq-vs-rrbs-vs-wgbs.html]
- 33. Comparison of sequencing-based methods to profile DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2955169/]
- 34. Variable performance of widely used bisulfite sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11957057/]
- 35. Cost-effective methylome sequencing of cell-free DNA for ... [https://www.nature.com/articles/s41467-022-32995-6]
- 36. Bisulfite sequencing, but at what cost? [https://www.neb.com/en-us/nebinspired-blog/bisulfite-sequencing-but-at-what-cost?srsltid=AfmBOoqNHoMK3-mCcV0T-0zUDW9jyzULizeYnTS87Jn8_uwd0kma_xdj]
- 37. Comparison of current methods for genome-wide DNA ... [https://pubmed.ncbi.nlm.nih.gov/40855329/]
- 38. Accounting for differences between Infinium ... [https://www.life-science-alliance.org/content/8/9/e202403155]
- 39. Accounting for differences between Infinium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12238762/]
- 40. Infinium MethylationEPIC v2.0 Kit | Methylation profiling array [https://www.illumina.com/products/by-type/microarray-kits/infinium-methylation-epic.html]
- 41. Microarray-Based DNA Methylation Profiling: Validation ... [https://www.sciencedirect.com/science/article/pii/S1525157824000345]
- 42. MethylCallR : a comprehensive analysis framework for ... [https://www.nature.com/articles/s41598-024-77914-5]
- 43. Comparative Performance of Methylation Array and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12589796/]
- 44. Comparison of current methods for genome-wide DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12376410/]
- 45. Enzymatic Methyl-seq: The Next Generation of Methylome ... [https://www.neb.com/en-us/tools-and-resources/feature-articles/enzymatic-methyl-seq-the-next-generation-of-methylome-analysis?srsltid=AfmBOorEj1BmZUGxtx7pb4Q1R-cxqCqfawc07OqU_vunLoMyLtEb_zag]
- 46. Comparison of Methods for DNA Methylation Analysis [https://www.neb.com/en-us/tools-and-resources/selection-charts/dna-methylation-table?srsltid=AfmBOop270N9Dro8XC4QwPJsMxe8dyauOqfHFd6a5WtNXT4EFWZQotdj]
- 47. WGBS vs. EM-seq: Key Differences in Principles, Pros ... [https://www.cd-genomics.com/resource-em-seq-wgbs-comparison-workflow-applications.html]
- 48. Ultra-mild bisulfite outperforms existing methods for 5- ... [https://www.nature.com/articles/s41467-025-66033-y]
- 49. The new NEBNext Enzymatic Methyl-seq (EM-seq) [https://www.neb-online.de/en/next-generation-sequencing/the-new-nebnext-enzymatic-methyl-seq-em-seq/]
- 50. Comprehensive comparison of enzymatic and bisulfite ... [https://pubmed.ncbi.nlm.nih.gov/41044668]
- 51. University of Chicago scientists develop ultra-mild bisulfite ... [https://physicalsciences.uchicago.edu/news/article/university-of-chicago-scientists-develop-ultra-mild-bisulfite-sequencing-to-preserve-dna-integrity-in-methylation-analysis/]
- 52. Multi-STEM MePCR: a bisulfite-free, multiplex, highly sensitive ... [https://pubs.rsc.org/en/content/articlelanding/2025/sc/d5sc01429h]
- 53. PacBio vs Oxford Nanopore: Which Long-Read ... [https://www.cd-genomics.com/resource-pacbio-oxford-nanopore-comparison.html]
- 54. Comparing long-read sequencing technologies [https://www.pacb.com/blog/sequencing-101-comparing-long-read-sequencing-technologies/]
- 55. Powered by PacBio: Selected publications from August 2025 [https://www.pacb.com/blog/powered-by-pacbio-selected-publications-from-august-2025/]
- 56. PacBio Announces Plans to Improve Methylation Detection ... [https://www.pacb.com/press_releases/pacbio-announces-plans-to-improve-methylation-detection-in-hifi-chemistry/]
- 57. A Hitchhiker's Guide to long-read genomic analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12047252/]
- 58. Science unlocked: publication picks from July 2025 [https://nanoporetech.com/blog/science-unlocked-publication-picks-from-july-2025]
- 59. Powered by PacBio:Selected publications from September ... [https://www.pacb.com/blog/powered-by-pacbioselected-publications-from-september-2025/]
- 60. Science unlocked: publication picks from August 2025 [https://nanoporetech.com/blog/science-unlocked-publication-picks-from-august-2025]
- 61. Science unlocked: publication picks from April 2025 [https://nanoporetech.com/blog/science-unlocked-publication-picks-from-april-2025]
- 62. dPCR vs qPCR [https://www.qiagen.com/us/applications/digital-pcr/beginners/dpcr-vs-qpcr]
- 63. Quantitative or digital PCR? A comparative analysis for ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993624001584]
- 64. Droplet Digital PCR versus qPCR for gene expression ... [https://www.nature.com/articles/s41598-017-02217-x]
- 65. Digital PCR outperforms quantitative real-time PCR for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288185/]
- 66. Comparison of quantitative PCR and digital PCR assays ... [https://pubmed.ncbi.nlm.nih.gov/38061673/]
- 67. Comparison of quantitative PCR and digital PCR assays ... [https://www.sciencedirect.com/science/article/pii/S0166093423001842]
- 68. Precision performance of Crystal Digital PCR vs. ... [https://www.stillatechnologies.com/digital-pcr/naica-system-analysis/precision-performance-of-crystal-digital-pcr-vs-quantitative-pcr/]
- 69. Single-cell multi-omic detection of DNA methylation and ... [https://www.nature.com/articles/s41592-025-02847-4]
- 70. 2025 Trends in Methylation and Epigenetic Testing [https://www.geneusdna.com/en-sa/blog/methylation-epigenetic-trends-2025?]
- 71. Liquid biopsy in cancer: current status, challenges and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11609310/]
- 72. A Review of Circulating Tumor DNA (ctDNA) and the Liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12032849/]
- 73. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 74. Enhancing the sensitivity of non-invasive cervical cancer ... [https://www.nature.com/articles/s41598-025-20050-5]
- 75. Chromogenic Substrates Overview [https://www.goldbio.com/blogs/articles/chromogenic-substrates-overview?srsltid=AfmBOop151Pyo-sXL6afYPZH5GedZ1P78rnKaNaZhoZp-Mly3ICq9rth]
- 76. Comparative performance evaluation of bisulfite [https://pmc.ncbi.nlm.nih.gov/articles/PMC11969950/]
- 77. A Researcher's Guide to Successful DNA Bisulfite Conversion [https://www.whatisepigenetics.com/a-researchers-guide-to-successful-dna-bisulfite-conversion/]
- 78. Ultrafast bisulfite sequencing detection of 5-methylcytosine ... [https://www.nature.com/articles/s41587-023-02034-w]
- 79. Analysis of DNA Methylation by Bisulfite Conversion [https://www.neb.com/en-us/products/epigenetics/methylation-analysis/bisulfite-conversion?srsltid=AfmBOopFDFtFilwBmJMuz0updopDd0dQcQSotE3-A_fDnlqfmLyhTlyi]
- 80. Comparative Analysis of Two Digital PCR Platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361875/]
- 81. Comparison and combination of mutation and methylation ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-024-00682-x]
- 82. Comparison of DNA methylation based classification ... [https://www.nature.com/articles/s41698-024-00718-3]
- 83. Real-World Technical Hurdles of ctDNA NGS Analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564474/]
- 84. Challenges and proposed solutions to the adoption of cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362566/]
- 85. Circulating tumor DNA to monitor treatment response in ... [https://www.nature.com/articles/s41698-025-00876-y]
- 86. Liquid clues: tracking early-stage breast cancer with ctDNA [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1634859/full]
- 87. Circulating tumour DNA assays in focus: highlights from ASCO ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12449440/]
- 88. Unleashing the potential of urine DNA methylation detection [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398378/]
- 89. Unleashing the power of urine-based biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11837902/]
- 90. Urine biomarkers can outperform serum ... [https://www.sciencedirect.com/science/article/pii/S2590280623000086]
- 91. Integrating analysis of multi-omics summary data identifies ... [https://link.springer.com/article/10.1007/s12672-025-02476-5]
- 92. Improvement of the sensitivity of circulating tumor DNA-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12332530/]
- 93. Decoding the Dynamics of Circulating Tumor DNA in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11240538/]
- 94. Strategies for improving detection of circulating tumor DNA ... [https://www.sciencedirect.com/science/article/pii/S0305737223000889]
- 95. Clinical applications of cell-free DNA-based liquid biopsy ... [https://www.sciencedirect.com/science/article/pii/S1936523325002505]
- 96. Cancer liquid biopsies by Oxford Nanopore Technologies ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02178-6]
- 97. Oxford Nanopore Technology and its Application in Liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10845067/]
- 98. Artificial Intelligence in cancer epigenomics: a review on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12166640/]
- 99. Machine learning approaches reveal methylation ... [https://www.nature.com/articles/s41598-025-99258-4]
- 100. Machine learning approach to DNA methylation and ... [https://www.sciencedirect.com/science/article/abs/pii/S0166432825003341]
- 101. Comparison of Different Machine Learning Methodologies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11729444/]
- 102. Machine learning in public health informatics [https://www.sciencedirect.com/science/article/abs/pii/S1047279724002886]
- 103. A predictive framework using advanced machine learning ... [https://www.nature.com/articles/s41598-025-00509-1]
- 104. Examining cellular heterogeneity in human DNA ... [https://www.sciencedirect.com/science/article/pii/S2666166725000449]
- 105. Comparison of WGBS, EPIC array, EM-seq, and Nanopore ... [https://ega-archive.org/studies/EGAS00001008014]
- 106. Practical Case Studies for Comparison Between EM-seq ... [https://www.cd-genomics.com/resource-em-seq-comparison-wgbs-pbat-case.html]
- 107. Bisulfite sequencing, but at what cost? [https://www.neb.com/en-us/nebinspired-blog/bisulfite-sequencing-but-at-what-cost?srsltid=AfmBOorpFIKxKUHScbeaC4WKznIyYnyf-gbkLozPCHhl1AgM598rI9ln]
- 108. Enabling whole-genome DNA methylation-based ... [https://www.medrxiv.org/content/10.1101/2025.09.18.25335800v1.full-text]
- 109. How nanopore sequencing works [https://nanoporetech.com/platform/technology]
- 110. Simultaneous sequencing of genetic and epigenetic bases ... [https://www.nature.com/articles/s41587-022-01652-0]
- 111. Nanopore sequencing technology, bioinformatics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8988251/]
- 112. Comparison of Illumina 450K and EPIC arrays in placental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6791701/]
- 113. Cost-effective solutions for high-throughput enzymatic DNA ... [https://journals.plos.org/plosgenetics/article?id=10.1371/journal.pgen.1011667]
- 114. Clinical validation of a multi-model blood cfDNA ... [https://www.sciencedirect.com/science/article/pii/S209012322500832X]
- 115. GRAIL PATHFINDER 2 Results Show Galleri® Multi ... [https://grail.com/press-releases/grail-pathfinder-2-results-show-galleri-multi-cancer-early-detection-blood-test-increased-cancer-detection-more-than-seven-fold-when-added-to-uspstf-a-and-b-recommended-screenings/]
- 116. Real-world data and clinical experience from over ... [https://www.nature.com/articles/s41467-025-64094-7]
- 117. A large-scale, multi-centre validation study of an AI ... [https://www.nature.com/articles/s41698-025-01105-2]
- 118. Evaluation of an innovative multi-cancer early detection test [https://pmc.ncbi.nlm.nih.gov/articles/PMC11922694/]
- 119. DNA methylation and machine learning - Clinical Epigenetics [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-025-01967-0]
- 120. Comparison of Methods for DNA Methylation Analysis [https://www.neb.com/en-us/tools-and-resources/selection-charts/dna-methylation-table?srsltid=AfmBOooZK2xfBvoAmly3UeEHi4WJ5YsCr2Q3eU5LcMcBovtGOvTjsugQ]
- 121. the potential of multi-cancer early detection (MCED) ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11785667/]
- 122. The performance of the SEPT9 gene methylation assay ... [https://www.nature.com/articles/s41598-017-03321-8]
- 123. Methylated Septin 9 as a Promising Biomarker in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9271001/]
- 124. Circulating tumor DNA for monitoring colorectal cancer [https://turkjsurg.com/articles/circulating-tumor-dna-for-monitoring-colorectal-cancer-a-prospective-observational-study-to-assess-the-presence-of-methylated-sept9-and-vim-promoter-genes-and-its-role-as-a-biomarker-in-colorectal-cancer-management/turkjsurg.2023.6038]
- 125. Press Releases [https://investors.guardanthealth.com/press-releases/press-releases/2025/Guardant-Health-Presents-Data-Demonstrating-Strong-Performance-of-Shield-Multi-Cancer-Detection-Test-Across-10-Tumor-Types/default.aspx]
- 126. FDA Grants Breakthrough Status to Shield Test [https://conexiant.com/internal-medicine/articles/fda-grants-breakthrough-status-to-shield-test/]
- 127. ctDNA methylation profiling reveals NBL1 as a promising ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12302688/]
- 128. Clinical and analytical validation of a combined RNA ... [https://www.nature.com/articles/s43856-025-00934-3]